Coronary revascularization is a crucial part of the treatment of acute coronary syndrome (ACS) due to its survival benefit.1 However, numerous studies have shown that between 30% and 60% of patients receive incomplete coronary revascularization (ICR), which is associated with worse cardiovascular prognosis.2 While some of the drugs available for treating angina have failed to show any change in cardiovascular prognosis, they have been shown to reduce the degree of angina and improve the patient's quality of life, making them widely used in clinical practice.3
Here we present a retrospective study conducted in all consecutive patients admitted with ACS over a 24-month period. ICR was defined as lesions > 70% remaining untreated in the main vessels or in the secondary branches with diameter > 1.5 mm2. The endpoints analyzed during the follow-up period were the addition of any antianginal drug and the cumulative incidence of cardiovascular complications (readmissions due to any cardiovascular cause and/or death due to cardiovascular cause). The antianginal drugs evaluated during the follow-up period were beta-blockers, dihydropyridine calcium-channel blockers, nitrates, ivabradine, and ranolazine. A multivariate analysis of the addition of antianginal drugs was carried out using a Cox regression model with hazard ratios; recurrent events were analyzed using negative binary logistic regression, with the IRR (incidence rate ratio), which has been postulated as a more precise way of analyzing the actual prognosis of cardiovascular disease.4
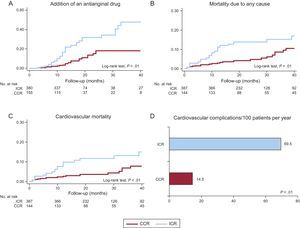
As shown in Table, 28.7% of the patients received ICR, and these patients had a higher mean age, prevalence of risk factors and comorbidities, as well as a higher score on the GRACE (Global Registry of Acute Coronary Events) scale. Patients with ICR received a lower number of stents, and the use of drug-eluting stents was less common. The most common reasons for receiving ICR were advanced age (28.8%), the presence of chronic occlusions (25.0%), renal failure (20.6%), and diffuse lesions (13.1%). Antianginal drugs (except beta-blockers) were more commonly recommended at discharge in patients with ICR, although they received less dual antiplatelet therapy. During the follow-up period (median, 19 months), mortality due to any cause was 10.6%, and mortality due to cardiovascular cause was 8.9%. An antianginal drug was added in 12.9% of the patients and, as shown in Figure, this was much more common in the patients with ICR (24.5% vs 7.1%; P < .01); mortality and recurrence of cardiovascular complications were also higher (Figure). The multivariate analysis (adjusted for age, sex, ACS type, risk factors, previous cardiovascular disease, GRACE score, and treatment at discharge) showed an independent association between the ICR and the addition of antianginal drugs (odds ratio, 2.62; 95% confidence interval, 1.34-5.14; P < .001) as well as with recurrent cardiovascular complications (IRR, 1.49; 95% confidence interval, 1.10-2.01; P = .01).
General Characteristics of the Original Cohort According to the Degree of Revascularization
| Total | ICR | CCR | P | |
|---|---|---|---|---|
| Patients | 557 (100.0) | 160 (28.7) | 397 (71.3) | |
| Age, y | 67.5 ± 13.0 | 72.5 ± 12.3 | 65.5 ± 12.8 | < .01 |
| Age > 75 y, % | 31.9 | 47.8 | 25.6 | .01 |
| Men, % | 73.8 | 77.4 | 72.7 | .25 |
| Diabetes mellitus, % | 30.0 | 37.1 | 26.6 | .01 |
| Hypertension, % | 65.4 | 74.8 | 61.3 | < .01 |
| Active smoker, % | 34.1 | 23.3 | 38.7 | .01 |
| Dyslipidemia, % | 49.6 | 56.6 | 46.6 | .03 |
| Previous HF, % | 2.7 | 6.9 | 0.8 | < .01 |
| Previous IHD, % | 22.6 | 38.4 | 16.2 | < .01 |
| Previous PTCA, % | 11.7 | 16.4 | 9.9 | .03 |
| Previous CABG, % | 3.8 | 8.2 | 1.8 | .01 |
| PAD, % | 5.0 | 11.3 | 2.5 | < .01 |
| AF, % | 7.7 | 10.1 | 6.6 | .16 |
| Previous stroke, % | 7.7 | 10.7 | 6.6 | .10 |
| COPD, % | 7.5 | 8.8 | 7.1 | .49 |
| STE-ACS, % | 37.5 | 23.9 | 43.3 | < .01 |
| GFR, 60 mL/min/1.72 m2 | 78.4 ± 25.3 | 72.5 ± 24.5 | 80.7 ± 25.2 | .01 |
| GFR < 60 mL/min/1.72 m2, % | 22.8 | 29.2 | 20.2 | .02 |
| GRACE score | 139.6 ± 41.0 | 149.4 ± 47.8 | 135.6 ± 37.3 | < .01 |
| GRACE score > 140, % | 46.9 | 48.8 | 46.1 | .32 |
| No. of diseased vessels | 1.7 ± 0.9 | 2.4 ± 0.8 | 1.4 ± 0.8 | < .01 |
| No. of treated vessels | 1.1 ± 0.6 | 0.9 ± 0.7 | 1.2 ± 0.6 | < .01 |
| Drug-eluting stents, % | 57.4 | 38.4 | 65.1 | < .01 |
| Bioabsorbable stents, % | 1.6 | 0.6 | 2.0 | .24 |
| Total No. of stents | 1.3 ± 1.1 | 1.0 ± 1.2 | 1.4 ± 1.0 | < .01 |
| No. of stents, % | 19.7 | 41.3 | 11.1 | < .01 |
| Charlson comorbidity index | 2.1 ± 2.0 | 2.6 ± 2.4 | 1.9 ± 1.8 | < .01 |
| Charlson comorbidity index ≥ 4, % | 16.0 | 23.9 | 12.9 | .01 |
| LVEF, % | 54.0 ± 12.2 | 50.8 ± 13.8 | 55.1 ± 11.3 | < .01 |
| Treatments at discharge, % | ||||
| Antiplatelet agents | 98.3 | 98.0 | 98.5 | .68 |
| Dual antiplatelet therapy | 82.8 | 72.8 | 88.3 | < .01 |
| Oral anticoagulants | 6.3 | 8.8 | 5.3 | .14 |
| Beta-blockers | 87.1 | 82.8 | 89.1 | .02 |
| Statins | 94.1 | 91.9 | 94.9 | .18 |
| ACE/ARB inhibitors | 80.4 | 83.8 | 79.2 | .23 |
| Calcium-channel blockers | 14.9 | 23.6 | 11.7 | .01 |
| Nitrates | 7.6 | 18.2 | 3.6 | < .01 |
| Ranolazine | 1.3 | 3.4 | 0.5 | .01 |
| Ivabradine | 1.7 | 4.7 | 0.5 | .01 |
ACE, angiotensin-converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft; CCR, complete coronary revascularization; COPD, chronic obstructive pulmonary disease; GFR, glomerular filtration rate; GRACE, Global Registry of Acute Coronary Events; HF, heart failure; ICR, incomplete coronary revascularization; IHD, ischemic heart disease; LVEF, left ventricular ejection fraction; PAD, peripheral artery disease; PTCA, percutaneous transluminal coronary angioplasty; STE-ACS, ST-segment elevation acute coronary syndrome.
Unless otherwise indicated, data are expressed as no. (%) or mean ± standard deviation.
The analysis of this cohort of patients with ACS reflects aspects of ICR that have not been widely studied to date. Coronary revascularization has become one of the pillars of ACS treatment, but ICR is a reality that generates a high-risk patient group in which medical treatment is highly relevant.5 The patients with ICR in this series received a lower number of stents and fewer drug-eluting stents, indicating that the percutaneous revascularization was less aggressive, both quantitatively and qualitatively. Some antianginal drugs are widely used in clinical practice due to the improvement observed in quality of life,3 despite the lack of evidence to support an improvement in prognosis. The patients with ICR in this series received more antianginal drugs at discharge, and others were added during the follow-up period. This is partly related to the treatment by the professionals involved in this phase, and may also be related to demand among patients who generally have more frequent angina, which impairs their quality of life to varying degrees.3
In conclusion, a significant percentage of patients with ACS undergo ICR, which is associated with an increased addition of antianginal drugs and the adjusted recurrence of cardiovascular complications during the follow-up period. The 2 priority objectives to be taken into account in the treatment of patients with ACS are maximum optimization of the degree of revascularization, and pharmacological treatment.
.