The cardiovascular benefits of the Mediterranean diet have usually been assessed under assumptions of ad libitum total energy intake (ie, no energy restriction). In the recently launched PREDIMED-Plus, we conducted exploratory analyses to study the baseline associations between adherence to an energy-restricted Mediterranean diet (MedDiet) and the prevalence of cardiovascular risk factors (CVRF).
MethodsCross-sectional assessment of all PREDIMED-Plus participants (6874 older adults with overweight/obesity and metabolic syndrome) at baseline. The participants were assessed by their usual primary care physicians to ascertain the prevalence of 4 CVRF (hypertension, obesity, diabetes, and dyslipidemia). A 17-point PREDIMED-Plus score was used to measure adherence to the MedDiet. Multivariable models were fitted to estimate differences in means and prevalence ratios for individual and clustered CVRF.
ResultsBetter adherence to a MedDiet pattern was significantly associated with lower average triglyceride levels, body mass index, and waist circumference. Compared with low adherence (≤ 7 points in the 17-point score), better adherence to the MedDiet (11-17 points) showed inverse associations with hypertension (prevalence ratio=0.97; 95%CI, 0.94-1.00) and obesity (prevalence ratio=0.96; 95%CI, 0.92-1.00), but positive associations with diabetes (prevalence ratio=1.19; 95%CI, 1.07-1.32). Compared with the lowest third of adherence, women in the upper third showed a significantly lower prevalence of the clustering of 3 or more CVRF (prevalence ratio=0.91; 95%CI, 0.83-0.98).
ConclusionsAmong participants at high cardiovascular risk, better adherence to a MedDiet showed significant inverse associations with CVRF among women, and improved lipid profiles and adiposity measures.
This trial was registered in 2014 at the International Standard Randomized Controlled Trial Registry (ISRCTN89898870).
Keywords
Hypertension, dyslipidemia, obesity, and diabetes have been consistently described as the most relevant metabolic cardiovascular risk factors (CVRF).1–3 The combination of more than 1 of these factors sharply increases the lifetime risk of cardiovascular disease (CVD).4 This combination was found with a higher frequency than expected only by chance.5 The lack of progress in reducing the prevalence of CVRF in the past few years6,7 has led to an alarming situation accounting for millions of deaths each year.8
The benefits of adhering to a Mediterranean dietary pattern for the prevention of CVD have been extensively documented.9–11 In the Lyon Diet Heart trial, an intervention in survivors of a myocardial infarction showed a pronounced reduction in CVD events compared with a control group.12 More recently, in the PREDIMED trial, an energy-unrestricted Mediterranean diet enriched with either extra-virgin olive oil or mixed nuts produced a 30% reduced risk of a first cardiovascular event in the intervention group compared with a control group, which was recommended a low-fat diet.13
However, these trials (as well as most observational studies) assessed only the effects of adherence to the Mediterranean diet without energy restriction (ie, total caloric intake was ad libitum). Within the framework of the PREDIMED-Plus, a trial designed to evaluate the long-term effectiveness of an intensive weight loss lifestyle intervention on primary cardiovascular prevention, we aimed to conduct exploratory analyses to examine the association of adherence to a score capturing an energy-restricted Mediterranean diet (MedDiet) with the prevalence of CVRF, including hypertension, diabetes, obesity, and dyslipidemia, alone or in combination.
METHODSWe conducted a cross-sectional assessment of all PREDIMED-Plus participants (6874 older adults with overweight/obesity and metabolic syndrome) at baseline. The PREDIMED-Plus is a 6-year, multicenter, parallel-group, randomized trial. The institutional review board of all participating institutions approved the study protocol, which followed the standards of the Declaration of Helsinki. The trial was registered in 2014 at the International Standard Randomized Controlled Trial Registry (ISRCTN89898870).
Participants and RecruitmentEligible participants were community-dwelling men and women aged 55 to 75 and 60 to 75 years, respectively, free from CVD at baseline, who were overweight or obese (body mass index [BMI] 27-40 kg/m2) and who met at least 3 criteria for the metabolic syndrome. We recruited 6874 participants from October 2013 to December 2016 in 23 Spanish centers.
Participants were randomly allocated in a 1:1 ratio to an intensive weight loss intervention group, based on a MedDiet (adapted to each participant's needs), physical activity promotion, and behavioral support, or a control group encouraged to adhere to an unrestricted-energy Mediterranean diet and receiving conventional health care. All participants provided written informed consent.
Dietary AssessmentA trained dietitian administered a 17-item questionnaire, a modified version of the previously validated questionnaire used in the PREDIMED trial,14 designed to assess adherence to the MedDiet. The 17-item questionnaire was scored with 1 point for each item capturing adherence to the MedDiet: a) use only extravirgin olive oil for cooking, salad dressings, and spreads; b) consume ≥ 3 fruit units (including natural fruit juices) per day; c) consume ≥ 2 servings (1 serving: 200 g, ≥ 1 portion raw or in a salad) of vegetables/garden produce per day; d) consume ≤ 1 servings (75 g) of white bread per day; e) consume ≥ 5 times per week whole grain cereals and pasta; f) consume ≤ 1 serving (100-150 g) of red meat, hamburgers, or meat products (eg, ham, sausage) per week; g) consume<1 serving (12 g) of butter, margarine, or cream per week; h) drink<1 sugary beverage or sugar-sweetened fruit juice per week; i) consume ≥ 3 servings (1 serving: 150 g) of legumes per week; j) consume ≥ 3 servings of fish or shellfish (1 serving: 100-150 g of fish or 200 g of shellfish) per week; k) consume<3 times per week commercial sweets or pastries (not homemade), such as cakes, cookies, sponge cake, or custard; l) consume ≥ 3 servings of nuts (1 servings: 30 g) per week; m) consume preferentially chicken, turkey, or rabbit instead of beef, pork hamburgers, or sausages; n) consume ≥ 2 times per week vegetables, pasta, rice, or other dishes seasoned with sofrito (sauce made with tomato and onion, leek or garlic and simmered in olive oil); o) add preferentially noncaloric artificial sweeteners to beverages (such as coffee or tea) instead of sugar; p) consume<3 times per week nonwhole grain pasta or white rice; q) drink 2-3 glasses (men) or 1-2 glasses (women) of wine per day (1 glass: 200 mL).
Although the 17-item questionnaire was not specifically validated, it is an adapted questionnaire based on a widely used and validated 14-item questionnaire.14 The 2 questionnaires share most items. However, the more stringent cutoff points in some items and the inclusion of a few additional items in the 17-item version attempt to better capture the potential caloric restriction that should be applied to a Mediterranean dietary pattern when there are goals for weight loss. Adherence to dietary habits reflecting a MedDiet was scored with 1 point, and with 0 points otherwise. Therefore, a score ranging from 0 to 17 points, with 0 meaning no adherence and 17 meaning maximum adherence, was developed. Subsequently, the score was categorized into approximate tertiles: low (≤ 7), medium (8-10), and high (11-17).
Measurements and OutcomesA general questionnaire was used to obtain information on sociodemographic variables, smoking status, medical conditions (diabetes), medication use, and family history of illness. Physical activity was measured using the validated Minnesota-REGICOR Short Physical Activity questionnaire.15
Anthropometric variables were measured by trained personnel according to the PREDIMED-Plus protocol. Weight and height were measured with high-quality electronic calibrated scales and a wall-mounted stadiometer, respectively. BMI was calculated by dividing the weight (kg) by height squared (m2). Obesity was defined as a BMI ≥ 30 kg/m2. Waist circumference was measured halfway between the last rib and the iliac crest by using an anthropometric tape. All anthropometric variables were determined in duplicate.
Blood pressure was measured in triplicate with a validated semiautomatic oscillometer (Omron HEM-705CP, the Netherlands) after 5minutes of rest while the participant was in a seated position. A participant was considered hypertensive if the average of the 3 measurements of systolic blood pressure was >135 mmHg or >85 mmHg for diastolic blood pressure, or if the participant was using antihypertensive drugs.
Blood samples were collected after an overnight fast and biochemical analyses were performed on fasting plasma glucose, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglyceride concentrations in local laboratories using standard enzymatic methods. A participant was considered diabetic by positive diagnosis of diabetes by a standard method,16 or if the participant reported taking medication for elevated glucose. Dyslipidemia was defined as either hypercholesterolemia (total cholesterol ≥ 240 mg/dL),17 or hypertriglyceridemia (total triglycerides ≥ 150 mg/dL), or low HDL-cholesterol (<40 mg/dL in men or<50 mg/dL in women).
We conducted additional analyses to evaluate the associations between adherence to the MedDiet and tobacco smoking.
Statistical AnalysisWe fitted logistic regression models and used a correction method18 to estimate prevalence ratios (PRs) in the 2017-12-13 PREDIMED-Plus dataset. Usually, odds ratios tend to be interpreted as if they estimated relative risks. However, due to the high prevalence of most CVRF in our study, the use of odds ratios, rather than PRs, would have exaggerated the magnitude of these associations if they had been mistakenly interpreted as relative risks. Therefore, to avoid any exaggeration of the true ratios of prevalence, we decided to correct the odds ratios and to transform them into PRs. The correction calculates the PR as the quotient between the odds ratio (OR) and a denominator comprising [(1-P0)+(P0*OR)] where P0 is the prevalence in the reference category. As dependent variables we used each of the 4 binary variables (hypertension, diabetes, obesity, and dyslipidemia), or 3 other binary variables representing the simultaneous presence of 2 or more, 3 or more, or 4 CVRF. To estimate adjusted differences in mean levels of CVRF (as continuous variables), we fitted linear regression models with adherence to the MedDiet (0-17 score, measured as a continuous variable) as the independent variable. Potential confounders included as covariates were smoking status (current, former, or never), family history of CVD (yes/no), total energy intake (kcal/d, continuous), physical activity (METs-min/wk, continuous), educational level (primary or less, secondary, or university), marital status (married, yes/no), living alone (yes/no), previous weight loss through dieting (yes/no), and center (categorized in quartiles by number of participants).
Tests of linear trends across categorical categories of adherence to the MedDiet were conducted, assigning the median value of each category, and considering them as continuous variables.
We tested for interactions between sex and adherence to the MedDiet with the likelihood ratio tests, in which full models, including interaction terms, were compared with reduced models without interaction terms. All P values lower than .05 were deemed as statistically significant. All statistical analyses were performed using STATA version 13.0 (StataCorp, College Station, TX, United States).
RESULTSThe participants’ baseline characteristics are shown in Table 1. The median adherence to the MedDiet in the full cohort was 8 points (range, 0-17). Participants with better adherence to the MedDiet were more likely to be women, to be more physically active, and to have previously followed a weight loss diet; they also showed lower PRs of obesity and dyslipidemia.
Baseline Characteristics According to Categories of Adherence to the Energy-restricted Mediterranean Diet Measured With the 17-item Score
| Baseline characteristics | Adherence to the energy-restricted Mediterranean diet | |||
|---|---|---|---|---|
| Low (≤ 7) | Medium (8-10) | High (11-17) | P | |
| No. | 2494 | 2789 | 1591 | — |
| Adherence to the Mediterranean diet | 5.7 ± 1.3 | 8.9 ± 0.8 | 12.1 ± 1.2 | <.001 |
| Hypertension, % | 86.3 | 86.0 | 84.4 | .219 |
| Diabetes, % | 26.1 | 30.7 | 29.2 | .001 |
| Obesity, % | 75.4 | 73.0 | 71.5 | .016 |
| Dyslipidemia, % | 92.3 | 90.2 | 91.0 | .025 |
| Age, y | 64.4 ± 5.1 | 65.1 ± 4.8 | 65.6 ± 4.7 | <.001 |
| Women, % | 40.5 | 50.7 | 57.3 | <.001 |
| Weight, kg | 88.4 ± 13.2 | 86.2 ± 13.0 | 84.5 ± 12.3 | <.001 |
| Waist circumference, cm | 108.9 ± 9.7 | 107.5 ± 9.8 | 105.8 ± 9.2 | <.001 |
| Waist-to-height ratio | 66.4 ± 5.6 | 66.3 ± 5.6 | 65.5 ± 5.4 | <.001 |
| Body mass index, kg/m2 | 32.7 ± 3.4 | 32.6 ± 3.5 | 32.2 ± 3.4 | <.001 |
| Smoking | <.001 | |||
| Current smoker, % | 45.4 | 36.5 | 18.1 | |
| Former smoker, % | 37.0 | 39.9 | 23.1 | |
| Highest educational level attained | <.001 | |||
| Primary school or less | 35.8 | 41.4 | 22.9 | |
| Complete secondary | 39.2 | 39.9 | 20.9 | |
| University | 33.6 | 39.8 | 26.6 | |
| Non-European origin, % | 3.5 | 2.0 | 1.9 | .001 |
| Willingness to change diet | 2.7 ± 0.5 | 2.7 ± 0.5 | 2.8 ± 0.4 | <.001 |
| Married, % | 76.6 | 77.0 | 73.9 | .057 |
| Living alone, % | 10.9 | 11.9 | 16.2 | <.001 |
| Retired, % | 52.9 | 56.6 | 58.4 | .001 |
| Self-reported previous depression, % | 19.9 | 20.8 | 22.1 | .241 |
| Family history of premature CHD, % | 15.9 | 16.5 | 18.6 | .071 |
| High blood cholesterol, % | 68.6 | 68.6 | 71.5 | .100 |
| Total cholesterol, mg/dL | 197.7 ± 38.8 | 196.3 ± 37.3 | 197.7 ± 36.8 | .344 |
| LDL-C, mg/dL | 122.7 ± 41.5 | 121.1 ± 41.9 | 122.9 ± 42.4 | .271 |
| HDL-C, mg/dL | 46.8 ± 11.7 | 48.4 ± 11.7 | 49.3 ± 12.1 | <.001 |
| Triglycerides, mg/dL | 160.0 ± 83.5 | 150.9 ± 74.8 | 144.6 ± 72.4 | <.001 |
| Fasting blood glucose, mg/dL | 112.7 ± 28.6 | 114.3 ± 29.2 | 113.1 ± 30.1 | .105 |
| Systolic blood pressure, mmHg | 139.3 ± 16.6 | 139.8 ± 17.0 | 139.3 ± 17.6 | .567 |
| Diastolic blood pressure, mmHg | 80.6 ± 10.3 | 81.0 ± 9.8 | 81.0 ± 9.6 | .336 |
| Leisure time physical activity, METS/min-wk | 2299 ± 2160 | 2635 ± 2332 | 2983 ± 2541 | <.001 |
| Chair test, 30 sec | 13.2 ± 5.5 | 13.2 ± 5.2 | 13.4 ± 4.9 | .418 |
| Total energy intake, kcal/d | 2522 ± 677 | 2360 ± 589 | 2312 ± 591 | <.001 |
| Fat intake, %E | 39.2 ± 6.4 | 39.5 ± 6.7 | 39.7 ± 6.5 | .030 |
| Carbohydrate intake, %E | 41.7 ± 6.7 | 40.8 ± 7.0 | 40.0 ± 6.6 | <.001 |
| Protein intake, %E | 15.8 ± 2.5 | 16.7 ± 2.8 | 17.4 ± 2.8 | <.001 |
| Dietary fiber intake, g/d | 23.5 ± 7.8 | 26.4 ± 8.7 | 30.5 ± 9.9 | <.001 |
| Alcohol intake, g/d | 12.3 ± 16.4 | 10.7 ± 15.1 | 10.2 ± 13.8 | <.001 |
| Previous weight loss dieting, % | 41.1 | 42.3 | 46.6 | .002 |
CHD, coronary heart disease; E, energy intake; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; MET, metabolic equivalent.
Unless otherwise indicated, data are presented as mean ± standard deviation.
Due to the study design, most CVRF were highly prevalent: 85.7% of participants were hypertensive, 73.5% were obese, and 91.1% had dyslipidemia. Only 28.7% had type-2 diabetes, also due to the study design. Most participants (over 90%) had at least 2 metabolic CVRF, 66% had 3 or more CVRF, and 18% had 4 of them.
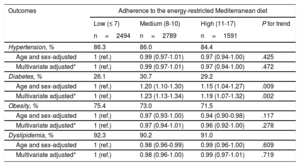
The group of participants with the highest adherence to the MedDiet (11-17 points) showed a marginally significant lower prevalence of hypertension (PR, 0.97; 95% confidence interval [95%CI], 0.94-1.00) and obesity (PR, 0.96; 95%CI, 0.92-1.00) compared with the group with the poorest adherence (≤ 7 points), although no significant linear trends across tertiles were found (P for trend .472 and .278, respectively). Unexpectedly, we found a positive significant association between better adherence to the MedDiet and the prevalence of type-2 diabetes (PR, 1.19; 95%CI, 1.07-1.32), with a significant linear trend (P for trend=.002) (Table 2).
Prevalence Ratios for Individual Cardiovascular Risk Factors According to Categories of Adherence to the Energy-restricted Mediterranean Diet Score
| Outcomes | Adherence to the energy-restricted Mediterranean diet | |||
|---|---|---|---|---|
| Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | |
| n=2494 | n=2789 | n=1591 | ||
| Hypertension, % | 86.3 | 86.0 | 84.4 | |
| Age and sex-adjusted | 1 (ref.) | 0.99 (0.97-1.01) | 0.97 (0.94-1.00) | .425 |
| Multivariate adjusted* | 1 (ref.) | 0.99 (0.97-1.01) | 0.97 (0.94-1.00) | .472 |
| Diabetes, % | 26.1 | 30.7 | 29.2 | |
| Age and sex-adjusted | 1 (ref.) | 1.20 (1.10-1.30) | 1.15 (1.04-1.27) | .009 |
| Multivariate adjusted* | 1 (ref.) | 1.23 (1.13-1.34) | 1.19 (1.07-1.32) | .002 |
| Obesity, % | 75.4 | 73.0 | 71.5 | |
| Age and sex-adjusted | 1 (ref.) | 0.97 (0.93-1.00) | 0.94 (0.90-0.98) | .117 |
| Multivariate adjusted* | 1 (ref.) | 0.97 (0.94-1.01) | 0.96 (0.92-1.00) | .278 |
| Dyslipidemia, % | 92.3 | 90.2 | 91.0 | |
| Age and sex-adjusted | 1 (ref.) | 0.98 (0.96-0.99) | 0.99 (0.96-1.00) | .609 |
| Multivariate adjusted* | 1 (ref.) | 0.98 (0.96-1.00) | 0.99 (0.97-1.01) | .719 |
Adjusted for sex, age (continuous), smoking (never smoked, current, former), family history of cardiovascular disease (yes/no), energy intake (continuous), physical activity (continuous), educational level (primary, secondary and university), married (yes/no), living alone (yes/no), previous weight loss dieting (yes/no), and node (recoded by number of participants).
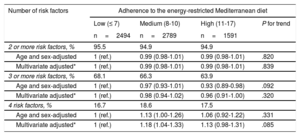
A marginally significant lower prevalence of clustered risk factors was found in participants with better adherence when we considered having 3 or more CVRF (PR, 0.96; 95%CI, 0.91-1.00). In contrast, better adherence to the MedDiet was associated with an increased prevalence, albeit nonsignificant, of having 4 CVRF (PR, 1.13; 95%CI, 0.98-1.31; Table 3, ). However, for a 1-point increment in adherence to the MedDiet, we found no significant differences in the number of CVRF (β=–0.001, 95%CI, –0.009 to+0.006; P=.750).
Prevalence Ratios for Clustered Cardiovascular Risk Factors (Hypertension, Diabetes, Obesity, and Dyslipidemia) According to Categories of Adherence to the Energy-restricted Mediterranean Diet Score
| Number of risk factors | Adherence to the energy-restricted Mediterranean diet | |||
|---|---|---|---|---|
| Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | |
| n=2494 | n=2789 | n=1591 | ||
| 2 or more risk factors, % | 95.5 | 94.9 | 94.9 | |
| Age and sex-adjusted | 1 (ref.) | 0.99 (0.98-1.01) | 0.99 (0.98-1.01) | .820 |
| Multivariate adjusted* | 1 (ref.) | 0.99 (0.98-1.01) | 0.99 (0.98-1.01) | .839 |
| 3 or more risk factors, % | 68.1 | 66.3 | 63.9 | |
| Age and sex-adjusted | 1 (ref.) | 0.97 (0.93-1.01) | 0.93 (0.89-0.98) | .092 |
| Multivariate adjusted* | 1 (ref.) | 0.98 (0.94-1.02) | 0.96 (0.91-1.00) | .320 |
| 4 risk factors, % | 16.7 | 18.6 | 17.5 | |
| Age and sex-adjusted | 1 (ref.) | 1.13 (1.00-1.26) | 1.06 (0.92-1.22) | .331 |
| Multivariate adjusted* | 1 (ref.) | 1.18 (1.04-1.33) | 1.13 (0.98-1.31) | .085 |
Adjusted for sex, age (continuous), smoking (never smoked, current, former), family history of cardiovascular disease (yes/no), energy intake (continuous), physical activity (continuous), educational level (primary, secondary and university), married (yes/no), living alone (yes/no), previous weight loss dieting (yes/no), and node (recoded by number of participants).
When we assessed the relationship between adherence to the MedDiet (as measured by the 17-item questionnaire) and smoking, better adherence to the 17-item questionnaire was significantly related to a lower prevalence of current smokers (PR, 0.95; 95%CI, 0.91-0.98; P for trend=.002). However, when we added smoking to the tally of clustered CVRF, we found no evidence of a significant inverse association between closer adherence to the MedDiet and the 4 clustered CVRF (PR, 0.99; 95%CI, 0.97-1.02) or all 5 clustered CVRF (PR, 0.97; 95%CI, 0.88-1.04) ().
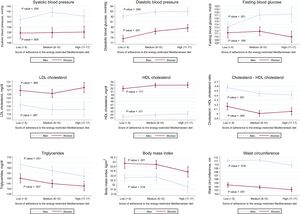
When we fitted linear regression models (adjusted for the potential aforementioned confounders), participants with better adherence to a MedDiet showed significantly lower average triglyceride levels (adjusted difference for an additional point in adherence (β=–1.61mg/dL; 95%CI,–2.34 to –0.88; P<.001), a lower total cholesterol to high-density lipoprotein cholesterol ratio (β=–0.02; 95%CI, –0.03 to –0.01; P<.001), lower BMI (β=–0.07kg/m2; 95%CI, –0.10 to –0.04; P <.001) and lower waist circumference (β=–0.18cm; 95%CI, –0.26 to –0.10; P <.001). In similar comparisons, we found for a 1-point increment of adherence significantly higher high-density lipoprotein cholesterol levels (β=+0.15mg/dL; 95%CI, +0.05 to +0.26; P=.004), and, unexpectedly, higher diastolic blood pressure (β=+0.24mmHg; 95%CI,+0.15 to+0.33; P <.001) and higher fasting blood glucose (β=+0.28mg/dL; 95%CI, 0.00 to+0.55; P=.048). No significant differences were found for systolic blood pressure (β=+0.04mmHg; 95%CI, –0.12 to+0.20; P=.619) (Figure 1).
Adjusted average levels of cardiovascular risk factors according to categories of adherence to the energy-restricted Mediterranean diet score. Linear regression models adjusted for age, sex (continuous), smoking (never smoked, current, former), family history of cardiovascular disease (yes/no), energy intake (continuous), physical activity (continuous), educational level (primary, secondary and university), married (yes/no), living alone (yes/no), previous weight loss dieting (yes/no), and node (recoded by number of participants). HDL, high-density lipoprotein; LDL, low-density lipoprotein.
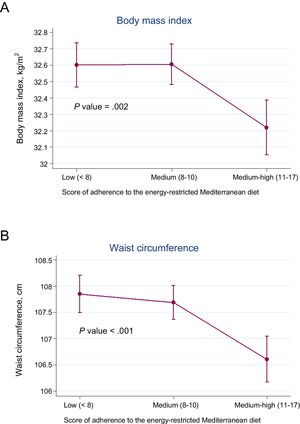
In addition, when we examined the associations between adherence to the MedDiet and BMI and waist circumference, we found strongly significant inverse linear trends across quartiles of adherence (P for trend .002 and <.001, respectively) (Figure 2). Furthermore, the best adherence (11-17 points) compared with the worst adherence (≤ 7 points) was significantly associated with a 17% reduced prevalence of waist-to-height ratio ≥ 0.7 (PR, 0.83; 95%CI, 0.72-0.95) ().
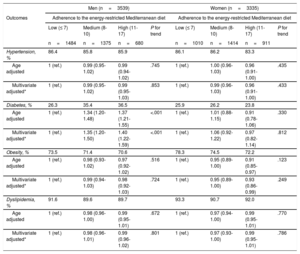
We noted a significant interaction (P for interaction <.001) between sex and adherence to the MedDiet regarding the prevalence of diabetes. Consequently, stratified analyses were conducted. We found a higher prevalence of diabetes among men who showed better adherence to the MedDiet (PR, 1.40; 95%CI, 1.22-1.59), with a significant positive linear trend (P for trend <.001). Contrarily, a lower prevalence of both hypertension (PR, 0.96; 95%CI, 0.91-1.00) and obesity (PR, 0.93; 95%CI, 0.86-0.99) were present, as well as a lower prevalence of diabetes, only among women, in the highest vs the lowest category of the MedDiet, although these differences did not reach statistical significance (PR, 0.97; 95%CI, 0.82-1.14). No interactions were found between sex and adherence to the MedDiet regarding the prevalence of hypertension or obesity (P for interaction .340 and .433, respectively) (Table 4).
Prevalence Ratios Stratified by Sex for Individual Cardiovascular Risk Factors According to Categories of Adherence to the Energy-restricted Mediterranean Diet Score
| Men (n=3539) | Women (n=3335) | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | Adherence to the energy-restricted Mediterranean diet | Adherence to the energy-restricted Mediterranean diet | ||||||
| Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | |
| n=1484 | n=1375 | n=680 | n=1010 | n=1414 | n=911 | |||
| Hypertension, % | 86.4 | 85.8 | 85.9 | 86.1 | 86.2 | 83.3 | ||
| Age adjusted | 1 (ref.) | 0.99 (0.95-1.02) | 0.99 (0.94-1.02) | .745 | 1 (ref.) | 1.00 (0.96-1.03) | 0.96 (0.91-1.00) | .435 |
| Multivariate adjusted* | 1 (ref.) | 0.99 (0.95-1.02) | 0.99 (0.95-1.03) | .853 | 1 (ref.) | 0.99 (0.96-1.03) | 0.96 (0.91-1.00) | .433 |
| Diabetes, % | 26.3 | 35.4 | 36.5 | 25.9 | 26.2 | 23.8 | ||
| Age adjusted | 1 (ref.) | 1.34 (1.20-1.48) | 1.37 (1.21-1.55) | <.001 | 1 (ref.) | 1.01 (0.88-1.15) | 0.91 (0.78-1.06) | .330 |
| Multivariate adjusted* | 1 (ref.) | 1.35 (1.20-1.50) | 1.40 (1.22-1.59) | <.001 | 1 (ref.) | 1.06 (0.92-1.22) | 0.97 (0.82-1.14) | .812 |
| Obesity, % | 73.5 | 71.4 | 70.6 | 78.3 | 74.5 | 72.2 | ||
| Age adjusted | 1 (ref.) | 0.98 (0.93-1.02) | 0.97 (0.92-1.02) | .516 | 1 (ref.) | 0.95 (0.89-1.00) | 0.91 (0.85-0.97) | .123 |
| Multivariate adjusted* | 1 (ref.) | 0.99 (0.94-1.03) | 0.98 (0.92-1.03) | .724 | 1 (ref.) | 0.95 (0.89-1.00) | 0.93 (0.86-0.99) | .249 |
| Dyslipidemia, % | 91.6 | 89.6 | 89.7 | 93.3 | 90.7 | 92.0 | ||
| Age adjusted | 1 (ref.) | 0.98 (0.96-1.00) | 0.99 (0.95-1.01) | .672 | 1 (ref.) | 0.97 (0.94-1.00) | 0.99 (0.95-1.01) | .770 |
| Multivariate adjusted* | 1 (ref.) | 0.98 (0.96-1.01) | 0.99 (0.96-1.02) | .801 | 1 (ref.) | 0.97 (0.93-1.00) | 0.99 (0.95-1.01) | .786 |
Adjusted for age (continuous), smoking (never smoked, current, former), family history of cardiovascular disease (yes/no), energy intake (continuous), physical activity (continuous), educational level (primary, secondary and university), married (yes/no), living alone (yes/no), previous weight loss dieting (yes/no), and node (recoded by number of participants).
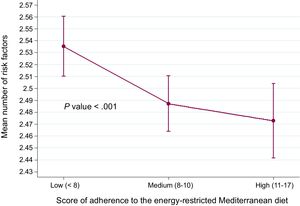
The mean number of CVRF across categories of adherence to the MedDiet was lower in women who showed better adherence to the MedDiet, with a significant interaction for sex (P for interaction=.002), and we observed an increasing trend in the mean number of CVRF across categories of adherence among men ().
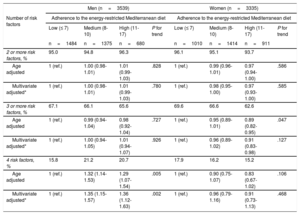
Significant inverse associations were found only among women who showed the greatest adherence to the MedDiet (11-17 points) compared with the poorest adherence (≤ 7 points) for the clustering of at least 2 CVRF (PR, 0.97; 95%CI, 0.93-1.00), and for at least 3 CVRF (PR, 0.91; 95%CI, 0.83-0.98), whereas a positive and significant increased prevalence for the clustering of all CVRF was observed among men (PR, 1.36; 95%CI, 1.12-1.63), with a significant linear trend (P for trend=.002) (Table 5).
Prevalence Ratios Stratified by Sex for Clustered Cardiovascular Risk Factors (Hypertension, Diabetes, Obesity, and Dyslipidemia) According to Categories of Adherence to the Energy-restricted Mediterranean Diet Score
| Men (n=3539) | Women (n=3335) | |||||||
|---|---|---|---|---|---|---|---|---|
| Number of risk factors | Adherence to the energy-restricted Mediterranean diet | Adherence to the energy-restricted Mediterranean diet | ||||||
| Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | Low (≤ 7) | Medium (8-10) | High (11-17) | P for trend | |
| n=1484 | n=1375 | n=680 | n=1010 | n=1414 | n=911 | |||
| 2 or more risk factors, % | 95.0 | 94.8 | 96.3 | 96.1 | 95.1 | 93.7 | ||
| Age adjusted | 1 (ref.) | 1.00 (0.98-1.01) | 1.01 (0.99-1.03) | .828 | 1 (ref.) | 0.99 (0.96-1.01) | 0.97 (0.94-1.00) | .586 |
| Multivariate adjusted* | 1 (ref.) | 1.00 (0.98-1.01) | 1.01 (0.99-1.03) | .780 | 1 (ref.) | 0.98 (0.95-1.00) | 0.97 (0.93-1.00) | .585 |
| 3 or more risk factors, % | 67.1 | 66.1 | 65.6 | 69.6 | 66.6 | 62.6 | ||
| Age adjusted | 1 (ref.) | 0.99 (0.94-1.04) | 0.98 (0.92-1.04) | .727 | 1 (ref.) | 0.95 (0.89-1.01) | 0.89 (0.82-0.95) | .047 |
| Multivariate adjusted* | 1 (ref.) | 1.00 (0.94-1.05) | 1.01 (0.94-1.07) | .926 | 1 (ref.) | 0.96 (0.89-1.02) | 0.91 (0.83-0.98) | .127 |
| 4 risk factors, % | 15.8 | 21.2 | 20.7 | 17.9 | 16.2 | 15.2 | ||
| Age adjusted | 1 (ref.) | 1.32 (1.14-1.53) | 1.29 (1.07-1.54) | .005 | 1 (ref.) | 0.90 (0.75-1.07) | 0.83 (0.67-1.02) | .106 |
| Multivariate adjusted* | 1 (ref.) | 1.35 (1.15-1.57) | 1.36 (1.12-1.63) | .002 | 1 (ref.) | 0.96 (0.79-1.16) | 0.91 (0.73-1.13) | .468 |
Adjusted for age (continuous), smoking (never smoked, current, former), family history of cardiovascular disease (yes/no), energy intake (continuous), physical activity (continuous), educational level (primary, secondary and university), married (yes/no), living alone (yes/no), previous weight loss dieting (yes/no), and node (recoded by number of participants).
To address the reverse causality bias by known baseline diabetes status that could have led the participants to adopt better food habits, we conducted an additional analysis excluding diabetes from the CVRF count (but adjusting for diabetes). An inverse association was found for the clustering of at least 2 CVRF (PR, 0.98; 95%CI, 0.95-0.99) in the whole sample (men and women), which was also apparent for having at least 3 CVRF (PR, 0.92; 95%CI, 0.87-0.98; Figure 3, ). We also found that for each additional point of adherence to the MedDiet, a significantly lower number of CVRF were present (β=–0.011; 95%CI, –0.017 to –0.005; P <.001).
Additionally, when we included smoking in the tally of CVRF (hypertension, obesity, dyslipidemia, smoking), higher adherence to the MedDiet was associated with a lower prevalence of the 4 CVRF (PR, 0.93; 95%CI, 0.87-0.98; P for trend=.001; ).
DISCUSSIONIn the present baseline assessment of the PREDIMED-Plus trial conducted in older participants with overweight or obesity and metabolic syndrome living in a Mediterranean country, we found evidence that higher baseline adherence to a MedDiet exhibited inverse associations with several individual or clustered CVRF among women, within the framework of the PREDIMED-Plus trial, but not with diabetes.
Better adherence to the MedDiet was significantly associated with a lower prevalence of hypertension, but paradoxically it was associated with higher average diastolic blood pressure and no significant differences in average systolic blood pressure. These findings contrast with previous intervention trials encouraging adherence to the MedDiet that found substantial benefits in terms of blood pressure and hypertension.19–21 However, we report only cross-sectional findings and therefore further longitudinal assessments seem necessary to reassess the relationship between blood pressure and adherence to the MedDiet.
An inverse cross-sectional association of the Mediterranean diet with obesity has previously been reported by Martínez-González et al.,22 but that assessment was conducted in the framework of the 14-item tool used in the PREDIMED trial, and this latter tool did not include any energy restriction. Our present findings showed that better adherence to the MedDiet was associated with a reduced prevalence of obesity, and a lower average BMI and waist circumference. The beneficial effect of the MedDiet on weight loss has previously been shown in the weight loss DIRECT trial, conducted in a younger mostly male population with overweight or obesity, wherein a calorie-restricted Mediterranean diet emerged as a feasible dietary pattern for achieving significant weight loss, over low-fat and low-carbohydrate diets.23,24 We observed a significant inverse association between better adherence to the MedDiet and obesity among women only. In the past few years, the prevalence of obesity among older Spanish women has increased.25 Therefore, these findings are relevant in order to propose a feasible intervention to address obesity in this group.
Consistent evidence has accumulated on the beneficial effect of the Mediterranean diet on diabetes. In the PREDIMED trial, we found a strong reduction in diabetes risk in the Mediterranean diet enriched with extra-virgin olive oil group compared with the control group.26 In addition, a recent meta-analysis including clinical trials and prospective studies suggested a 19% decreased risk of type-2 diabetes with greater adherence to the Mediterranean diet.27 Contrarily, we found in our present study a positive significant association between adherence to the MedDiet and the prevalence of diabetes, and we noted a significant interaction between sex and adherence to the MedDiet in the prevalence of diabetes. In our cross-sectional analysis, and taking into account the extensive media coverage of the good results of Mediterranean diet interventions in diabetic patients after the PREDIMED trial, these findings may suggest the existence of reverse causality bias. Participants with diabetes, because they were aware of their diabetic status, might have increased their adherence to the MedDiet as a consequence of their knowledge or because they might have received medical advice promoting both energy restriction and increased adherence to the MedDiet. In line with this hypothesis, participants who were recently diagnosed (less than 1 year) with diabetes, showed better adherence to the MedDiet than those with a longer-standing diagnosis or who were not diabetic (data not shown).
Despite the lack of significant associations between the highest adherence to the MedDiet and dyslipidemia, we observed significant improvements in triglyceride levels across tertiles of adherence, as well as a significant beneficial association with higher HDL-cholesterol levels. These results are partially in agreement with previous findings, including those of the PREDIMED trial,28 and other Spanish prospective cohort studies.29
When we examined the effects of better adherence to the MedDiet on clustered CVRF, the inverse association was apparent only among women, with a decreased prevalence of clustered CVRF, consistent with the findings of other studies.30,31 In another Spanish cohort, better adherence to the Mediterranean diet was also longitudinally inversely associated with CVD. Participants with higher scores on a 10-point healthy lifestyle score (7-10 points compared with 0-3 points), which included baseline adherence to a traditional Mediterranean diet, showed a subsequent significant reduction in the risk of hard cardiovascular events.32 Improvements in CVRF observed in women but not in men could be due to greater health self-awareness and motivation in women.33 In addition, older women included in this trial are likely to be preferentially responsible for food purchasing and preparing meals and might show a greater predisposition to adopting healthy dietary habits.
LimitationsA major limitation of our study is the potential reverse causation bias, inherent to the cross-sectional design, which we fully acknowledge. However, as PREDIMED-Plus represents an unprecedented large trial, unique in Europe, aiming to assess the effect of a MedDiet, weight loss, and physical activity on hard cardiovascular events, it seems important to present the cross-sectional associations between the principal tool for our intervention (the 17-item score of adherence to a MedDiet) and CVRF (or their clustering) at baseline. Other limitations are the lack of generalizability of our findings to younger ages or healthier populations, given the age range and baseline conditions of our participants, and the existence of a potential misclassification bias due to self-reported dietary information that may bias the results toward the null. In addition, the inclusion of obesity as a risk factor in a population of overweight/obese participants might lead to bias, and limit the generalizability of the results.
CONCLUSIONSIn conclusion, better adherence to a MedDiet showed evidence of a beneficial association with the prevalence of most classic metabolic CVRF among women, and improved lipid profile and anthropometric measures in this cross-sectional assessment of the baseline characteristics of older, overweight, or obese PREDIMED-Plus participants. However, it is important to conduct future large longitudinal assessments of the long-term effects of the intervention in the PREDIMED-Plus trial on changes in CVRF, including the incidence of new cases of type 2 diabetes among participants who were not initially diabetic. These studies will provide the best answers to the causal relationship between adherence to a MedDiet and CVRF.
FUNDINGThis work is supported by the European Research Council [Advanced Research Grant 2014 to 2019; agreement #340918 granted to MAM-G], and the Spanish Government Official Agency for funding biomedical research - Instituto de Salud Carlos III (ISCIII) with competitive grants for the periods 2014 to 2016, 2015 to 2017, 2017 to 2019 and 2018 to 2020, through the Fondo de Investigación para la Salud (FIS), which is cofunded by the European Regional Development Fund [grants: PI13/00673, PI13/00492, PI13/00272, PI13/01123, PI13/00462, PI13/00233, PI13/02184, PI13/00728, PI13/01090, PI13/01056, PI14/01722, PI14/00636, PI14/00618, PI14/00696, PI14/01206, PI14/01919, PI14/00853, PI14/01374, PI16/00473, PI16/00662, PI16/01873, PI16/01094, PI16/00501, PI16/00533, PI16/00381, PI16/00366, PI16/01522, PI16/01120, PI17/00764, PI17/01183, PI17/00855, PI17/01347, PI17/00525, PI17/01827, PI17/00532, PI17/00215, PI17/01441, PI17/00508, PI17/01732, PI17/00926]. Additional grants: Acciones Especiales from ISCIIII, Consejería de Salud, Junta de Andalucía [PI0458/2013, PS0358/2016], Recercaixa-grant 2013 [2013ACUP00194], a SEMERGEN grant, Generalitat Valenciana PROMETEO [grant 17/2017] and International Nut & Dried Fruit Council – FESNAD [No. 201302]. Fundación Patrimonio Comunal Olivarero is providing the necessary amounts of olive oil. Nuts were initially and only partially provided by Pistachios Growers and Almond Board of California. None of these funding sources played any role in the design, collection, analysis, or interpretation of the data or in the decision to submit manuscripts for publication.
CONFLICTS OF INTERESTE. Ros is a consultant for the California Walnut Commission. J. Salas-Salvadó is an unpaid member of the Scientific Advisory Board of the International Nut and Dried Fruit Foundation and received research grants through his research institution. The other authors report no conflicts of interests.
- –
CVD is still a major public health burden and a leading cause of death and health loss. There is consistent evidence of the cardiovascular benefits of adherence to the Mediterranean diet under assumptions of ad libitum total energy intake (ie, without energy restriction). However, there is a lack of studies evaluating the role of an energy-restricted Mediterranean diet on cardiovascular health.
- –
Better adherence to a MedDiet was inversely associated with individual and clustered CVRF among women, and with improved lipid profile and anthropometric measures.
The authors gratefully acknowledge other members of the PREDIMED-Plus group.
Supplementary data associated with this article can be found in the online version, at http://doi.org/10.1016/j.rec.2018.08.010.