To assess the structure of health care delivery and the clinical characteristics of adults with congenital heart disease (ACHD) attending specialized centers in Spain.
MethodsA survey was conducted among 32 Spanish centers in 2014. The centers were classified into 2 levels based on their resources. In 2017, a clinical dataset was collected of all consecutive patients attended for a 2-month period at these centers.
ResultsA total of 31 centers (97%) completed the survey. Seven centers without specialized ACHD clinics were excluded from the analysis. In 2005, only 5 centers met the requirements for specific care. In 2014, there were 10 level 1 and 14 level 2 centers, with a total of 19 373 patients under follow-up. Health care structure was complete in most centers but only 33% had ACHD nurse specialists on staff and 29% had structured transition programs. Therapeutic procedures accounted for 99% and 91% of those reported by National Registries of Cardiac Surgery and Cardiac Catheterization, respectively. Among attended patients, 48% had moderately complex lesions and 24% had highly complex lesions. Although 46% of patients attending level 2 centers had simple lesions, 17% had complex lesions.
ConclusionsThe structure for ACHD health care delivery in Spain complies with international recommendations and is similar to that of other developed countries. Congenital heart diseases under specialized care consist mostly of moderately and highly complex lesions, even in level 2 centers. It would be desirable to reorganize patient follow-up according to international recommendations in clinical practice.
Keywords
Current advances in pediatric cardiovascular treatment and socioeconomic circumstances have contributed to around 90% of newborns with congenital heart disease (CHD) surviving until adulthood.1,2 In Western countries, the prevalence of CHD in adults (ACHD) is already higher than that of CHD in children and is continuing to increase.3,4 However, the development of the health care structure to serve this emerging cardiovascular population has not followed a similar path to that of the child population. Pediatric cardiology emerged as a specific discipline in the 1960s. After a few years, pediatric cardiology and cardiac surgery were formalized and organized within national professional societies.5 Although pediatric cardiology and cardiovascular surgery are not yet recognized as medical specialties in Spain, their structure, organization, and efficiency are similar to those of other developed countries.6 Although the first ACHD clinic was established in 1959 in Toronto (Canada) and the first specialized center in Europe was founded in 1964 in the UK, in most western countries specialized ACHD centers were not developed until the 1990s. However, these centers were created with some reluctance, were always provided with fewer resources, and had a much lower priority than the pediatric cardiology services created 20 or 30 years ago.7 Several countries with a long history of treating ACHD have created national networks to promote adult follow-up and have developed models based on specialized multidisciplinary care teams.8,9 Recently, a panel of experts from the Working Group on Adult Congenital Heart Disease of the European Society of Cardiology has proposed criteria to standardize centers and recommended standards for staffing and services.10 However, in Spain, there has been no analysis of the development and adherence to international guidelines of the care structure or clinical characteristics of patients under follow-up. This study reports on the activity, strengths, and weaknesses of the development of this emerging subspecialty in Spain.
METHODSIn 2014, a survey on the ACHD health care structure was prepared and sent to all centers with known activity. The regional centers with recognized development in this subspecialty were contacted and invited to participate in a multicenter study. Each of these centers identified the collaborating or associated centers in their region. The survey was sent to a total of 32 centers within the Spanish public health care network.
A center was considered to deliver ACHD health care if it offered specialized consultations conducted by one or more dedicated or semi-dedicated cardiologists (). The following criteria were established to determine which centers could be considered as level 110: a) tertiary hospital with all medical and surgical specialties; b) pediatric cardiology service or section; c) specific diagnostic techniques, including echocardiography, ergospirometry, cardio magnetic resonance, computed tomography, electrophysiology, and cardiac catheterization performed by experienced specialists; d) specialized personnel, including at least 2 dedicated or semi-dedicated cardiologists (adult or pediatric), at least 2 cardiac catheterization specialists with experience in therapeutic procedures, and at least 1 electrophysiologist with experience in arrhythmia ablation in ACHD; and e) a multidisciplinary structure with related services and clinics, including its own transplant program in ACHD or a shared program. Centers with ACHD health care that did not meet any of these characteristics were considered as level 2. The stratified data were compared by level. The number of therapeutic procedures per year was compared with that of the Spanish registry of surgical interventions in adults with CHD in the same year published by the Spanish Society of Thoracic-Cardiovascular Surgery11 and with that of the Official Report of the Working Group on Cardiac Catheterization and Interventional Cardiology of the Spanish Society of Cardiology.12
To obtain a representative sample of the attended population, in 2017 all centers that had declared having at least 1 specialized clinic were invited to participate in a cross-sectional registry that included all consecutive patients attended for a 2-month period in these clinics (May to June, 2017). This registry included demographic data, specific diagnosis, and the level of complexity of CHD13 (), previous interventions (), clinical data, arrhythmias detected, and main findings of the diagnostic tests performed. The data obtained from this sample have been used as a control group to construct a sudden death risk model that is in the process of publication. Data were analyzed at the coordinating center and demographic data were used to avoid duplication. The study complied with the Declaration of Helsinki and was approved by the ethics committee of the coordinating hospital. Informed consent was not required due to the observational nature of the study and because all the analyzed data were anonymized.
All data were analyzed using the IBM SPSS Statistics V22.0 software package (IBM, 2013, USA). Qualitative variables were expressed as percentages and compared using the chi-squared χ test or Fisher exact test. The Kolmogorov-Smirnov test showed that the vast majority of quantitative variables were not normally distributed, therefore they were always expressed as median [interquartile range] and compared using the Mann-Whitney U test. A P value of <.05 was used as a cutoff for statistical significance.
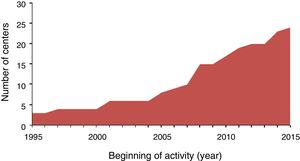
RESULTSA total of 31 centers (97%) out of the 32 centers completed the survey. Seven centers without specialized ACHD clinics were excluded from the analysis and 24 centers participated in the survey. There were 6 centers in Andalusia, 4 in Catalonia, 4 in the Community of Madrid, 3 in Galicia, 3 in the Valencian Community, 1 in the Chartered Community of Navarre, 1 in Aragon, 1 in the Balearic Islands, and 1 in the Canary Islands. There were no centers in the other autonomous communities (figure 1). Of the 24 centers, 9 have been recognized as Centers, Services and Refererral Units (CSURs) by the Spanish National Health System. Figure 2 shows the year in which ACHD health care was initiated in the 24 centers. In 2005, only 5 centers met the requirements for specific care. After this year, there was a steady increase in their number.
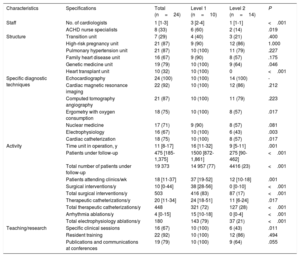
In total, 23 centers (96%) were integrated within the adult cardiology service, but 8 (33%) counted on the participation of pediatric cardiologists. Table 1 shows the main strengths and weaknesses of the centers and comparisons between them stratified by level. Almost all centers had similar numbers of specialized units; there were no significant differences between centers except in the case of genetics and heart transplant units. Level 1 centers had more clinical cardiologists and more ACHD nurse specialists on staff, but two-thirds of centers and 40% of level 1 centers had no dedicated nursing support. In addition, less than 30% of the centers and only 40% of level 1 centers had structured transition programs. Most centers performed echocardiography and advanced radiologic imaging procedures in ACHD, but only 57% of level 2 centers had ergospirometry units, 43% had electrophysiology units, and 57% had cardiac catheterization units.
Structure and activity. Comparison between level 1 and level 2 centers
| Characteristics | Specifications | Total (n=24) | Level 1 (n=10) | Level 2 (n=14) | P |
|---|---|---|---|---|---|
| Staff | No. of cardiologists | 1 [1-3] | 3 [2-4] | 1 [1-1] | <.001 |
| ACHD nurse specialists | 8 (33) | 6 (60) | 2 (14) | .019 | |
| Structure | Transition unit | 7 (29) | 4 (40) | 3 (21) | .400 |
| High-risk pregnancy unit | 21 (87) | 9 (90) | 12 (86) | 1.000 | |
| Pulmonary hypertension unit | 21 (87) | 10 (100) | 11 (79) | .227 | |
| Family heart disease unit | 16 (67) | 9 (90) | 8 (57) | .175 | |
| Genetic medicine unit | 19 (79) | 10 (100) | 9 (64) | .046 | |
| Heart transplant unit | 10 (32) | 10 (100) | 0 | <.001 | |
| Specific diagnostic techniques | Echocardiography | 24 (100) | 10 (100) | 14 (100) | - |
| Cardiac magnetic resonance imaging | 22 (92) | 10 (100) | 12 (86) | .212 | |
| Computed tomography angiography | 21 (87) | 10 (100) | 11 (79) | .223 | |
| Ergometry with oxygen consumption | 18 (75) | 10 (100) | 8 (57) | .017 | |
| Nuclear medicine | 17 (71) | 9 (90) | 8 (57) | .081 | |
| Electrophysiology | 16 (67) | 10 (100) | 6 (43) | .003 | |
| Cardiac catheterization | 18 (75) | 10 (100) | 8 (57) | .017 | |
| Activity | Time unit in operation, y | 11 [8-17] | 16 [11-32] | 9 [5-11] | .001 |
| Patients under follow-up | 475 [185-1,375] | 1500 [872-1,861] | 275 [90-462] | <.001 | |
| Total number of patients under follow-up | 19 373 | 14 957 (77) | 4416 (23) | <.001 | |
| Patients attending clinics/wk | 18 [11-37] | 37 [19-52] | 12 [10-18] | .001 | |
| Surgical interventions/y | 10 [0-44] | 38 [28-56] | 0 [0-10] | <.001 | |
| Total surgical interventions/y | 503 | 416 (83) | 87 (17) | <.001 | |
| Therapeutic catheterizations/y | 20 [11-34] | 24 [18-51] | 11 [6-24] | .017 | |
| Total therapeutic catheterizations/y | 448 | 321 (72) | 127 (28) | <.001 | |
| Arrhythmia ablations/y | 4 [0-15] | 15 [10-18] | 0 [0-4] | <.001 | |
| Total electrophysiology ablations/y | 180 | 143 (79) | 37 (21) | <.001 | |
| Teaching/research | Specific clinical sessions | 16 (67) | 10 (100) | 6 (43) | .011 |
| Resident training | 22 (92) | 10 (100) | 12 (86) | .494 | |
| Publications and communications at conferences | 19 (79) | 10 (100) | 9 (64) | .055 |
Values expressed as No. (%) or median [interquartile range].
The units had been active for a median period of 11 [8-17] years; the median was significantly higher in level 1 centers. There was a total of 19 373 patients under follow-up. Level 1 and level 2 centers had a median of 1500 patients and 275 patients under follow-up (P <.001), respectively. In 2013, there were 503 surgical interventions, 448 therapeutic cardiac catheterizations, and 180 arrhythmia ablations in ACHD (83%, 72%, and 79% in level 1 centers, respectively). These figures account for 99% and 91% of the surgical interventions and therapeutic cardiac catheterizations in adults with CHD reported by the Spanish Society of Cardiology and the Spanish Society for Thoracic and Cardiovascular Surgery in the same year, respectively.
Teaching and researchAll level 1 centers and 43% of level 2 centers conducted specific multidisciplinary clinical sessions. In total, 92% of the centers participated in the training of cardiology or pediatric cardiology residents and 79% had published articles or presented communications at conferences on ACHD. Two centers have members in the Working Group on Adult Congenital Heart Disease,14 2 have participated in consensus documents,15,16 and 1 has participated in the development of the European Society of Cardiology clinical practice guidelines for the management of ACHD.17
Register of specific congenital heart diseasesOf the 24 centers, 18 (75%) participated in the registration of specific ACHDs seen in an outpatient clinic for a 2-month period. Seven level 1 centers (70%) and 11 level 2 (79%) participated in the registry. In total, 2289 patients (50% male) were included. Median age was 35 [25-45] years. There were no differences in age or sex between the 2 types of center, but age at diagnosis was significantly lower in level 1 centers (table 2). Of the patients, 32% had simple lesions, 44% had moderately complex lesions, and 24% had highly complex lesions. There were significant differences in the distribution of the level of complexity: only 27% of the patients attended in level 1 centers had simple lesions, whereas 46% attended in level 2 centers had simple lesions. In total, 47% and 37% of the patients attended in level 1 and level 2 centers had moderately complex lesions, respectively, and 26% and 17% had highly complex lesions, respectively (figure 3). In general, the most frequent diagnostic groups were Tetralogy of Fallot (12%) and aortic coarctation (11%), but there were also significant differences between the 2 types of centers; the most frequent diagnoses in level 2 centers were bicuspid aortic valve disease, ostium secundum atrial septal defect, and ventricular septal defect (figure 3).
Clinical characteristics and diagnostic procedures. Comparison between level 1 and level 2 centers
| Characteristics | Specifications | Total (n=2289) | Level 1 (n=1685) | Level 2 (n=604) | P |
|---|---|---|---|---|---|
| Demographic data | Mena | 1145 (50) | 834 (50) | 311 (52) | .402 |
| Age, yb | 35 [25-45] | 35 [25-45] | 34 [25-45] | .126 | |
| Age at diagnosis, y | 1 [0-18] | 1 [0-15] | 1 [0-26] | .004 | |
| Lesion complexity | Simple | 739 (32) | 460 (27) | 279 (46) | <.001 |
| Moderately complex | 1011 (44) | 790 (47) | 221 (37) | ||
| Highly complex | 539 (24) | 435 (26) | 104 (17) | ||
| Diagnostic groups | Tetralogy of Fallot | 278 (12) | 231 (14) | 47 (7.8) | <.001 |
| Aortic coarctation | 258 (11) | 195 (12) | 63 (10) | ||
| Bicuspid aortic valve disease | 206 (9) | 122 (7.2) | 84 (14) | ||
| Ostium secundum ASD | 196 (8.6) | 122 (7.2) | 74 (12) | ||
| Transposition of the great vessels | 170 (7.4) | 146 (8.7) | 24 (4.0) | ||
| Canal defects | 167 (7.3) | 126 (7.5) | 41 (6.8) | ||
| Ventricular septal defect | 162 (7.1) | 106 (6.3) | 56 (9.3) | ||
| Pulmonary valve lesion | 131 (5.7) | 83 (4.9) | 48 (7.9) | ||
| Pulmonary vascular disease | 109 (4.8) | 85 (5.0) | 24 (4.0) | ||
| Fontan procedures | 98 (4.3) | 78 (4.6) | 20 (3.3) | ||
| Sinus venosus ASD/APVR | 77 (3.4) | 60 (3.6) | 17 (2.8) | ||
| Ebstein's anomaly | 63 (2.8) | 48 (2.8) | 15 (2.5) | ||
| Fixed subaortic stenosis | 63 (2.8) | 46 (2.7) | 17 (2.8) | ||
| Pulmonic subvalvular stenosis | 61 (2.7) | 51 (3.0) | 10 (1.8) | ||
| Pulmonary atresia (all forms) | 56 (2.4) | 44 (2.6) | 11 (2.0) | ||
| Unrepaired cyanotic congenital heart disease | 48 (2.1) | 38 (2.3) | 8 (1.7) | ||
| Congenitally corrected transposition of the great arteries | 41 (1.8) | 33 (2.0) | 8 (1.3) | ||
| Persistent ductus arteriosus | 31 (1.4) | 16 (0.9) | 13 (2.5) | ||
| Double outlet right ventricle | 18 (0.8) | 12 (0.7) | 6 (1.0) | ||
| Mitral valve lesions | 16 (0.7) | 13 (0.8) | 3 (0.5) | ||
| Coronary artery anomalies | 11 (0.5) | 9 (0.5) | 2 (0.3) | ||
| Supravalvular aortic stenosis | 9 (0.4) | 7 (0.4) | 2 (0.3) | ||
| Supravalvular pulmonary stenosis | 9 (0.4) | 7 (0.4) | 2 (0.3) | ||
| Miscellaneous | 11 (0.5) | 8 (0.5) | 3 (0.5) | ||
| Surgical history | Surgical or percutaneous intervention | 1756 (77) | 1323 (79) | 433 (72) | .001 |
| Palliative intervention only | 144 (6.3) | 110 (6.5) | 34 (5.6) | .008 | |
| Reparative intervention | 1.367 (60) | 1,034 (61) | 333 (55) | ||
| Percutaneous intervention alone | 154 (6.7) | 99 (5.9) | 55 (9.1) | ||
| Age at intervention, y | 4 [1-12] | 4 [1-10] | 5 [1-16] | .002 | |
| Reoperation in adulthood | 517 (23) | 424 (25) | 93 (15) | <.001 | |
| Diagnostic procedures | ECG | 2288 (100) | 1684 (100) | 604 (100) | .549 |
| Echocardiography | 2289 (100) | 1685 (100) | 604 (100) | - | |
| Chest X-ray | 1289 (56) | 989 (59) | 152 (50) | <.001 | |
| Holter monitoring | 440 (19) | 340 (21) | 100 (17) | .053 | |
| Ergometry | 830 (36) | 680 (40) | 150 (25) | <.001 | |
| Cardiopulmonary assessment | 388 (17) | 365 (22) | 23 (3.8) | <.001 | |
| Cardio-MRI/CTAb | 1124 (49) | 938 (56) | 186 (31) | <.001 |
APVR, anomalous pulmonary venous return; ASD, atrial septal defect; CTA, computed tomography angiography; ECG, electrocardiography; MRI, magnetic resonance imaging.
Values are expressed as No. (%) or median [interquartile range]. Percentages are rounded to absolute values when they are ≥ 10 and to the first decimal place when they are < 10. Qualitative multiple response variables are compared together.
In total, 77% of the patients had undergone previous cardiovascular intervention. The percentage was significantly higher in level 1 centers (79% vs 72%). More patients had undergone percutaneous procedures alone in level 2 centers. Age at the time of intervention was significantly lower in patients in level 1 centers. In addition, 517 patients (23%) had undergone reintervention during adulthood at a mean age of 31±13 years: 25% of these patients underwent reintervention in level 1 centers and 15% in level 2 centers. There were no significant differences between the 2 types of center regarding surgical or percutaneous reintervention (P=.581).
Diagnostic techniquesRegardless of the level of the center, all of the patients underwent electrocardiography and echocardiography at clinical assessment, but chest X-ray was only performed in 56% of patients and Holter monitoring in 19% of patients. Cardiac stress tests were performed in 830 patients (36%), although more were performed in level 1 centers (40%) than in level 2 centers (25%). Interestingly, 365 of the patients in level 1 centers (22%) underwent ergospirometry vs 3.8% in level 2 centers. Finally, a significantly higher percentage of patients underwent advanced radiologic imaging procedures in level 1 centers (56%) than in level 2 centers (31%).
DISCUSSIONThis is the first study to analyze the overall national health care structure, health care activity, and clinical characteristics of patients with ACHD. Other studies have analyzed the health care structure in specific countries or have reported national clinical records, but none have analyzed these aspects together to provide an overall picture of ACHD health care.
Comparison with other countriesThe first ACHD health care network was founded in Canada in October 1991.18 Currently, it includes 15 centers, 8 of which are level 1, serving a population of 37 million. In the UK, there are 11 level 1 centers and 5 level 2 centers serving a population of 66 million.19 ACHD health care in the United States is less structured, but some European countries, such as the Netherlands, Germany, and Switzerland, have followed examples of Canada and the UK by establishing ACHD health care networks of level 1 and 2 centers.
In Spain, the development of the ACHD health care network has followed a similar course. The greatest growth occurred in the second half of the 2000s followed by a steady increase, demonstrating the high level of interest in this subspecialty. Although the recommendations of the European Society of Cardiology10 do not require centers to have their own transplant program as an indispensable condition for being considered level 1, advanced heart failure remains the main clinical problem in ACHD.20 Thus, 10 centers with a complete health care structure and advanced heart failure and transplant programs were designated as level 1. Therefore, there are 2.2 centers for every 10 million inhabitants in Spain. This ratio complies with the recommendations of the 32nd Bethesda Conference of 2001, which estimated that there should be 1 referral center for every 5 to 10 million inhabitants.21 The Spanish National Health System has recognized 9 of these 10 centers as CSURs; thus, if some of the other centers were designated as CSURs a more balanced geographic distribution would be achieved.
There are also 14 level 2 centers, making a total of 24 specialized centers. This figure fulfills the international recommendations of 1 regional center for every 2 million inhabitants.22 However, the geographic distribution of these centers is not optimal. As shown in figure 1, some regions do not have at least 1 center with specialized ACHD clinics. However, it may be the case that this information is incomplete and that other communities have their own projects to serve this population.
Patients under follow-upSeveral studies have attempted to quantify the current number of ACHD patients; a systematic review described a prevalence of between 1.7 and 4.5 patients/1000 inhabitants (mean, 3‰).23 Extrapolating these data, there would be around 120 000 ACHD patients in Spain. Our study shows that there were less than 20 000 ACHD patients under follow-up in the 24 registered centers. This figure is less than one-sixth of the total estimated. This information may be relevant, because an association has been found between the referral of ACHD patients to specialized centers and significant reductions in mortality.24 However, our results are similar to those of other developed countries.8,25 Although calculations based on population studies may be overestimated, the abovementioned disparity suggests that many ACHD patients are not under active follow-up in experienced units.
Structure and activitySpanish centers have a health care structure comparable to that of other developed countries. At the national level, the mean number of surgical interventions, percutaneous therapeutic procedures, and arrhythmia ablations in level 1 centers were 38, 24, and 15, respectively. These means are similar to those of the Canadian health care network centers (31, 32 and 15)8 and 18 selected European centers.9 Moreover, surgical interventions and percutaneous procedures in adults with CHD that were performed in specialized clinics accounted for 99% and 91% of those reported by the Spanish Society for Thoracic and Cardiovascular surgery and the Spanish Society of Cardiology registries, respectively.11,12 However, 28% of percutaneous procedures, 21% of arrhythmia ablations, and 17% of surgeries were performed in level 2 centers. The clinical practice guidelines recommend that these therapeutic procedures should be performed in centers with more experience, and so a greater number complex procedures should be performed in level 1 centers.26
To meet the needs of ACHD patients, the number of centers and the number of patients being monitored should be taken into account, as well as the provision of the human and material resources required.18,27,28 This study shows that Spanish centers comply with international recommendations and pay special attention to specific training. The main weaknesses detected were the low percentages of ACHD nurse specialists on staff and structured transition programs. These aspects could be interrelated because nursing staff are the main human capital in structured transition programs. In Spain, the lack of development of specialized training programs in nursing is common to other specialties. Although the clinical assessment process was similar in level 1 and level 2 centers, the main differences were related to complete cardiopulmonary assessment or the use of advanced radiologic imaging procedures. Moreover, none of the level 2 centers had their own heart transplant and advanced heart failure programs, suggesting the need for all centers to be interconnected in a health care network.
Specific heart diseaseThe distribution of specific CHDs in adults continues to be a matter of speculation. Most estimates are based on population studies. It is generally assumed that more than 50% of ACHD patients have simple lesions, 30% to 40% have moderately complex lesions, and less than 15% have highly complex lesions.14 However, population studies have important methodological limitations. The International Classification of Diseases system does not always differentiate a nosological entity from a variant. Furthermore, it is not always easy to differentiate congenital lesions from acquired lesions, particularly in the setting of valvular abnormalities. Thus, the main source of uncertainty involves simple lesions.
In addition, the information provided by the records may have a selection bias. Most of the registries come from high-volume tertiary hospitals, where there may be an overrepresentation of more complex lesions. This study describes an unselected sample of consecutive patients with ACHD attended in 18 Spanish centers. It should be noted that 24% of the patients had highly complex lesions, 44% had moderately complex lesions, and 32% had simple lesions. The results show that there were more patients with more complex lesions in level 1 centers and more patients with simple lesions in level 2 centers. However, 17% of patients in level 2 centers had very complex lesions. The guidelines recommend that these patients should undergo comprehensive follow up in centers with the greatest experience. A common health care model, advocated in Europe, Canada, Australia, and the United States, recommends that all adults with CHD should be assessed by a multidisciplinary team in a specialized center, thus allowing the individual determination of the appropriate level of care and follow-up.2
LimitationsThe main limitation of this study is due to the survey methodology used, which, in some cases, may have relied on estimated data. However, the fact that therapeutic procedures accounted for 99% and 91% of those reported by national Cardiac Surgery and Cardiac Catheterization registries, respectively, suggests that these data are relatively reliable. In addition, although only 75% of the centers participated in the specific heart disease registry, the percentage was similar in level 1 and level 2 centers (70% and 79% respectively). This result provides a reasonably accurate snapshot of ACHD patients currently under follow-up in Spain, including centers with a widely heterogeneous volume of patients and activities. Although special care was taken to avoid duplication in the registry, some patients followed up in level 2 centers may have also been followed up in level 1 centers. The data obtained show clinical activity during a specific period and cannot be used to estimate the flow of patients within the health care network. In addition, the survey did not include palliative care and advance health care directives or specific rehabilitation programs.
CONCLUSIONSThis report shows that there is increasing interest in ACHD health care. The number and organizational development of ACHD centers complies with international recommendations, but there are large geographic areas without specific ACHD centers. The main weaknesses are the low percentages of ACHD nurse specialists on staff and structured transition programs. Although most of the surgical interventions, therapeutic cardiac catheterization procedures, and electrophysiological procedures performed in Spain are concentrated in specialized centers, it is recommended that complex procedures should be performed in level 1 centers. In general, although more ACHD patients with moderately complex or highly complex lesions are attended in level 2 centers, it is recommended that ACHD patients with highly complex lesions should undergo comprehensive follow up in centers with the most experience. To facilitate patient flow between centers, the health care structure network should be strengthened at community and supra-community levels.
FUNDINGInstituto de Salud Carlos III, Ministerio de Economía y Competitividad, Spain (Exp. PI14/02099 and PI17/01327), cofinanced by the European Regional Development Fund.
CONFLICTS OF INTERESTP. Gallego is Associate Editor of the Revista Española de Cardiología; the editorial procedure established by the journal has been followed to ensure the impartial treatment of the manuscript. There are no other conflicts of interest.
- -
ACHD is an emerging pathology in developed countries with extensive experience in cardiology and pediatric cardiac surgery.
- -
In recent years, international recommendations have been established that address the health care structure and activity of specialized ACHD centers.
- -
However, there has been little analysis of the health care structure of this population and the clinical characteristics of patients under active follow-up in specialized ACHD clinics in Spain.
- -
Currently, there are 24 recognized ACHD centers in Spain (1 center per 2 million inhabitants), but there are large regions without such centers. The equipment, staff, and structure of these centers comply with international recommendations. However, there are low percentages of ACHD nurse specialists on staff and structured transition programs.
- -
Most of the ACHD patients under follow-up have highly complex or moderately complex lesions, but many such patients could be lacking specific health care. All centers should be incorporated within networks to facilitate diagnostic and therapeutic activity and multicenter research.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2019.09.032