Atrial cardiomyopathy is a consequence of several pathophysiological processes with dysfunction and fibrosis of the left atrium (LA). This condition is often diagnosed in advanced stages due to incidental atrial fibrillation (AF), thromboembolic complications, or heart failure.1 Image based biomarkers can be considered as surrogates of the status of this atrial substrate as they are currently able to precisely quantify LA size, function and, potentially, geometry and tissue composition. A widely available, noninvasive, and inexpensive imaging technique such as transthoracic echocardiography (TTE) could be easily applied in large cohorts of at-risk patients and would be readily applicable if shown to be useful in the early detection of at-risk patients.
Moreover, in recent years, LA function has shown prognostic yield in various clinical settings (eg, diastolic dysfunction, heart failure, AF, etc).2 Analysis of LA function may demonstrate abnormal performance of the atrium prior to changes in LA size. Volumetric quantification of the LA and myocardial strain parameters allow detailed description of each LA contribution (reservoir, conduit, and contractile)3 and both can be adequately obtained with TTE.
While strain assessment provides detailed information on regional myocardial deformation and can detect subtle changes in atrial function, it is influenced by cavity size, yielding less accuracy in patients with significant atrial remodeling. On the other hand, 3-dimensional (3D) volume assessment offers a comprehensive evaluation of atrial morphology and function, without geometric assumptions, accommodating complex shapes, and facilitating detailed analysis of remodeling and changes in atrial size, but reflects volumetric changes that may be only reflected in more advanced stages of myocardial dysfunction. Both techniques require adequate image quality.
Although these 2 methods can study all these LA contributions, the relationship between them is poorly understood and limits understanding and standardization of evaluation of LA function. Given the potential differences between 2-dimensional (2D) strain and 3D volume assessment in evaluating atrial function, understanding their relationship is crucial to further explore the potential contributions they can offer. Therefore, we sought to analyze the agreement in assessing LA function with 2 modalities, phasic 3D volumetric assessment and strain imaging, using TTE in a large population cohort of patients at epidemiological risk of AF.
In this prospective observational study, we analyzed LA function in 483 patients (mean age 51.6±7.2 years; female sex, 29.8%). All patients were in sinus rhythm and at epidemiological risk of AF (high intensity endurance athletes [n=277, 57.35%], chronic hypertension [n=178, 36.85%], and mitral regurgitation [n=28, 5.80%]). Informed consent was obtained from all study participants.
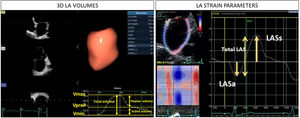
We obtained 3D TTE images with a dedicated commercially available echographic system (Vivid 9 and E95, General Electric, United States) and 3D LA volumes as well as LA strain were determined using a commercially available dedicated software package (Echo Pac, General Electric, United States). LA function was assessed based on phasic LA volumes and speckle tracking echocardiography derived myocardial deformation. Indexed 2D and 3D phasic LA volumes (ie, minimal [Vmin], maximal [Vmax], and the volume before atrial contraction at the beginning of the P wave [VpreP]) were used to calculate indices of LA function and total ejection fraction (related to LA reservoir function), as well as active (LA contractile function) and passive (LA conduit function) emptying fractions.4,5
We calculated the Pearson correlation coefficient between each pair of continuous quantitative variables. Inter- and intraobserver variability in measuring LA contractile strain were 0.3% (95% confidence interval [95%CI], −6.1 to 6.7) and 0.7% (95%CI, −1.39 to 2.85), while inter- and intraobserver variability in LA conduit strain were 0.9% (95%CI, −3.9 to 5.8) and 0.9% (95%CI, −3.7 to 5.6), respectively. The intra- and interobserver variability in the calculation of the maximum 3D LA volume were 0.7±5.2mL and 0.9±7.4mL, respectively.
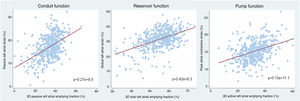
Mean left ventricular ejection fraction was 61.2±6.6% and indexed 3D LA volume was 37.4±10.8 mL/m2. Mean total 3D LA emptying fraction was 55.4±7.2% and global LA strain was 31.7±6.3% (reservoir function), while mean passive 3D emptying fraction was 34.2±9.1% and passive LA strain was 17.1±5.1% (conduit function). Finally, mean 3D LA active emptying fraction was 32±8.4% and peak atrial contraction strain was 15.6±2.8% (contractile function) (figure 1). Pearson correlation coefficients between each pair of variables assessing LA reservoir, conduit and pump function were 0.48 (P<.001), 0.48 (P<.001) and 0.38 (P<.001), respectively. Scatter plot graphics representing each LA function measured by the different modalities are shown in figure 2.
Our data show a moderate lineal and positive correlation between 3D volume and strain values assessing reservoir, conduit, and pump LA function. The correlation was higher between parameters evaluating reservoir and conduit function than contractile function. Theoretically, 2D strain may exhibit earlier changes than 3D volume assessment when evaluating atrial function, allowing detection of atrial dysfunction at an earlier stage, which could be one of the reasons for the modest correlation observed between 2D strain and 3D volume in assessing atrial LA function. The absence of clearly established reference values for normal LA function poses challenges in further interpreting the relationship between these 2 parameters. Our cohort includes patients with both nondilated and dilated LA, although the average value indicates only slight LA dilation. The presence or absence of LA dilation may have implications for the assessment of atrial function using 2D strain or 3D volume measurements. Despite a significant correlation between 3D volumes and 2D strain, the obtained values are not interchangeable and, therefore, the classification of different stages of LA function might vary according to the modality used.
Although the objective of the study did not include intergroup comparisons, the absence of a control group may constitute a limitation of the research. Technological improvement in 3D echo quantification and deformation imaging might increase the reproducibility of both methodologies and consequently improve agreement. Further studies will be needed to fully define normal and abnormal LA function and provide prognostic value independently of the technical modalities used for its measurement.
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSAll authors have equally contributed significantly to article conception and drafting.
CONFLICTS OF INTERESTL. Sanchis is associate editor of Rev Esp Cardiol. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed. The remaining authors have no conflicts of interest.