To the Editor,
A 53-year-old woman was referred for stress echocardiography. Her clinical record included a history of high blood pressure and VVIR pacemaker implantation secondary to atrioventricular nodal ablation for symptomatic refractory paroxysmal atrial fibrillation. During the previous 3 months, she reported episodes of precordial oppression and dyspnea triggered by emotionally stressful situations. Exercise echocardiography was indicated because of recurrent pain and the pacemaker rhythm in the electrocardiogram (ECG).
Baseline echocardiography showed concentric left ventricular hypertrophy (12mm) and a left ventricular ejection fraction (EF) of 67%, with interventricular asynchrony due to pacemaker stimulation without alterations in segmental contractility. At the end of the fifth minute of the Bruce protocol (heart rate 105bpm [63% of maximum], blood pressure 180/85mmHg), the patient experienced intense chest pain. Echocardiography showed septoapical and inferoapical akinesis.
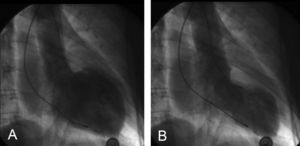
Given the persistent pain, the patient was referred to our center for urgent coronary angiography. The coronary arteries appeared normal. Ventricular angiography showed akinesis of the middle segments of the anterior and inferior wall, apical hypokinesia, basal segment hypercontractility and an EF of 45%–50% without an intraventricular gradient (Figure 1).
Figure 1. Ventricular angiography. Akinesis of the middle segments, apical hypokinesia, and baseline hypercontractility. Diastole (A) and systole (B).
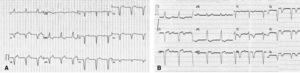
The patient was hospitalized in the coronary unit, where treatment with atenolol was begun. She experienced no new episodes of chest pain. The troponin-T level reached a maximum of 0.19ng/mL (normal <0.1ng/mL) in 24h and normalized at 48h (0.07ng/mL); the creatine kinase level was within the normal range. At 24h, the ECG revealed a negative precordial T wave (Figure 2). At 1 week, the echocardiogram showed no alterations in left ventricular segmental contractility and the EF had recovered to 65%. Consequently, the patient was discharged with a diagnosis of Tako–Tsubo syndrome.
Figure 2. ECGs at baseline (A) and 24h (B). Appearance of symmetrical precordial negative T waves.
Tako–Tsubo syndrome—or stress-induced cardiomyopathy—is a clinical entity characterized by the presence of chest pain in the context of a stressful situation, an ECG that mimics ST-segment elevation myocardial infarction, normal coronary arteries, and transitory left ventricular dysfunction due to midapical akinesis or dyskinesis.1 In acute coronary syndromes,2 the estimated prevalence is 0.7%. Knowledge of the pathophysiology is quite limited although it has been suggested that dysfunction of the coronary microcirculation occurs due to the release of catecholamines into plasma triggered by stress.3 However, in some cases, no trigger mechanism has been found.4 In our patient, the only trigger was the physical and emotional stress of undergoing a test for ischemia. The baseline echocardiogram was normal and akinesis appeared during the test. Ventricular angiography performed shortly after this suggested Tako–Tsubo syndrome. In our patient, the dysfunction mainly affected the middle segments, a location that may—albeit infrequently—be the only one involved.5 We were not able to repeat the test in order to determine the reproducibility of the response. However, this complication is extremely rare and no data on its occurrence have been reported in the literature. No clear recommendations on treatment exist, though previous reports propose standard management of the complications and beta-blocker administration.5
The main differential diagnosis is spasm of the left anterior descending artery. However, in this condition, contractility alterations would be incompatible with the anomalies observed in our patient. Moreover, the appearance of symmetrical negative T waves in the precordial region, a slight elevation in the troponin level, and normalization of left ventricular contractility 1 week after the episode support the diagnosis of stress-induced cardiomyopathy triggered by exercise echocardiography in this patient.
Corresponding author. angelkarpin@hotmail.com