New biomarkers could improve the predictive capacity of classic risk functions. The aims of this study were to determine the association between circulating levels of apolipoprotein A1 (apoA1), apolipoprotein B (apoB), albumin, and 25-OH-vitamin D and coronary events and to analyze whether these biomarkers improve the predictive capacity of the Framingham-REGICOR risk function.
MethodsA case-cohort study was designed. From an initial cohort of 5404 individuals aged 35 to 74 years with a 5-year follow-up, all the participants who had a coronary event (n = 117) and a random group of the cohort (subcohort; n = 667) were selected. Finally, 105 cases and 651 individuals representative of the cohort with an available biological sample were included. The events of interest were angina, fatal and nonfatal myocardial infarction and coronary deaths.
ResultsCase participants were older, had a higher proportion of men and cardiovascular risk factors, and showed higher levels of apoB and lower levels of apoA1, apoA1/apoB ratio, 25-OH-vitamin D and albumin than the subcohort. In multivariate analyses, plasma albumin concentration was the only biomarker independently associated with coronary events (HR, 0.73; P = .002). The inclusion of albumin in the risk function properly reclassified a significant proportion of individuals, especially in the intermediate risk group (net reclassification improvement, 32.3; P = .048).
ConclusionsPlasma albumin levels are inversely associated with coronary risk and improve the predictive capacity of classic risk functions.
Keywords
Tailoring the intensity of preventive interventions to individual needs requires the use of cardiovascular risk scores adapted to and validated in the target population.1,2 Although established risk scores have been validated, they are limited by their low sensitivity, which results in a high proportion of coronary and cardiovascular events occurring in people classified as being at intermediate risk.3,4 The inclusion of biomarkers in conventional risk scores could increase the precision of risk estimates.5
The various classes of biomarker that have been proposed and analyzed include genetic,6 biochemical,7,8 and imaging biomarkers.9 Among the biochemical biomarkers, apolipoprotein A1 (apoA1), apolipoprotein B (apoB), and the ratio between them track cardiovascular risk and the relative levels of antiatherogenic and atherogenic lipoproteins.10 Cardiovascular risk also shows a widely reported inverse association with plasma albumin,11 which is also inversely related to oxidative and inflammatory status. Another biochemical marker is vitamin D, which also shows an inverse association with cardiovascular risk12 and with several conventional cardiovascular risk factors.13 However, few studies have analyzed the ability of these biomarkers to predict coronary events, either individually or in combination.
The aims of this study were as follows: a) to determine the associations of apoA, apoB, and albumin in plasma and vitamin D in serum with the incidence of cardiovascular events during the follow-up of a population cohort; and b) to examine whether these biomarkers improve the predictive function of the REGICOR risk score in a study population aged 35 to 74 years.
METHODSStudy Design and ParticipantsA case-cohort study was designed within the follow-up of the REGICOR (Registre GIroní del COR) population cohort study.14 In REGICOR, a 6352-participant population cohort was recruited in 2005, with a response rate > 70%. Of these participants, 5404 were aged between 35 and 74 years and were free of cardiovascular disease at the time of inclusion. All participants were followed up between 2009 and 2013.
In line with the case-cohort study design, we included all participants who had a coronary event (n = 117) together with a random subcohort of participants included in the baseline evaluation at an approximate ratio of 1:6 (n = 667). Of these participants, we selected for analysis those with an available biological sample (105 case participants and 651 subcohort participants). The incidence of the event of interest in the original 5404-participant sample was 2.7%; assuming a type I error rate of 5%, the case-cohort sample size (n = 756) provides a statistical power of 80% for the statistically significant identification of a relative risk ≥ 1.58 per standard deviation increase in the biomarker. Statistical power was calculated using the ccsize function in the gap package in R. We also included 43 competing noncoronary cardiovascular events.
All participants were informed of the aims of the study and gave written consent. The study was approved by the local clinical research ethics committee.
BiomarkersParticipants provided biological samples after a 10 to 14 hour fast. Once the blood was centrifuged, and after coagulation in the case of serum, samples of serum and EDTA (ethylenediaminetetraacetic acid) plasma were aliquoted and stored at –80°C until analysis. Glucose, total cholesterol, and triglycerides were measured in serum by enzymatic methods, whereas high-density lipoprotein (HDL) cholesterol was measured directly (Roche Diagnostics; Basel, Switzerland) in a Cobas Mira Plus autoanalyzer (Roche Diagnostics). If the triglyceride concentration was < 300 mg/dL, low-density lipoprotein cholesterol was estimated with the Friedewald equation.
Vitamin D was measured in serum by competitive ELISA for 25-hydroxy vitamin D (Immunodiagnostic Systems; Boldon, United Kingdom). Plasma albumin concentration was assayed by bromocresol green dye binding (ABX Diagnostics; Montpellier, France) and plasma apoA1 and apoB concentrations by immunoturbidimetric assay (ABX Diagnostics) in a Cobas Mira Plus autoanalyzer.
The variables analyzed in the Cobas Mira Plus autoanalyzer (albumin, apoA1, and apoB) were checked against external quality assurance standards from the Spanish Society of Clinical Chemistry (Sociedad Española de Química Clínica). Interassay variation coefficients for albumin, apopA1, apoB, and 25-OH-vitamin D were 3.19%, 3.37%, 3.21%, and 5.72%, respectively.
Follow-up and Events of InterestVarious information sources were used during follow-up. Nonfatal events of interest were identfied through regular structured telephone interviews and a re-evaluation visit, and fatal events were identified from official death records. Events of interest were the appearnace of angina, fatal or nonfatal myocardial infarction, and coronary death.
Nonfatal events were validated by reviewing the medical records of participants reporting angina pectoris or a myocardial infarction. Deaths due to coronary disease were identified according to ICD (International Classification of Diseases) codes ICD-9 410-414 and ICD-10 I20-I22, I24, I25. A committee categorized all events according to standard criteria. Angina pectoris was defined as the presence of symptoms accompanied by an objective demonstration of ischemia in the electrocardiogram or > 50% coronary stenosis by coronary angiography. Myocardial infarction was defined according to international criteria.15
Recorded competing cardiovascular events were noncoronary cardiovascular death and nonfatal cerebrovascular disease.
Other VariablesQuestionnaires and standard methods were used to determine conventional cardiovascular risk parameters14: systolic and diastolic blood pressure, total cholesterol, HDL cholesterol, smoking, and diet. Smokers were defined as participants who were active smokers or who had stopped smoking within the previous year. Diabetes was defined as baseline blood glucose ≥ 126 mg/dL or treatment with oral antidiabetic drugs or insulin. Cardiovascular risk was estimated with the REGICOR score validated for the Spanish population.3
Statistical AnalysisBiomarkers of interest showing a nonnormal distribution were logarithmically transformed. Vitamin D was stratified into 3 bands widely used in the medical literature: < 30 nmol/L, 30-49 nmol/L, and ≥ 50 nmol/L.12 Differences between the case population and subcohort in sociodemographic variables, risk factors, and biomarkers were determined using the method of Lin and Ying for case-cohort studies.16 The relative risk of coronary disease associated with a 1 standard deviation increase in each biomarker of interest was estimated using the method proposed by Pintilie et al. to accommodate the existence of competing risks.17 We developed 2 multivariate models, the first adjusted for age and sex and the second additionally adjusted for systolic and diastolic blood pressure, total cholesterol, HDL cholesterol, diabetes, and smoking status. Furthermore, each biomarker was analyzed separately; all biomarkers were subsequently included in the multivariate model, and only those showing a statistically significant association with the event of interest were maintained. All variables except for diabetes fulfilled the assumption of risk proportionality. We confirmed that stratification for diabetes did not significantly modify the magnitude of association between the biomarkers of interest and coronary events.
The net contribution of biomarkers to the predictive capacity of conventional risk factors was evaluated from the improvement in discrimination, determined by analyzing the difference in Harrell's C statistic adapted to case-cohort studies.18 Proper reclassification was verified by estimating the categorical and continuous net reclassification improvement (NRI). NRI categories were defined using the standard cut-points for the 10-year risk of a coronary event in the Spanish population (5% and 10%).3 The number of events at 10 years in each risk category was obtained by preparing event-free survival curves. The NRI confidence intervals to accommodate uncertainty in the estimates were calculated using bootstrap resampling techniques.19 For the estimation of NRI in the intermediate risk group, we used the method proposed by Paynter and Cook to correct overestimation due to the use of a single risk category.20
Statistical analyses were conducted in R version 3.0.1 (R: a language and environment for statistical computing; the R Foundation for Statistical Computing, Viena, Austria). We used the function developed by Pintilie et al. to accommodate the existence of competing risks in case-cohort studies17 and wrote R code functions to calculate the C statistic for case-cohort studies.
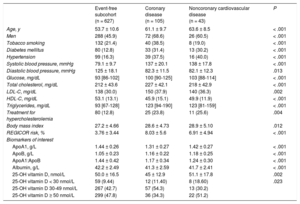
RESULTSThe subcohort included 13 participants with a coronary event and 11 with a competing noncoronary event. The baseline characteristics of the study population are presented in Table 1. There were 105 case participants with coronary events, 43 with noncoronary cardiovascular events, and 627 subcohort participants free of coronary and other cardiovascular events at the end of follow-up. Compared with the event-free population, the case population with coronary disease was older and included a higher proportion of men, a higher prevalence of conventional risk factors, and a higher cardiovascular risk estimated with the REGICOR score. The case population also had higher levels than the event-free subcohort of apoB and lower values for apoA1, the apoA1:apoB ratio, 25-OH-vitamin D, and albumin (Table 1).
Study Population Characteristics Stratified for Coronary and Noncoronary Cardiovascular Events
| Event-free subcohort (n = 627) | Coronary disease (n = 105) | Noncoronary cardiovascular disease (n = 43) | P | |
|---|---|---|---|---|
| Age, y | 53.7 ± 10.6 | 61.1 ± 9.7 | 63.6 ± 8.5 | < .001 |
| Men | 288 (45.9) | 72 (68.6) | 26 (60.5) | < .001 |
| Tobacco smoking | 132 (21.4) | 40 (38.5) | 8 (19.0) | < .001 |
| Diabetes mellitus | 80 (12.8) | 33 (31.4) | 13 (30.2) | < .001 |
| Hypertension | 99 (16.3) | 39 (37.5) | 16 (40.0) | < .001 |
| Systolic blood pressure, mmHg | 79.1 ± 9.7 | 137 ± 20.1 | 138 ± 17.8 | < .001 |
| Diastolic blood pressure, mmHg | 125 ± 18.1 | 82.3 ± 11.5 | 82.1 ± 12.3 | .013 |
| Glucose, mg/dL | 93 [86-102] | 100 [90-125] | 103 [88-114] | < .001 |
| Total cholesterol, mg/dL | 212 ± 43.6 | 227 ± 42.1 | 218 ± 42.9 | < .001 |
| LDL-C, mg/dL | 138 (30.0) | 150 (37.9) | 140 (36.3) | .002 |
| HDL-C, mg/dL | 53.1 (13.1) | 45.9 (15.1) | 49.9 (11.9) | < .001 |
| Triglycerides, mg/dL | 93 [67-128] | 123 [94-190] | 123 [81-159] | < .001 |
| Treatment for hypercholesterolemia | 80 (12.8) | 25 (23.8) | 11 (25.6) | .004 |
| Body mass index | 27.2 ± 4.66 | 28.6 ± 4.73 | 28.9 ± 5.10 | .012 |
| REGICOR risk, % | 3.76 ± 3.44 | 8.03 ± 5.6 | 6.91 ± 4.94 | < .001 |
| Biomarkers of interest | ||||
| ApoA1, g/L | 1.44 ± 0.26 | 1.31 ± 0.27 | 1.42 ± 0.27 | < .001 |
| ApoB, g/L | 1.05 ± 0.23 | 1.16 ± 0.22 | 1.18 ± 0.25 | < .001 |
| ApoA1:ApoB | 1.44 ± 0.42 | 1.17 ± 0.34 | 1.24 ± 0.30 | < .001 |
| Albumin, g/L | 42.2 ± 2.49 | 41.3 ± 2.59 | 41.7 ± 2.41 | < .001 |
| 25-OH vitamin D, nmol/L | 50.0 ± 16.5 | 45 ± 12.9 | 51.1 ± 17.8 | .002 |
| 25-OH vitamin D < 30 nmol/L | 59 (9.44) | 12 (11.40) | 8 (18.60) | .023 |
| 25-OH vitamin D 30-49 nmol/L | 267 (42.7) | 57 (54.3) | 13 (30.2) | |
| 25-OH vitamin D ≥ 50 nmol/L | 299 (47.8) | 36 (34.3) | 22 (51.2) | |
ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Data are expressed as No. (%), mean ± standard deviation, or median [interquartile range].
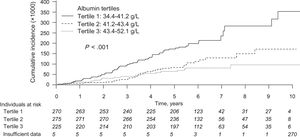
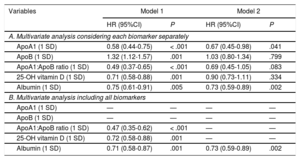
The cumulative incidence of coronary events after adjustment for competing risks is represented in Figure. Separate analysis of each biomarker of interest showed that all were associated with the incidence of coronary events in the model adjusted for age and sex (Table 2A, model 1). However, after adjustment for conventional risk factors, the only biomarkers maintaining an association with coronary events were the plasma concentrations of albumin and apoA1 (Table 2A, model 2). In the analysis of all biomarkers in the same multivariate model, only albumin maintained a statistically significant association after adjusting for age, sex, and conventional risk factors (Table 2B, model 2).
Cumulative incidence curves for coronary events after adjusting for the competing risk of noncoronary cardiovascular events. Insufficient data, plasma albumin data unavailable; 651 subcohort + 105 coronary events + 43 noncoronary cardiovascular events = 799; 799 – 13 coronary events and – 11 noncoronary cardiovascular events in the subcohort = 775.
Association Between Biomarkers of Interest (per Standard Deviation) and the Incidence of Coronary Events, Estimated With Different Approaches and Multivariate Models and Adjusting for Competing Risks
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| HR (95%CI) | P | HR (95%CI) | P | |
| A. Multivariate analysis considering each biomarker separately | ||||
| ApoA1 (1 SD) | 0.58 (0.44-0.75) | < .001 | 0.67 (0.45-0.98) | .041 |
| ApoB (1 SD) | 1.32 (1.12-1.57) | .001 | 1.03 (0.80-1.34) | .799 |
| ApoA1:ApoB ratio (1 SD) | 0.49 (0.37-0.65) | < .001 | 0.69 (0.45-1.05) | .083 |
| 25-OH vitamin D (1 SD) | 0.71 (0.58-0.88) | .001 | 0.90 (0.73-1.11) | .334 |
| Albumin (1 SD) | 0.75 (0.61-0.91) | .005 | 0.73 (0.59-0.89) | .002 |
| B. Multivariate analysis including all biomarkers | ||||
| ApoA1 (1 SD) | — | — | — | — |
| ApoB (1 SD) | — | — | — | — |
| ApoA1:ApoB ratio (1 SD) | 0.47 (0.35-0.62) | < .001 | — | — |
| 25-OH vitamin D (1 SD) | 0.72 (0.58-0.88) | .001 | — | — |
| Albumin (1 SD) | 0.71 (0.58-0.87) | .001 | 0.73 (0.59-0.89) | .002 |
ApoA1, apolipoprotein A1; ApoB, apolipoprotein B; SD, standard deviation; HR, hazard ratio; 95%CI, 95% confidence interval.
Model 1, adjusted for age and sex. Modelo 2, ajusted for age, sex, smoking, diabetes mellitus, systolic blood pressure, diastolic blood pressure, total cholesterol, and high-density lipoprotein cholesterol.
The inclusioun of plasma albumin concentrations in the REGOCR risk score did not improve its discriminatory power (Table 3). However, risk reclassification analysis revealed improved risk category assignment for the case and subcohort populations. This improvement was statistically significant for continuous NRI and for NRI in individuals classified as being at intermediate risk (clinical NRI). The risk category improvement was marginally nonsignificant for categorical NRI in the whole sample (P = .051) (Table 3). Reclassification of individuals from one risk category to another upon inclusion of albumin in the REGICOR score is shown in the .
Improvement in the Predictive Capacity of the REGICOR Risk Score for Coronary Events Upon Inclusion of Plasma Albumin Concentration: Discrimination and Reclassification
| Discrimination | C statistic (95%CI) | P |
|---|---|---|
| With classic risk factors | 79.80 (75.82-83.79) | |
| With classic risk factors + albumin | 79.94 (75.70-84.17) | |
| Difference | 0.14 (–1.19 to 1.46) | 0.841 |
| Reclassification | Estimator (95%CI) | P |
|---|---|---|
| Continuous NRI | 37.29 (6.25-67.00) | .018 |
| Categorical NRI | 13.79 (–0.08 to 27.66) | .051 |
| Case patients | 11.79 (–0.43 to 24.01) | .059 |
| Control participants | 2.00 (–0.47 to 4.47) | 0.113 |
| Clinical NRI | 32.30 (0.29-64.31) | .048 |
| Case patients | 19.30 (–2.60 to 41.21) | .084 |
| Control participants | 13.00 (–2.04 to 28.04) | .090 |
95%CI, 95% confidence interval; NRI, net reclassification improvement.
In this study, we found that plasma albumin concentration was inversely and independently associated with the risk of a coronary event. Moreover, the inclusion of plasma albumin improved the predictive capacity of the REGICOR score, thus improving risk category classification, especially of individuals with intermediate risk. The 25-OH-vitamin D, apopA1, and apoB concentrations and the apopA1:apoB ratio showed no independent association with the risk of coronary events.
Albumin and Cardiovascular RiskThe findings presented here reinforce the results of several studies analyzing the influence of albumin on coronary and cardiovascular risk and total mortality. A 1998 meta-analysis of data from 8 studies already confirmed the association between low albumin concentrations and an elevated risk of coronary disease.11 This association was also later reported in large epidemiological studies, such as ARIC21 and Framingham.22 A recent study concluded that low albumin concentration explains 41% of the attributable population risk for a first acute myocardial infarction.23 Low albumin concentration is also associated with cardiovascular diseases such as stroke24 and with total cardiovascular risk.25 Moreover, as far back as 1989, the British Regional Heart Study reported higher cardiovascular mortality in men with low systemic albumin concentrations. 26 These results have been confirmed in male participants in the Paris Health Study27 and the National Health and Nutrition Examination Survey I,28 but not in other studies.29
There is no consensus on whether albumin concentration is simply a nonspecific variable or is causally involved in cardiovascular disease.30 However, the relationship could be explained by several biological properties of albumin: a) Albumin has antioxidant and anti-inflammatory properties and accounts for more than 50% of total plasma antioxidant activity due to its free–radical-binding sulfhydryl groups.31 Moreover, albumin-bound bilirubin inhibits lipid peroxidation,32 and albumin interacts with factors that regulate the intensity of arterial inflammation.33b) Albumin transports free fatty acids and free cholesterol and participates in reverse cholesterol transport.34c) Albumin inhibits endothelial apoptosis and improves endothelial function.35 Nevertheless, the association between albumin and cardiovascular risk appears not to be very specific, since low albumin concentrations are also associated with noncardiovascular death and cancer.36
In this study, we have provided the first evaluation of albumin as a predictive risk biomarker. We found that inclusion of plasma albumin concentration in the REGICOR score improved the estimation of coronary risk and appropriately reclassified a significant proportion of the study population. The magnitude of the reclassification was higher than that observed with other biochemical biomarkers7 or with genetic biomarkers,6 and was similar to that obtained with intracoronary calcium.9 These results support the usefulness of albumin as a predictive biomarker of coronary risk. Nevertheless, confirmation is needed in other cohort studies, which should also analyze the predictive capacity of simultaneously considering different types of biomarkers.
Apolipoprotein A1/B Ratio and Cardiovascular RiskThe second biomarker analyzed in this study was the apoA1:apoB ratio. Several prospective studies have reported an association between the occurrence of coronary events and this ratio, sometimes expressed inversely as the apoB:apoA1 ratio.10,37 In the INTERHEART study,38 the aopB:apoA1 ratio was the biomarker associated with the highest population attributable risk, and apoB was identified as a more precise cardiovascular risk biomarker than non–HDL-cholesterol.39 In the present study, the apoA1:apoB ratio showed an inverse association with coronary risk, but this association disappeared after adjustment for conentional risk factors (total cholesterol and HDL cholesterol).
Given the lack of association with coronary risk, we did not analyze the influence of apoA1:apoB ratio on the predictive capacity of a conventional risk score. A previous study reported that inclusion of the apoA1:apoB ratio slightly improved the discriminatory capacity and reclassification of risk scores containing total cholesterol and HDL cholesterol.10
Vitamin D and Cardiovascular RiskVitamin D is much more than a simple regulator of calcium and phosphorus metabolism, and is linked to many cardiovascular risk factors, including dyslipidemia, hypertension, and diabetes.40–42 Nevertheless, the relationship between vitamin D concentration and coronary risk is highly controversial; although epidemiological studies indicate an association with lower cardiovascular risk,43 vitamin D supplementation in experimental studies has not demonstrated a cardioprotective effect.44 In the present study, the association of vitamin D concentration with reduced coronary risk disappeared after adjustment for conventional risk factors. Given the lack of an association with coronary events, we did not analyze the contribution of vitamin D concentration to the predictive capacity of a conventional risk score; however, where an association with cardiovascular risk has been observed, inclusion of vitamin D concentration did not improve risk prediction.43
Strengths and LimitationsThe strengths of this study include its prospective design and its population base, together with the evaluation of several biomarkers for their predictive association with coronary events.
Study limitations include the small number of coronary events, which limits the statistical power of the study. It should also be noted that vitamin D is subject to seasonal variations that may have influenced the results obtained.45 However, re-evaluations took place at all times of the year, so a seasonal effect would seem unlikely.
CONCLUSIONSPlasma albumin concentration was inversely and independently associated with the risk of coronary events, and its inclusion improved the predictive capacity of the REGICOR risk score in the general population. Niether vitamin D concentration nor apoA1:apoB ratio showed an association with the incidence of coronary events independently of conventional risk factors. Larger population studies are needed to confirm these findings.
FUNDINGThis study was supported by the Spanish Ministry of Economy and Innovation through the Carlos III Health Institute and the European Regional Development Fund (Red de Investigación Cardiovascular RD12/0042, FIS 99/0655, FIS 94/0540, FIS 99/0013-01, FIS 99/9342, FIS PI020471, INTRASALUD PI11/01801, CIBER [Centro de Investigación Biomédica en Red] de Enfermedades Cardiovasculares, CIBER de Fisiopatología de la Obesidad y Nutrición, and CIBER de Epidemiología y Salud Pública), a grant from the Spanish Society of Cardiology-Fundación Española del Corazón-Fuente Liviana 2011, and the Agència de Gestió d’Ajuts Universitaris i de Recerca (SGR 2014-1195). I.R. Degano received funding from the “la Caixa” RecerCaixa social program (RE087465). M. Grau was supported by a contract from the Carlos III Health Institute and the European Regional Development Fund (FIS CP12/03287).
CONFLICTS OF INTERESTNone declared.
- –
Cardiovascular risk estimation is essential for defining the intensity of preventive intervention appropriate for each individual.
- –
Conventional risk scores have been validated but lack sensitivity.
- –
The inclusion of new biomarkders in risk scores could improve their predictive capacity.
- –
Potential biomarkers of interest are the circulating concentrations of albumin, apoA1, apoB, and 25-OH-vitamin D.
- –
Plasma albumin concentration was inversely and independently associated with the risk of coronary events.
- –
Inclusion of plasma albumin concentration in the REGICOR risk score improved its predictive capacity, resulting in improved classification, especially among those at intermediate risk.
.
The authors gratefully acknowledge the contribution of the REGICOR study investigators and participants.