Acute aortic syndrome (AAS) is a rare condition associated with high mortality.1
The Aorta Code project was designed to create a dedicated health care network for patients with AAS. The project had 3 main goals: to increase vigilance and improve the diagnosis of AAS, to expedite the transfer of patients to the network's aortic referral center, and to provide optimal treatment through a highly specialized team.
The Aorta Code network is formed by 4 hospitals from the autonomous community of Madrid and the area's medical emergency response service (SUMMA-112). It provides coverage to a population of 1.04 million inhabitants.
The project set-up included specialized training at the hospitals’ emergency departments and SUMMA-112 and the development of a diagnostic and a treatment algorithm based on clinical practice guidelines.2 A highly specialized AAS care team formed by 2 cardiologists, 2 cardiac surgeons, and 2 vascular surgeons (the Aorta Team) was created to take responsibility for decisions on incoming patients and their treatment. The project was approved by the relevant health authorities in Madrid and the local ethics committee at Hospital Clínico San Carlos. Informed consent was obtained from all patients involved.
The full Aorta Code protocol has been published elsewhere.2 In brief, as soon as a patient is diagnosed with AAS, the emergency responders activate the Aorta Code via a dedicated telephone line. The coordination committee at SUMMA-112 dispatches a unit for the urgent transfer of the patient to the referral hospital, where their case is assessed by the members of the Aorta Team, who decide on the definitive treatment.
To evaluate the Aorta Code project, we compared outcomes from the 18 months before the project was implemented (care-as-usual period) with outcomes from the first 2 years of its implementation (March 15, 2019 to March 15, 2021).
Categorical variables are expressed as number and percentage and were compared using the chi-square or Fisher exact test. Quantitative variables are expressed as mean±standard deviation or median [interquartile range] and were compared using the t test. Statistical significance was set at P < .05 and the statistical analyses were performed in STATA (version 12.0).
The AAS code was activated 59 times during the 2 years analyzed (this included a 3-month period in which the service was interrupted due to the COVID-19 pandemic). AAS was confirmed in 42 patients (table 1); 5 patients did not have aortic disease, 8 had nonacute aortic disease, and 4 had a ruptured abdominal aortic aneurysm.
Baseline and presenting characteristics of patients with acute aortic syndrome during care-as-usual and after implementation of the Aorta Code project
| Variable | Aorta Code (n=42) | Care-as-usual (n=18) | P |
|---|---|---|---|
| Age, y | 67.1±2.2 | 63.4±4.3 | .403 |
| Male sex | 57.1% (24) | 77.8% (14) | .129 |
| Diagnosis | |||
| Aortic dissection | 80.9% (34) | 77.8% (14) | .720 |
| Hypertension | 17.1% (7) | 22.2% (4) | |
| DTTA rupture | 2.4% (1) | 0 | |
| Type | |||
| A | 73.8% (31) | 77.8% (14) | .745 |
| B | 26.8% (10) | 22.2% (4) | |
| Risk factors | |||
| Hypertension | 76.2% (32) | 55.6% (10) | .169 |
| Diabetes mellitus | 7.2% (3) | 5.6% (1) | .821 |
| Hypercholesterolemia | 45.2% (19) | 22.2% (4) | .172 |
| Smoking | 28.6% (12) | 27.8% (5) | .950 |
| COPD | 11.9% (5) | 5.6% (1) | .453 |
| Chronic kidney failure | 2.4% (1) | 5.6% (1) | .530 |
| Aortic aneurysm | 5.4% (2) | 11.1% (2) | .445 |
| Signs, symptoms, and complications on admission | |||
| SBP, mmHg | 134.6±6.5 | 132.3±8.8 | .840 |
| Chest pain | 80.5% (33) | 88.9% (16) | .428 |
| Syncope | 19.1% (8) | 11.1% (2) | .450 |
| Neurological deficit | 16.7% (7) | 27.8% (5) | .324 |
| Pulse deficit | 19.1% (8) | 22.2% (4) | .778 |
| Peripheral ischemia | 12.8% (5) | 27.8% (5) | .168 |
| Acute kidney failure | 15.8% (6) | 22.2% (4) | .557 |
| Myocardial infarction | 12.8% (5) | 11.1% (2) | .855 |
| Shock | 23.1% (9) | 16.7% (3) | .581 |
| Tamponade | 19.5% (8) | 16.7% (3) | .796 |
| Need for intubation | 7.5% (3) | 5.6% (1) | .787 |
| Other studies | |||
| Normal electrocardiogram | 52.4% (22) | 61.1% (11) | .533 |
| Normal chest radiograph | 7.3% (3) | 5.88% (1) | .844 |
| Hemopericardium | 28.6% (12) | 33.3% (6) | .712 |
| Pleural effusion | 23.8% (10) | 23.5% (4) | .982 |
| Hemomediastinum | 14.3% (6) | 18.8% (3) | .675 |
| Hemothorax | 7.2% (3) | 0% (0) | .550 |
| Periaortic hematoma | 31% (13) | 29.4% (5) | .907 |
| Supraortic branch involvement | 48.8% (20) | 58.8% (10) | .486 |
| True lumen compression | 60% (21) | 43.8% (7) | .279 |
| Renal artery involvement | 48.8% (20) | 35.3% (6) | .347 |
| D-dimer level, ng/mL | 7187 (4230-54 411) | 6817 (2390-49 739) | .871 |
| Maximal aortic diameter, mm | 50.3±2 | 51±3.3 | .836 |
| Maximal AIH thickness, mm | 12±1.4 | 17.4±4.9 | .197 |
AIH, aortic intramural hematoma; COPD, chronic obstructive pulmonary disease; DTAA, descending thoracic aortic aneurysm; SBP, systolic blood pressure.
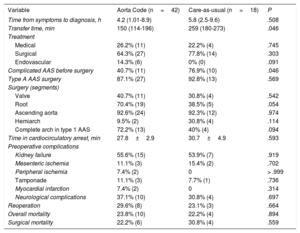
Following the implementation of the Aorta Code project, the number of patients diagnosed with AAS doubled (from a mean of 1 patient a month to 2 patients a month). No significant differences were observed between the groups for the presence of risk factors, imaging findings, or clinical presentations (table 1). Transfer times to the hospital were also significantly reduced (table 2). There were no significant differences between the groups for time from first symptom to diagnosis or time from diagnosis to surgery. Preoperative AAS complication rates also decreased (table 2).
Treatment and prognosis of patients with acute aortic syndrome during care-as-usual and after implementation of the Aorta Code project
| Variable | Aorta Code (n=42) | Care-as-usual (n=18) | P |
|---|---|---|---|
| Time from symptoms to diagnosis, h | 4.2 (1.01-8.9) | 5.8 (2.5-9.6) | .508 |
| Transfer time, min | 150 (114-196) | 259 (180-273) | .046 |
| Treatment | |||
| Medical | 26.2% (11) | 22.2% (4) | .745 |
| Surgical | 64.3% (27) | 77.8% (14) | .303 |
| Endovascular | 14.3% (6) | 0% (0) | .091 |
| Complicated AAS before surgery | 40.7% (11) | 76.9% (10) | .046 |
| Type A AAS surgery | 87.1% (27) | 92.8% (13) | .569 |
| Surgery (segments) | |||
| Valve | 40.7% (11) | 30.8% (4) | .542 |
| Root | 70.4% (19) | 38.5% (5) | .054 |
| Ascending aorta | 92.6% (24) | 92.3% (12) | .974 |
| Hemiarch | 9.5% (2) | 30.8% (4) | .114 |
| Complete arch in type 1 AAS | 72.2% (13) | 40% (4) | .094 |
| Time in cardiocirculatory arrest, min | 27.8±2.9 | 30.7±4.9 | .593 |
| Preoperative complications | |||
| Kidney failure | 55.6% (15) | 53.9% (7) | .919 |
| Mesenteric ischemia | 11.1% (3) | 15.4% (2) | .702 |
| Peripheral ischemia | 7.4% (2) | 0 | > .999 |
| Tamponade | 11.1% (3) | 7.7% (1) | .736 |
| Myocardial infarction | 7.4% (2) | 0 | .314 |
| Neurological complications | 37.1% (10) | 30.8% (4) | .697 |
| Reoperation | 29.6% (8) | 23.1% (3) | .664 |
| Overall mortality | 23.8% (10) | 22.2% (4) | .894 |
| Surgical mortality | 22.2% (6) | 30.8% (4) | .559 |
AAS, acute aortic syndrome.
Complicated AAS: occurrence of any of the following complications before surgery for AAS: poor perfusion, kidney failure, myocardial infarction, tamponade, shock, and neurological complications.
The number of surgeons treating patients diagnosed with AAS fell from 13 (7 cardiac and 6 vascular surgeons) during care-as-usual to 4 (2 cardiac and 2 vascular surgeons) during the project. Sixty percent of patients with type A AAS were treated with the Bentall-De Bono procedure during the care-as-usual period. This percentage fell to 42% after implementation of the project, as 58% were treated with aortic root repair surgery. There was also a relative increase of 80% in the number of complete aortic arch procedures performed (P=.09) (table 2). The project achieved a relative reduction of 28% in surgery mortality rates compared with care-as-usual, although the difference was nonsignificant (risk difference, 8.5%; odds ratio=0.64; 95% confidence interval, 0.15-2.6; P=.559). There were no differences between the groups in overall mortality.
The clinical presentation of AAS is variable and often leads to diagnostic errors.3 Implementation of the Aorta Code project improved the knowledge and skills of emergency service physicians and increased the number of AAS diagnoses. Although management of acute aortic disease by a small team of dedicated surgeons at a limited number of specialized centers has been found to improve survival outcomes,4 our project is the first of its kind to be implemented in Spain. The Aorta Code project has had 2 main effects: a) it has increased the complexity of surgical procedures (by assigning all interventions to just 2 surgeons) and b) it has reduced surgical mortality rates, although the difference with care-as-usual was not significant due to the small sample. Extending surgical repair to include the aortic arch and root increases complexity, but performance of this surgery by an expert team of surgeons in carefully selected patients does not increase in-hospital morbidity or mortality and reduces the need for reoperation in the mid- to long-term, thereby improving prognosis.5
In conclusion, a) the creation of a health care network for patients with AAS is feasible and requires the extensive involvement of emergency departments and response services and the creation of a team of experts in aortic conditions, b) the Aorta Code project has improved the diagnosis of AAS and shortened transfer times to the referral hospital, and c) the performance of AAS surgery by a small team of highly specialized surgeons has improved outcomes.
FundingNo funding was received for this study.
AUTHORS’ CONTRIBUTIONSC. Ferrera, I. Vilacosta, P. Busca, A. Martín Martínez, F.J. Serrano, and L. Maroto Castellanos contributed significantly to the collection and interpretation of data. C. Ferrera analyzed the data. C. Ferrera and I. Vilacosta wrote the first version of the manuscript. All the authors revised the full manuscript and approved its final version. All the authors agree on the content of the article and guarantee the veracity and accuracy of all parts of this study. The authors declare that they are responsible for the content of this study.
Conflicts of InterestNone.
Julián Pérez Villacastín, Marian Bas, Christian Bengoa, Ana Cortés Martínez, J. Alberto García Lledó, Inmaculada Fernández Rozas, Alejandro Curcio, and Carlos Macaya.
Carlos Ferrera, Ana Carrero, Alfonso Martín, Francisco Javier Martín Sánchez, María Jesús Domínguez García, Pablo Busca, Fátima Fernández Salgado, Isaac Martínez, Javier Cobiella, Francisco Javier Noriega, Ana Viana Tejedor, Francisco Javier Serrano Hernando, Luis Carlos Maroto Castellanos, Isidre Vilacosta.