To the Editor,
The prevalence of arrhythmogenic right ventricular dysplasia (ARVD) varies widely according to the series and the geographical area, and accounts for 5% of all sudden deaths in patients <65 years old.1 This condition is an autosomal dominant disease with variable penetrance and incomplete expression. A higher prevalence is observed in men, and a family history is found in about 30% of patients.2 The mean age at diagnosis is around 30 years, whereas presentation in patients >65 years old is rare.
We describe the case of a 76-year-old man with a history of benign prostatic hyperplasia, but no cardiovascular risk factors. The family history included death of 2 brothers at age 50 and 60 due to uncertain causes, as well as death of a sister at age 11, also for unknown reasons; two of the patient's sons had died accidentally. The patient consulted for mid-chest discomfort, dizziness, and palpitations; the electrocardiogram showed regular, monomonphic wide QRS complex tachycardia and a left bundle-banch block morphology. Tachycardia persisted following administration of intravenous amiodarone and electrical cardioversion was performed; sinus rhythm was restored with left anterior bundle-branch block and negative T-waves in V2 and V3.
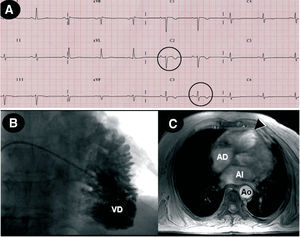
The echocardiogram showed good function of the left ventricle (LV) and dysfunction of the right ventricle (RV) with dilation (43 mm), but no valve abnormalities or evidence of pulmonary hypertension (Figure 1A). Catheterization revealed RV dilation and considerable trabeculation with a "stack of coins" image, as well as normal pulmonary pressure; the LV and coronary arteries were normal (Figure 1B). Magnetic resonance imaging (Figure 1C) showed RV dilation with an area of apical dyskinesia and wall thinning. Holter monitoring disclosed 352 premature ventricular beats, with no episodes of ventricular tachycardia (VT). An electrophysiological study performed after intravenous amiodarone for several days showed ventricular electric stability.
Figure 1. A: baseline electrocardiogram shows negative T waves in V2 and V3 (circles). B: right ventriculography discloses dilation of the right ventricle (RV) and "stack of coins" image. C: magnetic resonance image showing apical aneurysm (arrow).
Based on the presence of diagnostic criteria for ARVD,2 the patient was diagnosed with this condition, and because he had experienced VT while under amiodarone therapy, a single-chamber defibrillator was implanted.3 He subsequently had episodes of paroxysmal atrial fibrillation that triggered inappropriate discharges and in the following months, presented VT that was controlled with sotalol 160 mg/day.
A search of the Medline database (National Library of Medicine, Bethesda, MD) found 5 cases of ARVD among the elderly4-7; all of these patients had died and were diagnosed by histology (Table). One patient was diagnosed at 72 years, although he had presented a history of VT from age 45.4 The mean patient age was 75.8 years; 4 were men and 2, women. None of the cases mentioned a family history, except for the present case. Four had presented VT, one of them polymorphic VT,5 which, even though it is not the characteristic type, has been described in some cases of ARVD. The most frequent electrocardiographic findings were negative T-waves in the right precordials (V2 and V3), and in two cases, epsilon waves.7
New pharmacological therapies, radio frequency ablation, and defibrillators3 will probably have a favorable impact on the survival of these patients and will make it not unlikely to see elderly patients with ARVD. The possibility of a late onset of the disease should also be suspected. A two-chamber defibrillator in these patients could improve the diagnosis of supraventricular arrhythmias, because they are elderly patients in whom the prevalence of atrial fibrillation is increased and because inappropriate therapies for supraventricular tachyarrhythmia may be more common among patients with ARVD.8