We describe a male patient born in June 1965. His parents are first cousins, he is their second and last child, and he has no descendants. At the age of 33 years, the patient experienced palpitations, and the episode was diagnosed as atrial fibrillation with rapid ventricular response. At that time, he started to be studied at the cardiology service, where he was also diagnosed with dyslipidemia, hypertension, hypertensive cardiomyopathy, and mild aortic regurgitation with a tricuspid aortic valve. Physical examination revealed the presence of palpebral bilateral ptosis, hypertelorism, and long face. In addition, the patient has multiple diseases requiring follow-up by other specialties. These diseases include high bilateral myopia, producing left-eye blindness due to retinal detachment, chronic bilateral otitis media requiring bilateral tympanoplasty, and erectile dysfunction, as well as depressive disorder and hip and elbow osteoarthritis, requiring bilateral hip replacement at the age of 50 years. The patient was also diagnosed with nonallergic moderate bronchial asthma and hemochromatosis with a C282Y mutation in the HFE gene with no liver injury. At the age of 41 years, after an accidental fall, he experienced generalized onset tonic-clonic seizures, classified as “posttraumatic”.
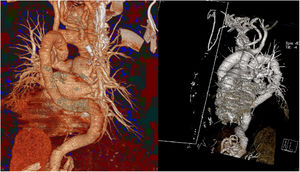
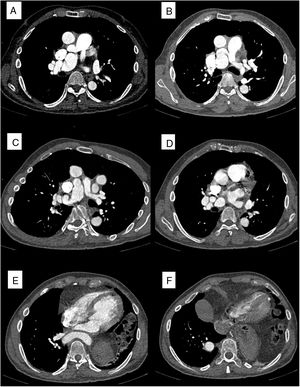
When the patient was 52 years old, during cardiologic check-up, he reported that he was asymptomatic and that he had not had any new palpitation episodes. Echocardiography showed moderate to severe aortic regurgitation and a nondilated left ventricle with moderate septobasal hypertrophy (15 mm). Although the patient was 120mg verapamil every 12hours, during the examination we observed asymmetric blood pressure (171/80 on the right arm, 147/78 on the left arm). This asymmetry had not previously been diagnosed; therefore, aortic computed tomography angiography was requested to rule out coarctation of the aorta. The computed tomography angiogram showed a tortuous ascending aorta with looping (figure 1 and figure 2). The origin of the 3 supra-aortic trunks is located in the first ascending section of the aorta. The descending section of the looping seems anatomically related to the point of attachment of the ligamentum arteriosum. The descending aorta is also tortuous and crosses the midline to go through a right intrapulmonary trajectory. This right trajectory seems to be the consequence of a left diaphragmatic hernia. No aneurysm or significant stenosis in the aorta were identified. The 2 pulmonary branches showed substantial tortuosity. In the right pulmonary artery, we observed an aneurysm and the cluster of vessels sign.
Two-dimensional computed tomography angiogram showing A: origin of pulmonary branches and the cluster of vessels sign in the right pulmonary artery. B: tortuous left pulmonary artery. C: aneurysmal lesion of the right pulmonary artery. D: tortuous right pulmonary artery. E: descending aorta crossing the midline. F: right intrapulmonary trajectory of the descending aorta.
These findings led us to suspect arterial tortuosity syndrome (ATS). Consequently, we requested a genetic analysis of the SLC2A10 gene. This test revealed a homozygous c. 1333 of G:p.G445fs deletion. This mutation could lead to a premature stop codon, which could produce either a decrease in ribonucleic acid or a truncated protein with a 10% loss of amino acids. Since it has not been previously described, this mutation should be considered as likely pathogenic for ATS; however, for c.1334, adjacent pathogenic mutations have been previously diagnosed.1
One year after the diagnosis of ATS, the patient was still asymptomatic from a cardiovascular perspective. He originally rejected an imaging test to rule out vascular malformations at other anatomical sites, mainly the brain. So far, no surgical procedure has been performed due to the absence of severe vascular stenosis or a clinically relevant aneurysm. Therefore, follow-up has been arranged, consisting of periodic repetition of computed tomography angiography and/or magnetic resonance imaging scan. We suggested performing a genetic study on his living first-degree relatives (mother and brother), who also initially refused to be studied.
ATS is a rare connective tissue disorder, which is typically transmitted in an autosomal recessive manner. It is characterized by elongated and tortuous large-sized arteries, together with a strong tendency for dissection and aneurysm formation in the major arteries. ATS also shows additional dysmorphic features and other alterations typically associated with connective tissue disorders, such as cutaneous hyperextensibility and diaphragmatic hernia. ATS is typically described in pediatric patients.2 Our case has certain special characteristics. First, the patient was diagnosed at an unusually late age. This allows us to add some information to this disease, whose development is scarcely known in adulthood. So far, few cases have been diagnosed in adults and, as far as we know, the oldest patient with ATS molecularly confirmed through genetic testing was 51 years old at the moment of confirmation.3 The only adult diagnosed when older than 51 years was aged 67 years. Although that patient had features reminiscent of ATS, he lacked molecular characterization.4
Regarding the clinical course in our patient, extensive comorbidity was observed, requiring thorough follow-up mainly at the services of cardiology, ophthalmology, otorhinolaryngology, traumatology, and hematology. In addition to typically described cardiovascular manifestations such as left ventricular hypertrophy and valvular regurgitation, we also observed atrial fibrillation, which is very rarely described in this syndrome.2 Finally, the description of a new mutation associated with ATS (c.1333del G:p.G445fs) is notable and, at the time of writing, should be considered as likely pathogenic.