Keywords
INTRODUCTION
The long-term development of left ventricular dysfunction is a major concern in the management of patients with chronic severe mitral valve regurgitation.1-4 In the preoperative period alterations in myocardial contractility may be 'invisible' with the traditional methods used to assess systolic function, a consequence of the loading conditions present. Mitral regurgitation provides a low impedance alternative for left ventricular ejection, and increases the left ventricular ejection fraction (LVEF).5,6 The early detection of deteriorating systolic function in patients with chronic mitral regurgitation, and thus the ability to identify the most appropriate moment for surgery, remains a challenge to physicians.
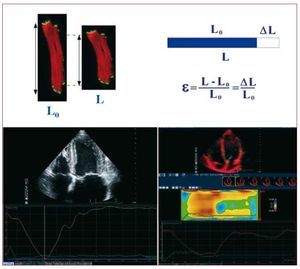
The analysis of myocardial deformation has recently emerged as a quantitative means of reliably estimating myocardial contractility. The strain represents the percentage shortening of the myocardial fibers (Figure 1), while the strain rate, which represents the speed of myocardial deformation, is derived as a function of strain and time. The main advantage of this method over those that analyze myocardial displacement is that it differentiates between active contraction and the passive movement resulting from the general translation of the heart or through the traction of neighboring myocardial regions. In the assessment of left ventricular function it is therefore less dependent on the load than traditional methods.
Figure 1. The strain represents the percentage shortening of the myocardial fibers in systole. Lower left: strain determined by speckle-tracking. Lower right: strain obtained by tissue Doppler. DL: change in length; L: Final length; Lo: Initial length; S: strain.
There are currently 2 ways to assess myocardial deformation: tissue Doppler (TD) and a new method known as speckle-tracking (ST). The latter is not based on Doppler analysis but on the following of bright points via gray scale analysis (Figure 1). In a prior study performed by our group, speckle-tracking was shown to be valuable in predicting the deterioration of the LVEF in the immediate postoperative period in patients who had undergone surgery for chronic severe mitral valve regurgitation.7 However, a number of factors can influence the LVEF during this period, such as the hemodynamics of the patient, changes in loading, post-surgical myocardial contusion, and septic states etc. The aim of the present work was to determine the value of analyzing the longitudinal myocardial deformation of the left ventricle using speckle-tracking and TD for predicting the medium term deterioration of the LVEF in patients who have undergone surgery for chronic severe mitral valve regurgitation.
METHODS
The study subjects were 38 consecutive patients scheduled to undergo mitral valve replacement at the Hospital Clínico San Carlos for chronic severe mitral valve regurgitation owing to organic disease of the mitral valve. All 38 patients were prospectively included between December 2006 and October 2007. Patients with ischemic heart disease, cardiomyopathy, significant aortic valve disease, mitral stenosis worse than mild, or congenital heart disease were excluded, as were those who declined to participate. Four patients were excluded from the sample since they could not be located six months before their operation; the final sample was therefore composed of 34 patients. No patient was excluded because of a poor acoustic window.
Echocardiography
The longitudinal strain and strain rate of the basal and mid interventricular septum were determined by TD and speckle-tracking in the apical four-chamber plane.8,9 The ultrasound beam was aligned as best as possible with the interventricular septum. Speckle-tracking images were obtained at a frame rate of 80 or 100 frames per second (fps); TD images were obtained at >150 fps. An IE33 apparatus with an S5 probe (Philips, Andoven, Massachusetts) was used for all tests. Two cycles were recorded in patients with sinus rhythm, and the mean results determined. The mean result of three cycles was determined in patients with atrial fibrillation. The pre- and postoperative LVEF was obtained by three dimensional echocardiography using the complete volume technique.10 The study subjects were then divided into 2 groups: those with a reduction in LVEF of ≤10% at 6 months (Group 1), and those with a reduction of >10% at 6 months (Group 2).
Mitral regurgitation was quantified by measuring the proximal isoconvergence area (PISA) and the effective regurgitant orifice. The pressure/ time derivative (Dp/Dt) for the left ventricle was obtained by continuous spectral Doppler monitoring of the mitral regurgitation flow in the apical 4-chamber plane. The echocardiographic studies were performed 48 h before surgery and 6 months after surgery. Images were stored on a magneto-optical disc or a compact disc, and analyzed off-line using Q-lab software (Philips, Andoven, Massachusetts).
Statistical Analysis
Quantitative variables were expressed as means (standard deviation); qualitative variables were expressed as absolute values and percentages. The normal distribution of variables was examined using the Kolmogorov-Smirnov test. Differences between groups were analyzed using the Student t test (quantitative variables) or the χ2 test (qualitative variables). The Student t test for paired samples was used to examine the change in quantitative variables. Linear regression was used to study the correlation between continuous variables. Logistic regression analysis was used to analyze the predictors of deterioration of the LVEF by >10% at six months. Receiver operating characteristic (ROC) curves (with the corresponding area under them) were plotted to determine the optimum cut-off for predicting the deterioration of the LVEF. Significance was set at P<.05. All calculations were made using SPSS v.15.0 software.
RESULTS
The mean age of patients was 59.9 (11.3) years; 10 patients (29.4%) were male. The etiology of the mitral regurgitation was rheumatic in 19 patients (55.9%), degenerative in 14 (41.2%), and secondary to cured endocarditis in 1 (2.9%). Twenty-five patients (73.5%) were in atrial fibrillation; the rest were in sinus rhythm. A bioprosthesis was used in 2 patients (5.9%) and a metallic prosthesis in 32 (94.1%). The surgical procedure included the conservation of the subvalvular apparatus in all cases. The mean LVEF fell from 62.46% (8.4%) before surgery to 56.08% (12.9%) at 6 months after surgery (P<.001). In Group 1, the LVEF fell from 62.6% (7.2%) before surgery to 61.7% (7%) at 6 months after surgery (P=.38), while in Group 2 it fell from 62.2% (10.6%) before surgery to 45.7% (15%) at 6 months after surgery (P<.001). The comparison of these results with those for the immediate postoperative period reported in a recently published study7 suggests a discrete and non-significant improvement in the LVEF between the immediate post-surgery and 6 month post-surgery time points, rising from 54.6% (13.6%) to 56.1% (12.9%) (P=.23).
Table 1 shows the baseline characteristics of the 2 groups. Significant differences were seen in ventricular volume and Dp/Dt. No significant differences were seen in any of the variables recorded, although there was a trend towards more severe mitral regurgitation in Group 2.
Values for the longitudinal strain and strain rate of the basal and mid interventricular septum were obtained by both speckle-tracking and TD. Table 2 shows the results of the analysis of myocardial deformation; Table 3 shows the results of the logistic regression analysis. The peak longitudinal strain and strain rate of the interventricular septum obtained by speckle-tracking were very good predictors of a deterioration of the LVEF by >10% at 6 months, and showed a higher predictive value than the corresponding TD measurements. The preoperative dimensions of the left ventricle and the Dp/Dt showed a trend towards being able to predict the deterioration of the LVEF, but did not reach statistical significance.
Table 4 and Figure 2 show the ROC curve results. The area under the curve for the speckle-tracking method was greater than that obtained with TD. The longitudinal strain of the basal septum measured by speckle-tracking was the variable with the best general predictive power; the area under the curve was 0.85 (0.72-0.94) and the optimum cut-off point -0.11 (sensitivity 58.3%, specificity 95.4%, positive predictive power 87.5%, negative predictive power 80.7%).
Figure 2. ROC curves for the different methods for predicting a deterioration in the LVEF of >10% at 6 months. Dp/Dt: derived from pressure/time for the left ventricle; TD: Tissue Doppler; LVEF: left ventricular ejection fraction; IVS: interventricular septum; SR: strain rate; ST: speckle-tracking; EDV: end-diastolic volume; ESV: end-systolic volume.
Table 5 shows the results of the linear regression analysis with respect to the correlation of the different variable studied and the degree of deterioration of the LVEF at 6 months after surgery. The speckle-tracking results showed a good linear correlation with the fall in LVEF, better than that obtained with TD and traditional variables (Table 5, Figures 3 and 4).
Figure 3. Correlation of speckle-tracking results with deterioration of LVEF at six months. Dp/Dt: derived from pressure/time for the left ventricle; LVEF: left ventricular ejection fraction; IVS: interventricular septum; SR: strain rate; ST: speckle-tracking.
Figure 4. Correlation of TD results with deterioration of LVEF at six months. Dp/Dt: derived from pressure/time for the left ventricle; TD: Tissue Doppler; LVEF: left ventricular ejection fraction; IVS: interventricular septum; SR: strain rate.
DISCUSSION
In patients with chronic severe mitral regurgitation, the deterioration of myocardial contractility can be "invisible" to the traditional methods used to assess systolic function, a consequence of the loading conditions present. Mitral regurgitation provides an alternative, low impedance route for left ventricular ejection, increasing the LVEF. Sometimes, contractile dysfunction can only be "unmasked" with a change in the loading conditions following surgery, when left ventricular dysfunction and postoperative congestive heart failure appear. The identification of contractile dysfunction in its early phases, and its surgical correction, could avoid the development of irreversible left ventricular dysfunction in the postoperative period.
Despite adhering to current clinical guidelines, the incidence of postoperative ventricular dysfunction in patients with the present condition is notable—a problem that worsens their short- and long-term prognoses.1-4 These guidelines recommend close monitoring of such patients until symptoms—left ventricular dilatation, systolic dysfunction, pulmonary hypertension, or atrial fibrillation11—occur. However, these symptoms can be masked owing to their insidious appearance and slow course, and the interpretation of systolic function is difficult in patients with mitral regurgitation due to loading changes.
The risk of postoperative ventricular dysfunction is notably increased in patients with a reduced preoperative LVEF or who already show symptoms.12 This observation, in combination with the excellent results achieved in valve repair, 13,14 has led many researchers to propose surgical correction with the aim of preserving contractile function and improving long-term prognosis.15,16 Enríquez-Sarano et al15 showed patients with an effective regurgitant orifice of >40 mm2 to have a poor prognosis with medical treatment alone despite the absence of symptoms. Timely surgery should therefore be contemplated in such patients.
The early detection of a deterioration in contractile function in patients with chronic severe mitral regurgitation is a great challenge to physicians. A precise and reproducible echocardiographic technique is required for identifying anomalies in myocardial contractility that cannot be detected simply, the aim being to identify the best moment at which to perform surgery. The echocardiographic methods proposed to date for detecting latent systolic dysfunction in these patients17-22 have limitations that reduce their usefulness in daily clinical practice5; neither have they become consolidated in current practice for this end, nor do they appear in clinical guidelines referring to mitral regurgitation.11
The analysis of myocardial deformation allows myocardial contractility to be precisely measured. Weidemann et al23 showed that the strain rate obtained by TD was strongly related to myocardial contractile function. Recently, Lee et al8 showed that the TD-measured strain rate can detect subclinical ventricular dysfunction in asymptomatic patients with severe mitral regurgitation. The main limitation of TD measurements is their dependence on the angulation of the ultrasound beam. Precise measurements can only be taken when the main movement vector is parallel to the ultrasound beam. The speckle-tracking technique, however, affords certain advantages over DT.9,24 Firstly, it makes direct measurements of myocardial deformation while TD makes an estimate via the integral of the velocity gradient. Speckle-tracking is independent of the angulation of the ultrasound beam, which allows segments that are not linearly aligned with the beam to be analyzed. This also allows the study of the radial deformation from the apical four-chamber plane and short parasternal axis. In addition, it allows the rotational and torsional movement of the left ventricle to be studied, providing a better understanding of the latter's systolic function. The measurements are not affected by the translation movement of the myocardium, and the results of speckle-tracking analysis are seen on-screen, allowing visual monitoring of the quality of point tracking, ensuring accurate analysis. With TD, noise can alter the measurements made without the knowledge of the operator. Speckle-tracking has been validated by comparing the values returned with those provided by sonomicrometry and magnetic resonance tagging studies, with strong correlations detected.25-30 This new method has been used successfully to detect contractile dysfunction in other conditions such as hypertrophic cardiomyopathy.31 Finally, reports exist that show intra- and interobserver variation to be less in speckle-tracking than in TD.32,33
The present study assessed the usefulness of analyzing myocardial deformation in the preoperative evaluation of systolic function in patients with chronic severe mitral regurgitation. The results show that the analysis of the longitudinal deformation of the left ventricle by speckle-tracking is a powerful tool for predicting medium term deterioration of the LVEF in patients who have undergone valve replacement for chronic mitral regurgitation. They also show that the diagnostic precision of this method is greater than that of TD and traditional methods for the analysis of systolic function.
The preoperative LVEF was found not to be a predictor of postoperative LVEF deterioration. The preoperative LVEF appears as a powerful predictor of postoperative ventricular dysfunction when reduced, but the opposite is not always true. Its sensitivity is low for the early detection of abnormalities of contractility when the LVEF is normal, and the appearance of postoperative ventricular dysfunction is frequent in patients with an apparently normal preoperative LVEF. In the present study, the preoperative LVEF was normal in both groups of patients (Group 1 = 62.6% [7.2%], Group 2 = 62.2% [10.6%]). However, the members of Group 2, in whom the LVEF had deteriorated at 6 months, showed reduced myocardial deformation in the preoperative period, showing contractility to be abnormal. In this work, no significant improvement in LVEF was seen at six months compared to recently published results for the immediate postoperative period.7 This supports the idea that surgery unmasks patients' "true" systolic function by eliminating the alternative, low impedance route for left ventricular ejection.
Given the results obtained, the study of myocardial deformation could be useful in detecting latent ventricular dysfunction in patients with chronic severe mitral regurgitation. When the values of the deformation variables start to deteriorate, surgery should be contemplated with the aim of preventing irreversible systolic dysfunction and reducing the rates of postoperative ventricular dysfunction and heart failure.
Limitations
The longitudinal deformation analysis of the left ventricle was performed only in the interventricular septum. The reason for this lies in the high quality of the images that can be obtained in this region in 2-dimensional studies. In other regions, such as the lateral face of the left ventricle, the inclusion of artifacts is greater and the reproducibility of measurements is poorer. Valve substitutions were not included, neither were mitral valve repairs, despite the fact that this surgical technique has been shown better than valve replacement in the preservation of left ventricular systolic function.12,13 However, in all patients the sub-valvular apparatus was conserved, providing a functional result similar to valve repair.34,35 Finally, no study of interobserver variation with respect to the measurement of myocardial deformation was undertaken.
CONCLUSIONS
The longitudinal myocardial deformation analysis of the left ventricle by speckle-tracking is useful for predicting the medium term deterioration of the LVEF following surgery in patients with chronic severe mitral regurgitation subjected to valve replacement. This method is invested with a diagnostic precision that is greater than that offered by TD and traditional methods of assessing systolic function. This promising method could be of use in the clinic when trying to decide upon the optimum time to schedule surgery for such patients. When myocardial deformation begins to decrease, surgery should be contemplated even though patients may show no or only very mild symptoms; this might help prevent irreversible systolic dysfunction in the long term.
ABBREVIATIONS
TDI: Tissue doppler imaging.
LEVF: left ventricular ejection fractions.
Correspondence: Dr. J.A. de Agustín.
Unidad de Imagen Cardiovascular. Hospital Clínico San Carlos. Prof. Martín Lagos, s/n. 28040 Madrid. Spain
E-mail: albertutor@hotmail.com
Received July 26, 2009.
Accepted for publication December 17, 2009.