Keywords
INTRODUCTION
Acute unilateral pulmonary edema is an unusual clinical condition. Most cases reported in the literature occur at the upper right side and are caused by severe mitral regurgitation (MR).1-3
We describe a patient who, after presenting an acute anterior myocardial infarction, developed acute right-sided unilateral pulmonary edema with no associated MR.
CASE STUDY
A 76-year-old man, ex-smoker, diabetic and hypertensive, was admitted for Killip Class I acute anterior myocardial infarction of 48 hours' evolution, with no reperfusion. The electrocardiogram revealed QS complexes in V1-V3. Peak troponin I was 99.7 ng/mL. The echocardiogram performed at admission disclosed an ejection fraction (EF) of 50% with anteroapical akinesia and mild MR.
On the fourth day of hospitalization, coronary angiography was performed to investigate post-infarction angina, showing severe three-vessel disease with good distal beds.
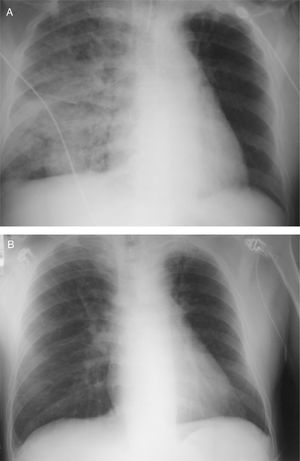
While awaiting surgery, the patient developed rapidly progressive dyspnea that required intubation and mechanical ventilation. The EF at the time was 32% with mild MR. The chest x-ray showed a pattern of acute pulmonary edema, predominantly right-sided, which resolved after diuretic treatment (Figure 1). The patient was extubated after a few hours.
Figure 1. A: pattern of right alveolar edema. B: evidence of congestion had disappeared after diuretic treatment.
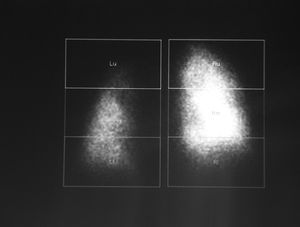
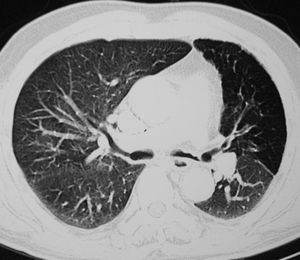
In the absence of any evidence of heart failure, a technetium-99 macroaggregated albumin perfusion scan was performed, revealing generalized hypoperfusion of the left lung, with an uptake of 29.7% versus 70.3% in the right lung (Figure 2). Chest computed tomography showed hypoplasia of the left upper pulmonary arterial tree, with apical pleural thickening and scarring changes probably related to remote tuberculosis (Figure 3).
Figure 2. Perfusion scintigraphy (posterior view) showed greater uptake in the right lung (R) than the left (L).
Figure 3. Chest computed tomography showing the small diameter of the upper branches of the left pulmonary artery.
DISCUSSION
We describe a patient who, while in the subacute phase of an anterior infarction, presented acute unilateral pulmonary edema, predominantly on the right side. The mechanism of asymmetry was identified as an imbalance in pulmonary perfusion secondary to acquired hypoplasia of the left pulmonary arterial tree, in all likelihood due to pulmonary tuberculosis.
In normal situations, perfusion of both lungs is practically equal (±5%). In the presence of a trigger (e.g., severe ischemia) that produces a sudden rise in capillary pressure, acute pulmonary edema will develop in a symmetrical manner.4
In cases of acute unilateral pulmonary edema, the differential diagnosis must be made by comparing it to other causes of alveolar congestion: unilateral pneumonia, broncoaspiration, or alveolar hemorrhaging. Most reported cases of acute unilateral pulmonary edema have resulted from severe eccentric MR. A mitral regurgitation jet affecting a pulmonary vein, predominantly on the upper right,1 can lead to a larger increase in mean capillary pressure in the right side and consequently, a greater degree of right acute pulmonary edema.2,3 On rare occasions, the asymmetrical increase in capillary pressures is caused by compression of a pulmonary vein outlet by a myxoma or atrial wall hematoma.5
Perfusion imbalance between the lungs is another source of acute unilateral pulmonary edema. The degree of edema is proportional to the degree of perfusion; hence, in cases of congenital hypoplasia or pulmonary artery agenesis, the less perfused lobes will present a lower degree of edema.6 The patient we describe, who had left pulmonary hypoperfusion due to acquired hypoplasia of the pulmonary branches, developed acute pulmonary edema in the more highly perfused contralateral (right) lung.
We believe the pathogenic mechanism should be identified in acute unilateral pulmonary edema.
ACKNOWLEDGEMENTS
To Dr. Jaume Figueras, of the Hospital Vall d'Hebron, for his insight in the search for answers to questions that come up in daily clinical practice.
Correspondence: Dr. C. Peña Gil.
Servicio de Cardiología. Hospital Clínico Universitario.
Travesía Choupana, s/n. Santiago de Compostela.
15706 La Coruña. España.
E-mail: carlospenagil@hotmail.com