Keywords
INTRODUCTION
Atrial septal defect (ASD) is congenital heart disease which is more frequently diagnosed in adults. In some patients, chronic exposure to high pulmonary flow typically causes a progressive increase in pulmonary pressure and resistance, with an estimated prevalence of less than 10%. Patients with severe pulmonary hypertension (PH) or Eisenmenger syndrome have a poor prognosis, but better than the prognosis of patients with idiopathic PH.1 In patients with Eisenmenger syndrome, defect closure may alter their prognosis to one more similar to patients with idiopathic PH. The difference between the 2 entities is thought to be the atrial defect which would function as a safety valve to unload the right ventricle thereby preserving its function and maintaining systemic output, although at the risk of hypoxemia and cyanosis.2
The standard approach to assessing whether PH is reversible or not is acute vasodilator testing with medications, but there is no evidence regarding their usefulness in predicting the response of PH to defect closure. Another simple technique is to temporarily occlude the defect and evaluate pulmonary response during occlusion. Although this technique is well-known, no studies have evaluated its long-term predictive value. Our aim was to assess the usefulness of temporary balloon test occlusion to predict how PH would respond in patients with ASD and severe PH, and its possible value in assessing operability and in determining pulmonary resistance.
METHODS
Technique
Basal levels of pulmonary, systemic, and ventricular end-diastolic pressures were recorded. Pulmonary flow, effective pulmonary flow, and systemic flow were determined based on the Fick principle. The relationship between pulmonary and systemic output (Qp/Qs) was determined, as well as pulmonary vascular resistance (PVR) and systemic vascular resistance (SVR). The ASD was occluded for 15 minutes using a Z-Med II balloon (Numed, Hopkinton, USA) or an Amplatzer balloon (AGA, Minneapolis, USA). The balloon was inflated until the shunt completely disappeared, as shown by transesophageal echocardiography, and then Qp/Qs, PVR, and SVR were again determined. In addition, 2 patients underwent acute vasodilator testing using inhaled nitric oxide (80 ppm) and 1 of them also underwent this test using inhaled iloprost.
We defined a positive response or reversible PH as a mean reduction in pulmonary pressure of ≥25% after balloon test occlusion compared to basal levels, without a fall in systemic pressure or an increase in ventricular end-diastolic pressures. To establish the operability criteria, the result of balloon test occlusion was taken into account, in addition to pulmonary resistance and its relation to systemic resistance.
Patients
Between January 2002 and December 2007, 51 adult patients with ASD were referred to our catheterization laboratory for potential percutaneous closure. In total, 5 of the patients presented severe PH, defined as right ventricular systolic pressure (RVSP) ≥70 mmHg as estimated by transthoracic echocardiography. These patients underwent balloon test occlusion to assess whether PH was reversible. Follow-up was conducted on an outpatient basis and included echocardiography at 1 month, 3 months, and 6 months and annually thereafter.
Statistical Analysis
The SPSS statistical package (version 15) was used. Serial echocardiographic and hemodynamic values were compared using the Wilcoxon nonparametric test.
RESULTS
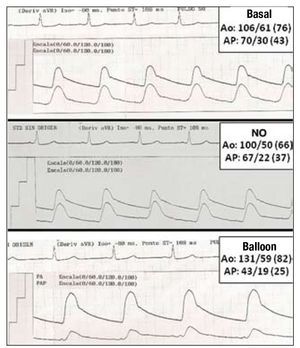
The results of basal echocardiography and echocardiography at follow-up are shown in Table 1. All the patients were symptomatic women with a mean age of 65 (6) years. The mean size of the ASD as estimated by transesophageal echocardiography was 25 (12) mm. The defect was occluded in 4 patients; this was done percutaneously in 3, and 1 underwent surgery due to the lack of suitable margins. Despite receiving treatment with bosentan and sildenafil, pulmonary hypertension remained unchanged at 5-year follow-up in the patient in whom closure was underestimated, although her New York Heart Association (NYHA) functional class changed from III to class II. In the patients in whom ASD closure was successful, the mean RVSP was 85 (17) mmHg before closure, falling to 52 (7) mmHg (P=.06) after a mean 22 (16) months of follow-up. In 2D-mode, a reduction was also observed in the size of the right ventricle from 37 (4) mm to 31 (5) mm (P=.06) and 2D-sonography showed a reduction in the outflow tract from 54 (3) mm to 42 (6) mm (P=.06). Table 2 shows the hemodynamic values obtained during temporary balloon test occlusion. The patient in whom closure was underestimated also underwent tests with vasodilators (inhaled nitric oxide, 80 ppm; inhaled iloprost 10 µL) with negative results (Figure 1). In the patients in whom ASD was successfully closed, mean pulmonary pressure was 38 (5) mmHg, decreasing to 26 (5) mmHg after balloon test occlusion. Systemic pressure did not of pulmonary vascular resistance, its relation to systemic resistance and the size the shunt, balloon test occlusion can provide additional information on whether the pulmonary arterial hypertension is reversible or not in order to establish whether the defect is operable.
Figure 1. Recording of pulmonary and systemic pressure during basal study, after temporary balloon test occlusion, and after nitric oxide (NO) inhalation in patient 3. The results of temporary balloon test occlusion were negative.
Formerly, in order to establish whether adult patients with severe PH and dominant left-right shunt were operable, pulmonary biopsy was conducted to determine whether the histological changes associated with PH in small pulmonary vessels were irreversible or reversible, mainly by vasoconstriction. Currently, different vasodilator agents, such as tolazoline, epoprostenol, nitric oxide, iloprost, or sildenafil, are used to assess the degree of reversibility. However, there is no evidence regarding their usefulness in predicting the response of PH to defect closure.
Two studies have demonstrated long-term reductions in pulmonary pressure in patients with ASD and PH who have undergone percutaneous closure. In a study by Suárez de Lezo et al,3 mean systolic pulmonary pressure was invasively measured in 29 patients. The initial value of 65 (23) mmHg decreased to 54 (21) mmHg after occlusion during approximately 21 months of follow-up. More recently, Balint et al4 studied 44 patients; after a mean follow-up of 31 months, pulmonary pressure fell from 58 mmHg to 44 mmHg.
Temporary balloon test occlusion offers a unique and unrivalled opportunity to assess the response of PH following definitive closure.
If there are elevated ventricular end-diastolic pressures or decreased systemic expenditure, defect closure could be detrimental to the right ventricle as this would close the safety valve that helps maintain its contractile function. The degree to which there is a reduction in pulmonary pressure during closure provides information on the percentage of hyperkinetic hypertension. In addition to the acute reduction due to the increase in pulmonary flow, there is a subsequent reduction in pulmonary pressure in the long term. This small long-term reduction may be due to reversible changes in pulmonary arteriolar vasculature. It is reasonable to assume that temporary balloon test occlusion may reveal the short-term changes in PH by reducing the pulmonary hyperflow and that acute vasodilator testing may show the long-term changes in vascular remodelling. A mean ≥25% decrease in pulmonary pressure relative to basal values is required to define the test as positive. However, this value is arbitrary, and larger studies are needed to define objective criteria by which the test can be considered positive and to assess its relationship to the long-term evolution of pulmonary pressure. vary significantly after balloon test occlusion, as indicated by the change from 85 (9) mmHg to 89 (9) mmHg (P=1).
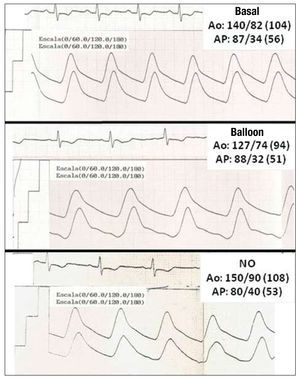
Basal PVR was 4.5 uW/m2 falling to 4.1 uW/ m2 (P=1) after temporary balloon test occlusion. After balloon test occlusion, Qp/Qs changed from 2.4:1 to 1.1:1 (P=.06). No increase was found in right ventricular or left ventricular end-diastolic pressures. The hemodynamic values of patient 1 are shown in Figure 2. There was a mean 30% reduction in mean pulmonary pressure after balloon test occlusion, and a mean 40% reduction in systolic pulmonary pressure over the long term. The symptoms improved in all patients after occlusion. The patients were in NYHA functional class III before occlusion, whereas after occlusion 3 patients were in class II and 1 patient was in class I. All the patients were in sinus rhythm both before and after closure.
Figure 2. Recording of pulmonary and systemic pressure during basal study, after nitric oxide (NO) inhalation, and after temporary balloon test occlusion in patient 1. The results of temporary balloon test occlusion were positive.
DISCUSSION
A hemodynamic study during temporary balloon test occlusion in elderly patients with severe PH can be a good indicator of the subsequent evolution of PH. In addition to the absolute value
Correspondence: Dr. A. Sánchez-Recalde.
Unidad de Hemodinámica y Cardiología Intervencionista. Hospital General Universitario La Paz.
P.o de la Castellana, 261; Planta 1.a diagonal. 28046 Madrid. Spain.
E-mail: recalde@secardiologia.es
Received February 25, 2009.
Accepted for publication August 8, 2009.