We report the results of a survival analysis performed to evaluate the relationship of preimplantation biventricular volumes and function, assessed by cardiac magnetic resonance (CMR), with clinical response to cardiac resynchronization therapy (CRT) and long-term mortality.
Right ventricular volumes and function are well established markers of prognosis in heart failure, and therefore we hypothesized that they would also be associated with lack of response and higher mortality in the CRT setting.
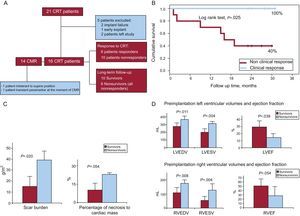
Twenty-one CRT candidates were enrolled between November 2007 and November 2008, as part of a study performed to determine the levels of different serum biomarkers in heart failure patients and to assess their association with response to CRT and long-term mortality. Patients underwent preimplantation CMR as a part of the protocol of the study. Figure A depicts the flow chart for the 21 CRT patients along the follow-up period and the number of responders and nonresponders according to definition.
A: Flow chart for the 21 cardiac resynchronization therapy patients, during the follow-up period. B: Kaplan Meier survival curves for responders and nonresponders to cardiac resynchronization therapy. C: Preimplantation scar burden and percentage of necrosis to cardiac mass assessed by cardiac magnetic resonance according to survival status. D: Preimplantation left and right ventricular volumes and ejection fraction assessed by cardiac magnetic resonance according to survival status.
LVEDV: 369 (42) vs 276 (47) mL; LVESV: 311 (32) vs 198 (51) mL; LVEF: 15 (5) vs 29 (9) %, (nonsurvivors vs survivors); RVEDV: 177 (21) vs 111 (33) mL; RVESV: 128 (43) vs 56 (26) mL; RVEF: 28 (20) vs 51 (15) %, (nonsurvivors vs survivors).
CMR, cardiac magnetic resonance; CRT, cardiac resynchronization therapy; LVEDV, left ventricle end-diastolic volume; LVEF, left ventricle ejection fraction; LVESV, left ventricle end-systolic volume; RVEDV, right ventricle end-diastolic volume; RVEF, right ventricle ejection fraction; RVESV, right ventricle end-systolic volume.
Response to CRT was defined as an improvement of ≥10% in a 6-min walking test, conducted 6 months after CRT implantation, and the absence of events (admissions for heart failure, cardiac death, or heart transplantation) during the first 6 months after implantation.
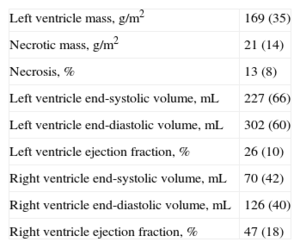
Patients were followed up for a median of 23.5 [16-27] months. Six patients (33.3%) died during the follow-up period: the time elapsed until the event occurrence was 387 [90-515] days, and 496 [387-549] days if expressed conditioned to the first six months, in order to exclude the patient who died early, during the time of assessment of response to CRT. Survival rates were significantly different among responders and nonresponders (Fig. B). The Table shows the mean (standard deviation) values for the main variables assessed at the preimplantation CMR.
Main Variables Assessed During Preimplantation Cardiac Magnetic Resonance
| Left ventricle mass, g/m2 | 169 (35) |
| Necrotic mass, g/m2 | 21 (14) |
| Necrosis, % | 13 (8) |
| Left ventricle end-systolic volume, mL | 227 (66) |
| Left ventricle end-diastolic volume, mL | 302 (60) |
| Left ventricle ejection fraction, % | 26 (10) |
| Right ventricle end-systolic volume, mL | 70 (42) |
| Right ventricle end-diastolic volume, mL | 126 (40) |
| Right ventricle ejection fraction, % | 47 (18) |
Data are expressed as mean (standard deviation).
Patients who died showed larger preimplantation left ventricular end-diastolic volume and left ventricular end-systolic volume in addition to lower left ventricular ejection fraction when compared with the survivors. They also had larger preimplantation right ventricular end-diastolic volume and right ventricular end-systolic volume, in addition to lower right ventricular ejection fraction when compared with the survivors. Nonsurvivors also had a greater scar burden and a greater percentage of necrosis to cardiac mass than the survivors (data depicted in Figs. C and D). These findings are in line with previous reports.1 We did not find significant associations among scar location, response to CRT, or mortality, but this can be explained by the very small number of patients in our cohort.
Nonsurvivors in our group also showed larger right ventricular end-diastolic volume and right ventricular end-systolic volume, in addition to lower right ventricular ejection fraction, when compared with the survivors. This is congruent with the fact that right ventricular volumes and dysfunction are well established markers of prognosis in heart failure,2 but little has been studied about right ventricular volumes and ejection fraction in terms of their relationship with response to CRT and long-term survival. Some authors have studied the relationship between right ventricular dysfunction and left ventricle dyssinchrony,3 but publications about right ventricular volumes and function, and their association with response to CRT and long-term mortality are very scarce.4 Recently, Alpendurada et al.5 found that baseline right ventricular dysfunction, assessed by CMR, predicted lack of response to CRT and a bad long-term outcome in a group of 60 patients, with a median follow-up time of 26 months. As in our cohort, they also found that the rate of response to CRT was low (48%). Tabereaux et al.6 also found a high rate of nonresponders (of almost 60%) among patients with preimplantation right ventricular failure. Our findings, although in a smaller group of patients, are consistent with these observations. Hence, our hypothesis about the association of right ventricular volumes and dysfunction with the lack of response and mortality, in the setting of CRT, might be true. It is possible that large right ventricular volumes and dysfunction reflect an advanced stage of disease, characterized by an extended remodeling, and that these aspects preclude response to CRT. Although conventional criteria for selection of patients for CRT only take into account the left ventricle parameters, considering the right ventricle structure and function before implantation, could identify a subgroup of more severely ill patients that might not benefit from CRT at all.
In the light of our findings, we believe that the role of preimplantation right ventricular volume and function should be further explored in the setting of CRT, with regard to both–response to CRT and long-term mortality. In addition, it is advisable to study these aspects in larger populations so that we can better define the need of preimplantation evaluation of the right ventricle in CRT candidates.
Lastly, although CMR is not widely available, and patients with CRT find it difficult to undergo a new CMR in the post-implantation phase, it is possible that in the near future, greater availability of CMR-safe and magnetic resonance imaging-safe devices, would allow patients to undergo a comparative CMR after the CRT implantation. This would help us to understand more about the right ventricle structure and function in the CRT setting.
FundingThis study was funded by a Cardiology grant from Fundación Carolina-BBVA obtained by Dr M. E. Tettamanti.