We assessed short- and long-term outcomes of primary angioplasty in ST-segment elevation myocardial infarction by comparing bifurcation culprit lesions (BCL) with non-BCL.
MethodsObservational study with a propensity score matched control group. Among 2746 consecutive ST-segment elevation myocardial infarction patients, we found 274 (10%) patients with BCL. The primary outcome was a composite endpoint including all-cause death, myocardial infarction, coronary artery bypass grafting or target vessel revascularization, assessed at 30-days and 5-years.
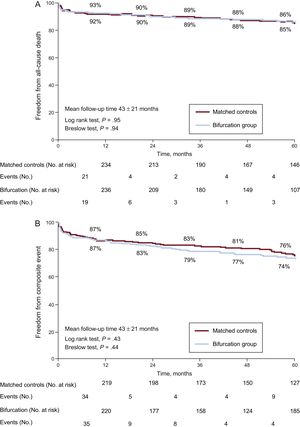
ResultsBaseline characteristics showed no differences after propensity matching (1:1). In the BCL group, the most frequent strategy was provisional stenting of the main branch (84%). Compared with the non-BCL group, the procedures were technically more complex in the BCL group in terms of need for balloon dilatation (71% BCL vs 59% non-BCL; P = .003), longer procedural time (70 ± 29minutes BCL vs 62.8 ± 28.9minutes non-BCL; P = .004) and contrast use (256.2 ± 87.9mL BCL vs 221.1 ± 82.3mL non-BCL; P < .001). Main branch angiographic success was similar (93.4% BCL vs 93.8% non-BCL; P = .86). Thirty-day all-cause mortality was similar between groups: 4.7% BCL vs 5.1% non-BCL; P = .84. At the 5-year follow-up, there were no differences in all-cause death (12% BCL vs 13% non-BCL; P = .95) or the combined event (22% BCL vs 21% non-BCL; P = .43).
ConclusionsPrimary angioplasty of a BCL was technically more complex; however, main branch angiographic success was similar, and there were no differences in long-term prognosis compared with non-BCL patients.
Keywords
Bifurcations are considered challenging lesions for percutaneous coronary intervention (PCI), and despite substantial improvements, bifurcation (BIF) PCI is associated with worse immediate results and clinical outcomes, mainly because of a higher revascularization rate.1,2 In the last years, the growing body of BIF research has allowed a consensus regarding a simpler approach using 1 stent in the main vessel (provisional stenting) instead of 2-stent techniques or dedicated devices for most cases.3 This approach simplifies the procedure but carries a greater risk of side branch (SB) closure that apparently is not associated with worse clinical outcomes.4–6
In acute ST-segment elevation myocardial infarction (STEMI), timely primary PCI is currently the standard treatment for most patients.7 During a primary PCI, the operator must deal in an emergent situation with ad hoc intervention over thrombotic lesions in often unstable patients. Therefore, finding a BIF as the culprit lesion adds further complexity to primary PCI, which could potentially lead to worse short- and long-term outcomes. The purpose of this study was to evaluate the incidence of bifurcation culprit lesions (BCL) in acute STEMI, and to compare procedural characteristics and clinical outcomes between BCL STEMI patients and a matched control (MC) group of non-BCL STEMI patients.
METHODSWe designed an observational, analytical, retrospective cohort study, using propensity score matching to pair patients with and without a BCL in STEMI.
Patient SelectionData from all cardiac catheterizations and hospital admissions were prospectively filled in a comprehensive database shared by a network of hospitals that includes 1 main tertiary center and 2 satellite centers. For the purpose of this study, we retrospectively selected from the database patients with STEMI treated with primary or rescue PCI < 24hours from symptom onset. Exclusion criteria were: normal coronary arteries or alternative diagnostics different from STEMI; other emergent indications for PCI different from STEMI (cardiac arrest or shock without suspected STEMI); culprit lesion located at left main or surgical grafts and facilitated PCI. From 2004 to 2015, a total of 2746 STEMI patients met the inclusion/exclusion criteria.
Lesion SelectionAll cases with the culprit lesion coded as bifurcated in our database had their angiographies independently reviewed by 2 interventional cardiologists who were not involved in the analysis of the outcomes. The selection of BIF cases and controls is detailed in and . The BIF group included 274 patients (10%) with lesions involving or adjacent (≤ 5mm) to a SB ≥ 2mm by visual estimation or quantitative coronary angiography if there was disagreement.
Propensity Score Matching for Comparison GroupPropensity score matching was used to create an MC group for comparison and reduce differences in clinical characteristics.8 The propensity score was estimated using logistic regression, entering only baseline (pre-PCI) covariates by statistical (differences with P value < .1) and clinical criteria. The model was adjusted by date of the primary PCI, time from symptoms onset to PCI, culprit vessel, age, sex, rescue PCI, number of diseased vessels, previous myocardial infarction (MI), and diabetes. There were no interactions among variables, and the area under the curve was 0.66. Participants were matched using 1:1 nearest neighbor matching. A total of 274 patients from the BIF group were matched with 274 patients from the control group, from which 2189 were unmatched. The achieved balance was assessed with a Hotelling's T-square statistic (T^2, 0.56, df, 12,535; P = .876).9
Variables and Clinical Outcomes DefinitionsThe main outcome of this study was all-cause mortality and a combined endpoint (including all-cause death, recurrent MI, coronary artery bypass graft or target vessel revascularization) at 5 years.
Main branch (MB) angiographic success was defined as patent artery (Thrombolysis In Myocardial Infarction [TIMI] flow 2 or 3) with residual stenosis ≤ 30% (visual estimation). Side branch angiographic success was defined as TIMI flow 2 or 3. BCL global angiographic success was defined as MB and SB angiographic success. Death was analyzed as all-cause death. Medina BIF classification was evaluated when TIMI flow10 2 or 3 was obtained, and defined as previously described.11 Recurrent MI (nonfatal) was considered as type 1 or 2 using the third universal definition.12 Target vessel revascularization and target lesion revascularization (TLR) was defined as any revascularization within the culprit vessel or the culprit lesion (or 5mm edge), respectively.
Data from the index cardiac catheterization, hospital admission, and 30-day follow-up was routinely and prospectively collected in all patients. Follow-up data were obtained (mainly from electronic clinical records, and telephone interview in patients with external clinical follow-up) for the BIF and MC cohort (n = 548) and updated until January 2016, then censored to a maximum of 5 years of follow-up. Censoring was done due to a wide inclusion timeframe (January 2004 to January 2015) and in order to ensure greater consistency in the follow-up data (≥ 1 year and up to 5 years). The mean follow-up was 42.9 ± 21.4 months.
Procedural CharacteristicsAll patients were premedicated with aspirin and tyenopiridine or ticagrelor with loading dose; no upstream glycoprotein IIb/IIIa inhibitors were used. Other treatments, the interventional technique and the BIF approach were decided by the operator. Secondary prevention drugs following current European guidelines and 12 months of dual antiplatelet therapy were recommended at discharge.7
Statistical AnalysisContinuous variables are expressed as mean values ± standard deviation and were compared by the Student t test if normally distributed. In the case of skewed distribution, we used median values with interquartile ranges and the data were compared by Wilcoxon Mann-Whitney test. Categorical variables are expressed as numbers and percentages and were compared using the chi-square or Fisher exact test, as deemed appropriate. Thirty-day events were compared with Cox regression analysis, providing survival probabilities and hazard ratios (HR) for comparison. Five-year all-cause mortality and the combined endpoint were compared with Cox regression analysis. Kaplan-Meier curves were built and then compared using the Breslow and log-rank tests. To adjust for the effect of concomitant all-cause mortality, the Fine and Gray competing risk proportional hazard regression was used to report the HRs for each component of the combined endpoint.13 Crude HRs were adjusted by drug-eluting (vs bare metal) stent, aspiration thrombectomy, and use of IIb/IIIa inhibitors. P values below .05 were considered statistically significant. Propensity computations were performed with MatchIt package of R software (version 3.0.2), all other analyses with SPSS (version 21).
RESULTSBaseline CharacteristicsA total of 274 (10%) lesions were included in the BIF group, while all other lesions (2472) were considered non-BIF lesions (control group). Baseline clinical characteristics from the total population, BIF, control and MC groups are shown in Table 1. There were no significant differences in either cardiac risk factors or the extension of coronary disease between the BIF and control groups. The main difference before propensity matching was the infarct-related artery: in the BIF group, the left anterior descending artery was more frequently involved, and less frequently the right coronary artery (Figure 1A). Segments involved (Figure 1B) were also similar within left anterior descending artery or left circumflex infarcts (mainly proximal and midsegments). In contrast, in the right coronary artery the culprit lesion was found mainly in distal segments followed by midsegments in the BIF group, whereas it was found more frequently in proximal or midsegments in the control group. After propensity score matching, the infarct-related artery was well balanced between BIF and MC groups.
Clinical and Anatomic Characteristics, Before and After Propensity Matching
| Variable | Before matching | After matching | |||||
|---|---|---|---|---|---|---|---|
| Total (n = 2746) | BIF group (n = 274) | Controls (n = 2472) | P | BIF group (n = 274) | MC group (n = 274) | P | |
| Agea | 63 ± 13 | 62 ± 14 | 63 ± 13 | .83 | 62 ± 14 | 63 ± 13 | .75 |
| Femalea | 594 (22) | 57 (21) | 537 (22) | .76 | 57 (21) | 57 (21) | 1 |
| BMI, kg/cm2 | 28 ± 5 | 28 ± 4 | 28 ± 5 | .64 | 28 ± 4 | 27 ± 4 | .72 |
| Cardiovascular risk factors | |||||||
| Obesity | 653 (24) | 69 (25) | 584 (24) | .58 | 69 (25) | 67 (25) | .84 |
| Hypertension | 1414 (52) | 135 (49) | 1279 (52) | .44 | 135 (49) | 141 (51) | .61 |
| Dyslipidemia | 1166 (43) | 114 (42) | 1052 (43) | .76 | 114 (42) | 116 (42) | .86 |
| Diabetesa | 572 (21) | 50 (18) | 522 (21) | .31 | 50 (18) | 49 (18) | .91 |
| Smoking history | 1713 (64) | 176 (64) | 1537 (62) | .51 | 176 (64) | 166 (60) | .29 |
| Familial CAD history | 120 (4) | 11 (4) | 109 (4) | .75 | 11 (4) | 11 (4) | 1 |
| Previous history | |||||||
| Previous stroke | 100 (4) | 8 (3) | 92 (4) | .50 | 8 (3) | 8 (3) | 1 |
| Peripheral vascular disease | 115 (4) | 7 (3) | 108 (4) | .16 | 7 (3) | 6 (2) | .78 |
| Chronic kidney disease | 103 (4) | 8 (3) | 95 (4) | .45 | 8 (3) | 7 (3) | .79 |
| Previous MIa | 248 (9) | 18 (7) | 230 (9) | .13 | 18 (7) | 13 (5) | .36 |
| Previous PCI | 230 (8) | 20 (7) | 210 (8) | .50 | 20 (7) | 12 (4) | .15 |
| Previous CABG | 16 (0.6) | 1 (0.4) | 15 (0.6) | .62 | 1 (0.4) | 1 (0.4) | 1 |
| Coronary anatomy | |||||||
| Number of diseased vesselsa | .68 | .70 | |||||
| 0b | 80 (3) | 8 (3) | 72 (3) | 8 (3) | 7 (3) | ||
| 1 | 1472 (54) | 147 (54) | 1325 (54) | 147 (54) | 157 (57) | ||
| 2 | 803 (29) | 86 (31) | 717 (29) | 86 (31) | 74 (27) | ||
| 3 | 391 (14) | 33 (12) | 358 (15) | 33 (12) | 36 (13) | ||
| Mean number of severely diseased vessels | 1.35 ± 0.7 | 1.33 ± 0.7 | 1.35 ± 0.7 | .67 | 1.33 ± 0.7 | 1.29 ± 0.6 | .48 |
| Dominance | .21 | .72 | |||||
| Left | 188 (7) | 20 (7) | 168 (7) | 20 (7) | 18 (7) | ||
| Right | 2323 (85) | 223 (81) | 2100 (85) | 223 (81) | 219 (80) | ||
| Balanced | 235 (31) | 31 (11) | 204 (8) | 31 (11) | 37 (14) | ||
| Culprit vessela | < .001 | .59 | |||||
| LAD | 1096 (40) | 159 (58) | 937 (38) | 159 (58) | 147 (54) | ||
| LCx | 324 (12) | 39 (14) | 285 (12) | 39 (14) | 53 (19) | ||
| RCA | 1107 (40) | 50 (18) | 1057 (43) | 50 (18) | 49 (18) | ||
| Other | 219 (8) | 26 (9) | 193 (8) | 26 (9) | 25 (9) | ||
BIF, bifurcation; BMI, body mass index; CABG, coronary artery bypass graft; CAD, coronary artery disease; LAD, left anterior descending artery; LCx, left circumflex; MC, matched control; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCA, right coronary artery.
Data are expressed as mean ± standard deviation or No. (%).
A: distribution of infarct-related artery between BIF (n = 274) and control (n = 2472) groups (P < .001). B: segment where the culprit lesion was found within each infarct-related artery. BIF, bifurcation; LAD, left anterior descending artery; LCx, left circumflex; RCA, right coronary artery.
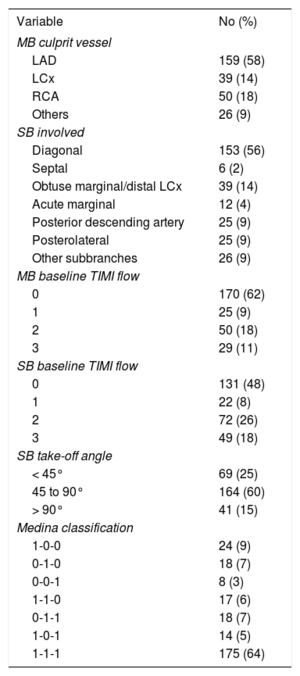
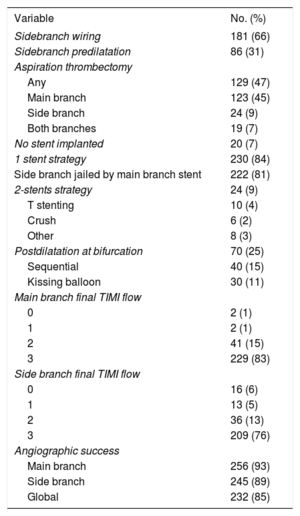
Further anatomical data of the BIF group are shown in Table 2. The mean diameter of the SB was 2.16 ± 0.2mm. More than half of the BIF (56%) were left anterior descending artery-diagonal (involving the first diagonal branch in 124 [45%] cases). The most frequent type of Medina classification was largely the 1.1.1 (64%), with the other types were more or less evenly distributed. The type of lesion known as “true bifurcation” (1.1.1, 1.0.1, 0.1.1) was found in 207 (76%) patients.
Coronary Anatomy and Angiographic Characteristics of the Bifurcation Group (n = 274)
| Variable | No (%) |
|---|---|
| MB culprit vessel | |
| LAD | 159 (58) |
| LCx | 39 (14) |
| RCA | 50 (18) |
| Others | 26 (9) |
| SB involved | |
| Diagonal | 153 (56) |
| Septal | 6 (2) |
| Obtuse marginal/distal LCx | 39 (14) |
| Acute marginal | 12 (4) |
| Posterior descending artery | 25 (9) |
| Posterolateral | 25 (9) |
| Other subbranches | 26 (9) |
| MB baseline TIMI flow | |
| 0 | 170 (62) |
| 1 | 25 (9) |
| 2 | 50 (18) |
| 3 | 29 (11) |
| SB baseline TIMI flow | |
| 0 | 131 (48) |
| 1 | 22 (8) |
| 2 | 72 (26) |
| 3 | 49 (18) |
| SB take-off angle | |
| < 45° | 69 (25) |
| 45 to 90° | 164 (60) |
| > 90° | 41 (15) |
| Medina classification | |
| 1-0-0 | 24 (9) |
| 0-1-0 | 18 (7) |
| 0-0-1 | 8 (3) |
| 1-1-0 | 17 (6) |
| 0-1-1 | 18 (7) |
| 1-0-1 | 14 (5) |
| 1-1-1 | 175 (64) |
LAD, left anterior descending artery; LCx, left circumflex; MB, main branch; RCA, right coronary artery; SB, side branch; TIMI, thrombolysis in myocardial infarction.
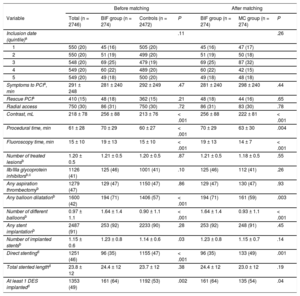
Comparative procedural and interventional data are shown in Table 3. Time from symptoms onset to PCI, a relevant prognostic factor in STEMI, was included in the propensity score and was similar in all groups. While it might be rather long (mean 281 and 298minutes), it represents “real life” and decreased significantly over time (from a mean of 312 ± 275minutes in the oldest quintile to 214 ± 169minutes in the most recent (P = .003 for comparison among quintiles). The mean time from symptom onset to PCI was higher in the rescue PCI subgroup compared with the primary PCI subgroup (415 ± 243 vs 269 ± 230; P < .001); further differential procedural details between primary and rescue PCI are shown in and . The quintiles of procedural inclusion date (20% each 2 years), as well as the rate of rescue PCI (17.5% and 16.1%), were evenly distributed. After propensity score matching, the procedures in the BIF group were longer (70 ± 29 BIF vs 63 ± 30minutes MC; P = .004), and required more fluoroscopy time (19 ± 13minutes BIF vs 14 ± 7minute MC; P < .001) and more contrast (256 ± 88mL BIF vs 222 ± 81mL MC; P < .001) compared with the MC group. The number of treated lesions were similar, but the procedures of the BIF group were technically more complex in terms of need for any balloon dilatation (71% BIF vs 59% MC; P = .003) and the number of different balloons used (1.64 ± 1.4 BIF vs 0.93 ± 1.1 MC; P < .001). After propensity score matching, the number of implanted stents per patient was similar between groups (1.23 ± 0.8 BIF vs 1.15 ± 0.7 MC; P = .14), but drug-eluting stents were more frequently implanted in the BIF group (64% BIF vs 54% MC; P = .04) and direct implantation was less frequently used (35% BIF vs 49% MC; P = .001).
Procedural Characteristics Before and After Propensity-matched Analysis
| Before matching | After matching | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Total (n = 2746) | BIF group (n = 274) | Controls (n = 2472) | P | BIF group (n = 274) | MC group (n = 274) | P |
| Inclusion date (quintile)a | .11 | .26 | |||||
| 1 | 550 (20) | 45 (16) | 505 (20) | 45 (16) | 47 (17) | ||
| 2 | 550 (20) | 51 (19) | 499 (20) | 51 (19) | 50 (18) | ||
| 3 | 548 (20) | 69 (25) | 479 (19) | 69 (25) | 87 (32) | ||
| 4 | 549 (20) | 60 (22) | 489 (20) | 60 (22) | 42 (15) | ||
| 5 | 549 (20) | 49 (18) | 500 (20) | 49 (18) | 48 (18) | ||
| Symptoms to PCIa, min | 291 ± 248 | 281 ± 240 | 292 ± 249 | .47 | 281 ± 240 | 298 ± 240 | .44 |
| Rescue PCIa | 410 (15) | 48 (18) | 362 (15) | .21 | 48 (18) | 44 (16) | .65 |
| Radial access | 750 (30) | 86 (31) | 750 (30) | .72 | 86 (31) | 83 (30) | .78 |
| Contrast, mL | 218 ± 78 | 256 ± 88 | 213 ± 76 | < .001 | 256 ± 88 | 222 ± 81 | < .001 |
| Procedural time, min | 61 ± 28 | 70 ± 29 | 60 ± 27 | < .001 | 70 ± 29 | 63 ± 30 | .004 |
| Fluoroscopy time, min | 15 ± 10 | 19 ± 13 | 15 ± 10 | < .001 | 19 ± 13 | 14 ± 7 | < .001 |
| Number of treated lesionsb | 1.20 ± 0.5 | 1.21 ± 0.5 | 1.20 ± 0.5 | .87 | 1.21 ± 0.5 | 1.18 ± 0.5 | .55 |
| IIb/IIIa glycoprotein inhibitorsb,c | 1126 (41) | 125 (46) | 1001 (41) | .10 | 125 (46) | 112 (41) | .26 |
| Any aspiration thrombectomyb | 1279 (47) | 129 (47) | 1150 (47) | .86 | 129 (47) | 130 (47) | .93 |
| Any balloon dilatationb | 1600 (42) | 194 (71) | 1406 (57) | < .001 | 194 (71) | 161 (59) | .003 |
| Number of different balloonsb | 0.97 ± 1.1 | 1.64 ± 1.4 | 0.90 ± 1.1 | < .001 | 1.64 ± 1.4 | 0.93 ± 1.1 | < .001 |
| Any stent implantationb | 2487 (91) | 253 (92) | 2233 (90) | .28 | 253 (92) | 248 (91) | .45 |
| Number of implanted stentsb | 1.15 ± 0.6 | 1.23 ± 0.8 | 1.14 ± 0.6 | .03 | 1.23 ± 0.8 | 1.15 ± 0.7 | .14 |
| Direct stentingd | 1251 (46) | 96 (35) | 1155 (47) | < .001 | 96 (35) | 133 (49) | .001 |
| Total stented lengthd | 23.8 ± 12 | 24.4 ± 12 | 23.7 ± 12 | .38 | 24.4 ± 12 | 23.0 ± 12 | .19 |
| At least 1 DES implantedd | 1353 (49) | 161 (64) | 1192 (53) | .002 | 161 (64) | 135 (54) | .04 |
BIF, bifurcation; DES, drug-eluting stent; MC, matched control; PCI, percutaneous coronary intervention.
Data are expressed as mean ± standard deviation or No. (%).
Specific details of the PCI in the BIF group are depicted in Table 4. In two-thirds of the lesions, the SB was wired, and the preferred approach was a single, provisional stenting over the MB (84%). The SB was jailed in 81% but was patent in most cases at the end of the procedure (only 11% of TIMI flow 0 or 1). Main branch angiographic success was similar (93.4% BIF vs 93.8% MC; P = .86), although the global angiographic success was lower in the BIF group (84.7%).
Procedural Characteristics of Bifurcation Culprit Lesion
| Variable | No. (%) |
|---|---|
| Sidebranch wiring | 181 (66) |
| Sidebranch predilatation | 86 (31) |
| Aspiration thrombectomy | |
| Any | 129 (47) |
| Main branch | 123 (45) |
| Side branch | 24 (9) |
| Both branches | 19 (7) |
| No stent implanted | 20 (7) |
| 1 stent strategy | 230 (84) |
| Side branch jailed by main branch stent | 222 (81) |
| 2-stents strategy | 24 (9) |
| T stenting | 10 (4) |
| Crush | 6 (2) |
| Other | 8 (3) |
| Postdilatation at bifurcation | 70 (25) |
| Sequential | 40 (15) |
| Kissing balloon | 30 (11) |
| Main branch final TIMI flow | |
| 0 | 2 (1) |
| 1 | 2 (1) |
| 2 | 41 (15) |
| 3 | 229 (83) |
| Side branch final TIMI flow | |
| 0 | 16 (6) |
| 1 | 13 (5) |
| 2 | 36 (13) |
| 3 | 209 (76) |
| Angiographic success | |
| Main branch | 256 (93) |
| Side branch | 245 (89) |
| Global | 232 (85) |
TIMI, Thrombolysis In Myocardial Infarction.
In the paired population (n = 574), in-hospital all-cause mortality and cardiac mortality were similar: 3.3% BIF vs 2.6% MC; P = .61 and 2.6% BIF vs 2.2% MC; P = .76, respectively. Thirty-day clinical events were similar with no differences in survival free from all-cause death (95.3% BIF vs 94.9% MC; P = .84; HR, 0.93; 95% confidence interval [95%CI], 0.44-1.97), survival free from cardiac mortality (96% BIF vs 95.6% MC; P = .83; HR, 0.91; 95%CI, 0.40-2.07) or survival free from recurrent MI (98.5% BIF vs 98.9% MC; P = .71, HR, 1.33; 95%CI, 0.30-5.95). Four patients underwent coronary artery bypass graft in the BIF group compared with 2 patients in MC group, but without statistical significance (survival free from coronary artery bypass grafting 98.5% BIF vs 99.3% MC; P = .42, HR, 2.01; 95%CI, 0.37-10.99).
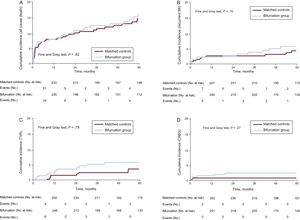
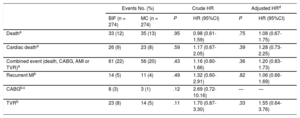
At long-term follow-up, there were no differences in all-cause death or the composite endpoint (Figure 2 and ; Table 5 and ). The individual components of the combined event were evenly distributed, with slightly higher numbers for target vessel revascularization and coronary artery bypass grafting in the BIF group (Table 5 and Figure 3). Target lesion revascularization occurred in 17 (6%) patients in the BIF group compared with 12 (4%) in the MC group; crude HR, 1.44; 95%CI, 0.69-3.02; P = .33 and adjusted HR, 1.47; 95%CI, 0.70-3.09; P = .31. There were 3 cases of definite stent thrombosis in each group, all of them were subacute in the BIF group, whereas 2 cases of thrombosis were subacute and the other one very late (17 months) in the MC group.
Events and Hazard Ratios at 5-year of Follow-up
| Events No. (%) | Crude HR | Adjusted HRd | ||||
|---|---|---|---|---|---|---|
| BIF (n = 274) | MC (n = 274) | P | HR (95%CI) | P | HR (95%CI) | |
| Deatha | 33 (12) | 35 (13) | .95 | 0.98 (0.61-1.59) | .75 | 1.08 (0.67-1.75) |
| Cardiac deatha | 26 (9) | 23 (8) | .59 | 1.17 (0.67-2.05) | .39 | 1.28 (0.73-2.25) |
| Combined event (death, CABG, AMI or TVR)a | 61 (22) | 56 (20) | .43 | 1.16 (0.80-1.66) | .36 | 1.20 (0.83-1.73) |
| Recurrent MIb | 14 (5) | 11 (4) | .49 | 1.32 (0.60-2.91) | .82 | 1.06 (0.66-1.69) |
| CABGb,c | 8 (3) | 3 (1) | .12 | 2.69 (0.72-10.16) | — | — |
| TVRb | 23 (8) | 14 (5) | .11 | 1.70 (0.87-3.30) | .33 | 1.55 (0.64-3.76) |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; BIF, bifurcation; CABG, coronary artery bypass graft; HR, hazard ratio; MC, matched control; MI, myocardial infarction; TVR, target vessel revascularization.
We present the second largest series of BCL in STEMI, the first with a propensity score matching control group and the longest follow-up. The main finding of the present study was the similar short- and long-term prognosis in patients with and without BCL in STEMI.
Angiographic FindingsIn our study, the culprit lesion involved a BIF in 10% of STEMI. In the literature, this frequency ranges from 15% to 20% of all PCIs,3 and in a few specific studies of BCL in STEMI between 10% and 23%.14–17 Although there is no single anatomical feature that defines a SB as “significant” to consider the lesion as a BIF,3 we used the 2-mm cutoff because it is common practice and was used in previous BIF studies.18 Frangos et al.16 and Kanei et al.17 also selected patients with SB ≥ 2 and 2.25mm, respectively, and found BCL rates of 10% and 14%.
The main difference between STEMI patients with and without a BCL was the infarct-related artery, with a predominance (56%) of left anterior descending artery-diagonal lesions within the BIF group and a majority (43%) of right coronary artery infarctions in non-BCL patients. This pattern was also found by Dudek et al.15 and a probable explanation is that the proximal right coronary artery lacks significant branches, as shown in Figure 1B. Except for this peculiarity, the most frequently affected segments were proximal followed by middle, as previously reported.19
The classification of the BIF anatomy by Medina and all other classifications are troublesome in the setting of a STEMI because the angiographic appearance of the plaque or thrombus might be similar. Moreover, 62% of the MB and 48% of the SB had TIMI flow 0 at the baseline angiogram, and therefore we decided to assess the Medina classification when at least temporary TIMI flow 2 or 3 was obtained (after wire crossing and/or aspiration thrombectomy). Although the anatomy should be interpreted with caution, most BIF had a complex anatomy (64% 1.1.1; 76% “true bifurcation”). In contrast, previous authors classified the BIF before opening the infarct-related artery in STEMI but found discordant data.14,16 In the stable setting, data from the large COBIS Registry II (non-left main BIF data) showed aggregate rates of 34% for 1.1.1 lesions and 56% for “true bifurcations”.20 Therefore, we might conclude that BCL in STEMI are at least as anatomically complex as in the stable setting.
Primary Percutaneous Coronary Intervention and Short-term ResultsThe PCI procedure in the BIF group was indeed longer (in terms of time, amount of contrast and radiation) and was also technically more complex. More patients in the BIF group underwent at least 1 balloon dilatation and predilatation before stenting. Conversely, there was no increase in the rate of aspiration thrombectomy or in the number of implanted stents. Many aspiration thrombectomy devices do not cross over a regular 6-Fr catheter if more than 1 wire has been inserted, which may explain the low rate of aspiration to both MB and SB (7%). The similar number of stents per patient is probably a result of the predominant single-stent approach, encouraged by the emergent setting. Moreover, the burden of coronary disease in the patients with a BCL was also similar to that in the control group (similar number of diseased vessels, number of treated lesions, or total stented length).
The single-stent strategy chosen in 84% of the BCL patients (91% of patients who had at least 1 stent implanted) was consistent with that of many randomized studies showing similar or better outcomes with 1- vs 2-stent techniques (although most of them excluded STEMI patients).4–6 Only the DKCRUSH II study included STEMI patients (n = 63) and found similar in-hospital or 1-year events comparing the provisional stenting and the double kissing double crush 2-stent technique.21 On the other hand, higher rates of early and late stent thrombosis have been reported for STEMI patients,22 and therefore provisional stenting seems reasonable in the emergent primary PCI setting.
Regarding the angiographic results, final TIMI flow was worse in the SB than in the MB, and global angiographic success was lacking in 15% of the BIF group. Nevertheless, MB angiographic success was similar in the BIF and MC groups, leading to similar clinical outcomes. These similar outcomes might be explained by the adjustment for other prognostic factors (time to reperfusion23 or similar distribution of the infarct-related artery24) or the relatively low (15%) rate of “lost SBs”. On the other hand, the SB occlusion might be only temporary (spasm or thrombus that will resolve), and the subtended territory might be relatively small, making interventional efforts to preserve the patency of the SB clinically irrelevant or even deleterious (more contrast, procedure length, unnecessary manipulation of the MB stent). There is no available information on the fate of the SB in the setting of STEMI in the literature and it is unlikely that angiographic follow-up studies will be performed, and therefore this study might reassure a “keep it simple” approach focusing on provisional stenting and a good angiographic result of the MB.
Long-term Follow-upThe present study is the first that explores the clinical outcomes of a BCL in STEMI as long as 5 years after the index primary PCI, finding similar long-term prognosis in patients with and without BCL in STEMI. Two studies have compared clinical outcomes at follow-up in this setting: a) Abdel-Hakim et al.14 studied an unselected population at 1-year, finding similar mortality (5% BCL vs 3% non-BCL; P = .15) but higher rates of a combined event (death, recurrent MI, and TLR) 23% BCL vs 20% non-BCL; P = .56 (at 1-year, we had 13% of the combined endpoint), and b) Dudek et al.,15 in a substudy of the HORIZONS-AMI randomized trial (which excluded patients with an intended 2-stent strategy) showed lower mortality at 3 years: 6.1% BCL vs 6.7% non-BCL; P = .72 but similar rates of a combined event (death from any cause, stroke, recurrent MI and unplanned revascularization) at 3 years (22% BCL vs 22% non-BCL; P = .92); while our study found 11% mortality in both groups and composite endpoint rates of 21% BIF vs 17% MC at 3 years.
If we contrast our study to others in stable setting with 5-year follow-up, the Nordic BIF study reported 5.9% all-cause death in the single strategy against 10.4% in the double stent strategy (P = .16), and composite event rates (all-cause death, MI, target vessel revascularization, and definite stent thrombosis) of 12% (simple strategy) vs 28% (double stent); P = .03.25 The 5-year results of the Bifurcations Bad Krozingen I study showed all-cause death of 7.9% (provisional T) vs 10% (routine T); P = .65; and composite event (all-cause death, MI, and TLR) rates occurring in 22.8% (provisional T) vs 22.9% (routine T); P = .91.26 Although we did not compare any BIF strategies, these results compare favorably against our series of a predominant single-stent strategy. Moreover, our study did not show any relevant increase in clinically-driven TLR or target vessel revascularization, or stent thrombosis during follow-up in the BCL group. There are only a few contemporary randomized STEMI trials reporting 5-year all-cause death after primary PCI, which ranged between 9% and 16%.27,28 Composite endpoints vary among studies, but the EXAMINATION trial reported a similar composite endpoint (all-cause death, recurrent MI or any revascularization) at 5 years (21% drug-eluting stent vs 26% bare metal stent).27 All these data are comparable to those in our study of an unselected population.
LimitationsThis is an observational, nonrandomized study; therefore uncontrolled variables may have had an impact on the outcomes comparison between groups. However, propensity score matching was used to reduce disparities in clinical characteristics. We decided to exclude left main culprit lesions, a rare finding in primary PCI with large subtended territory at risk and different long-term prognosis. The interventional strategy for primary PCI and BIF treatment was not standardized and therefore no conclusions on specific BIF PCI techniques in the setting of a STEMI can be made. The data on Medina classification of BCL should be interpreted with caution as it was assessed when TIMI ≥ 2 was obtained, and therefore it could be modified by the maneuvers to restore coronary flow. We had no data on antithrombotic drug prescription after discharge, which could potentially influence outcomes such as stent thrombosis. The timeframe of the study was wide, with obvious changes in therapy throughout the years, although the study represents clinical practice and the controls were paired according to quintiles of the index procedure date.
CONCLUSIONSA BCL can be found in 10% of primary or rescue PCI in STEMI patients, anatomically located mainly in left anterior descending artery-diagonal BIF. Primary PCI in this setting is technically more complex with increased procedural time and contrast use. However, compared with a propensity-matched cohort of non-BCL patients, a predominant single-stent strategy led to similar MB angiographic success, without differences in 30-day or 5-year clinical outcomes.
CONFLICTS OF INTERESTNone declared.
- –
Bifurcated lesions represent 15% to 20% of all PCIs, with worse long-term results, especially in terms of need for new revascularization. In the setting of STEMI, there is a paucity of data regarding the incidence of BIF lesions, and only a few studies have explored BIF outcomes, with either short-term results or limitations in patient selection.
- –
We present the second largest series of BCL in STEMI, the first with a propensity score matching control group, and the longest follow-up. A BCL was found in 10% of STEMI. The main finding of the present study was a similar short- and long-term prognosis in patients with and without BCL in STEMI.
- –
Bifurcation primary PCI was longer and technically more complex, with a lack of angiographic success in 15% of the BIF group. However, MB angiographic success was similar in both groups, leading to similar outcomes. This finding might reassure a “keep it simple” approach focusing on provisional stenting and a good angiographic result of the MB.