There are limited data on the preferred treatment strategy in ST-segment elevation myocardial infarction (STEMI) patients with bifurcation lesions. This study aimed to compare clinical outcomes between 1-stent and 2-stent strategies in STEMI patients with bifurcation lesions undergoing primary percutaneous coronary intervention (PCI).
MethodsThe COronary BIfurcation Stenting II is a retrospective multicenter registry of 2897 consecutive patients with bifurcation lesions undergoing PCI with drug-eluting stents from January 2003 through December 2009. Among the registered population, 367 (12.7%) patients had STEMI; of these, a 1-stent strategy was used in 304 patients and a 2-stent strategy in 63 patients; 77.1% of the patients received primary PCI with a first-generation drug-eluting stent. The inverse-probability-of-treatment-weighting method was used to adjust for confounding factors. The primary outcome was major adverse cardiovascular events (MACE), a composite of cardiac death, myocardial infarction, target lesion revascularization, and stent thrombosis.
ResultsThe median length of follow-up was 38 months. Postprocedural side branch diameter stenosis differed significantly between the 2 groups (1-stent vs 2-stent, 42.7% vs 9.7%; P < .001). After the performance of inverse-probability-of-treatment-weighting methods, the rate of MACE was significantly higher in the 2-stent group than in the 1-stent group (HR, 1.85; 95%CI, 1.19-2.87; P = .006), mainly driven by target lesion revascularization and stent thrombosis.
ConclusionsIn STEMI patients with bifurcation culprit lesions undergoing primary PCI, the 2-stent strategy had significantly higher rates of MACE than the 1-stent strategy, despite successful treatment of the side branch. However, this result should be interpreted with caution because this study does not reflect current practice.
Keywords
Coronary bifurcation lesions are frequent and are involved in 15% of percutaneous coronary interventions (PCIs).1 However, they remain the most challenging procedure in interventional cardiology, despite enormous advances in PCI technique and devices.2 Although many attempts have been made with a variety of different stenting techniques, current guidelines still recommend that provisional side branch (SB) stenting should be the initial approach in patients with bifurcation lesions, based on the results of previous randomized controlled trials.3 However, most of these trials comparing the outcomes between provisional 1-stenting and 2-stenting strategies excluded patients with ST-segment elevation myocardial infarction (STEMI) or included a limited number of cases.4–9
The prevalence of bifurcation culprit lesions in STEMI is approximately 10% and their impact on clinical outcomes has been evaluated in multiple studies.10–14 All of these data showed similar outcomes between bifurcation and nonbifurcation culprit lesions in patients with STEMI. However, there are limited data on the preferred treatment strategy in STEMI patients with bifurcation culprit lesions who receive primary PCI. Therefore, we sought to compare the clinical outcomes between 1-stent and 2-stent strategies for bifurcation culprit lesion in patients with STEMI undergoing primary PCI using a real-world registry.
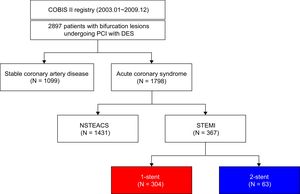
METHODSStudy PopulationThe COBIS (COronary BIfurcation Stenting) II registry is a retrospective, multicenter registry (NCT01642992) dedicated to patients with bifurcation lesions undergoing PCI with drug-eluting stents (DES). Between January 2003 and December 2009, 2897 consecutive patients were enrolled from 18 major coronary intervention centers in Korea. The inclusion criteria for the registry were bifurcation lesions treated with DES only, main vessel diameter ≥ 2.5mm, and SB diameter ≥ 2.3mm confirmed by quantitative coronary analysis. The exclusion criteria were cardiogenic shock, cardiopulmonary resuscitation, and protected left main disease. Among the registered population, 367 (12.7%) patients had STEMI and all of them have received primary PCI. Of these, the 1-stent strategy was applied in 304 (82.8%) patients and the 2-stent strategy in 63 (17.2%) patients (Figure 1). This study was supported by the Korean Society of Interventional Cardiology. The study protocol was approved by the institutional review board of each hospital.
Interventional ProcedureAll interventions were performed according to current practice guidelines. All patients received loading doses of aspirin (300mg) and clopidogrel (300-600mg) before coronary intervention unless they had previously received these antiplatelet medications. Anticoagulation during PCI was performed using low-molecular weight heparin or unfractionated heparin to achieve an activated clotting time of 250 to 300seconds. The treatment strategy for bifurcation lesion, access, type of DES, use of intravascular ultrasound, and duration of dual antiplatelet therapy were at the operator's discretion.
Data Collection and AnalysisPatient information, procedural data, and outcome data were collected using a web-based reporting system. Additional information was obtained from review of the medical records or telephone contact, if necessary. Coronary angiograms were reviewed and analyzed quantitatively by an independent core laboratory at Samsung Medical Center with a Centricity CA 1000 automated edge-detection system (GE, Waukesha, Wisconsin, United States) using standard qualitative and quantitative analyses and definitions.15 When the lesion characteristics were difficult to classify due to obstructive lesions with decreased Thrombolysis in Myocardial Infarction flow, the Medina classification and baseline quantitative coronary angiography was measured after restoring artery patency. True bifurcation lesions were defined as Medina classification type (1,1,1; 1,0,1, and 0,1,1) lesions.16 Bifurcation lesions were divided into 3 segments for quantitative coronary angiographic analysis: proximal main vessel, distal main vessel, and SB ostium. We determined the minimum luminal diameter and reference diameter for each segment. Percent diameter stenosis was calculated as 100 × (reference diameter-minimum luminal diameter/reference diameter). Bifurcation angle was defined as the angle between the distal main vessel and the SB at its origin using the angiographic projection with the widest separation of the 2 branches. An independent clinical event adjudicating committee reviewed all outcome data reported from the participating centers.
Definitions and OutcomesAngiographic success of the main vessel was defined as ≤ 30% residual stenosis with final Thrombolysis in Myocardial Infarction flow grade 3. Angiographic success of the SB was defined as residual stenosis ≤ 50% with final Thrombolysis in Myocardial Infarction flow grade 3.11 Procedural success of PCI was defined as angiographic success without associated in-hospital major clinical complications (death, myocardial infarction, stroke, emergency coronary artery bypass graft surgery).3 The primary endpoint was major adverse cardiovascular events (MACE), a composite of cardiac death, myocardial infarction, target lesion revascularization, and stent thrombosis (ST). All deaths were considered of cardiac cause unless obvious noncardiac causes could be identified. Myocardial infarction was defined as an elevation of creatine kinase-myocardial band or troponin level greater than the upper limit of normal with concomitant ischemic symptoms or electrocardiography findings indicative of ischemia. Periprocedural enzyme elevation was not included in this definition of myocardial infarction. Target lesion revascularization was defined as repeat PCI of the lesion within 5mm of the inserted stent. Stent thrombosis was defined using the definitions of the Academic Research Consortium as definite, probable, or possible.17 Both definite and probable cases were included as ST in this study. The timing of ST was stratified as early (within 1 month after the index procedure), late (between 1 month and 1 year), or very late (after 1 year).
Statistical AnalysisThe main comparison groups were the 1-stent vs 2-stent technique in patients with STEMI undergoing primary PCI. Categorical variables were compared using the chi-square test, and continuous variables were compared using the Student t test or Wilcoxon rank-sum test, as appropriate. The cumulative incidences of clinical events were calculated based on Kaplan-Meier censoring estimates and the log rank test was used to compare survival curves between the 2 groups. A Cox proportional hazard regression model was used to calculate hazard ratio (HR) and 95% confidence interval (95%CI) to compare the difference of events. The inverse-probability-of-treatment-weighting method was performed to reduce the possibility of biased effect estimates in observational studies.18,19 Variables selected for use in the inverse-probability-of-treatment-weighting method included age, sex, hypertension, diabetes mellitus, dyslipidemia, previous history of PCI, previous myocardial infarction, left ventricular ejection fraction, multivessel disease, left main bifurcation, stent type, true bifurcation, and SYNTAX score. An inverse probability weighted propensity-score adjusted Cox proportional hazard regression model was used to compare the clinical outcomes between the 1-stent and 2-stent techniques after adjustment for potential confounding factors. Statistical analyses were performed using R Statistical Software (version 3.2.5; R Foundation for Statistical Computing, Vienna, Austria) with P < .05 considered statistically significant.
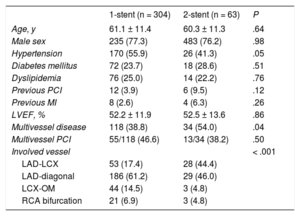
RESULTSBaseline Clinical CharacteristicsThe baseline clinical characteristics of STEMI patients according to treatment strategy are shown in Table 1. The 2-stent group had a higher proportion of multivessel disease and left main coronary artery involvement, but a lower proportion of hypertension compared with the 1-stent group. Other risk factors for cardiovascular disease were similar between the 1-stent and 2-stent strategy groups. In the subset of STEMI with multivessel disease, 44.7% of patients received multivessel PCI and there was no significantly difference of multivessel PCI between the 1-stent and 2-stent strategy groups.
Baseline Clinical and Angiographic Characteristics According to Treatment Strategy in Patients With Bifurcation Culprit Lesions Undergoing Primary PCI
| 1-stent (n = 304) | 2-stent (n = 63) | P | |
|---|---|---|---|
| Age, y | 61.1 ± 11.4 | 60.3 ± 11.3 | .64 |
| Male sex | 235 (77.3) | 483 (76.2) | .98 |
| Hypertension | 170 (55.9) | 26 (41.3) | .05 |
| Diabetes mellitus | 72 (23.7) | 18 (28.6) | .51 |
| Dyslipidemia | 76 (25.0) | 14 (22.2) | .76 |
| Previous PCI | 12 (3.9) | 6 (9.5) | .12 |
| Previous MI | 8 (2.6) | 4 (6.3) | .26 |
| LVEF, % | 52.2 ± 11.9 | 52.5 ± 13.6 | .86 |
| Multivessel disease | 118 (38.8) | 34 (54.0) | .04 |
| Multivessel PCI | 55/118 (46.6) | 13/34 (38.2) | .50 |
| Involved vessel | < .001 | ||
| LAD-LCX | 53 (17.4) | 28 (44.4) | |
| LAD-diagonal | 186 (61.2) | 29 (46.0) | |
| LCX-OM | 44 (14.5) | 3 (4.8) | |
| RCA bifurcation | 21 (6.9) | 3 (4.8) | |
LAD, left anterior descending artery; LCX, left circumflex artery; LVEF, left ventricular ejection fraction; MI, myocardial infarction; OM, obtuse marginal; PCI, percutaneous coronary intervention; RCA, right coronary artery.
Data are presented as mean ± standard deviation or No. (%).
Table 2 presents the lesion and procedural characteristics of the study population. The proportion of true bifurcation and procedural success rates of SB were higher in the 2-stent group than in the 1-stent group. The 2-stent group had higher rates of final kissing-balloon inflation and intravascular imaging compared with the 1-stent group. In addition, total stent length was significantly longer in the 2-stent group than in the 1-stent group. There were no significant differences between the 2 groups in procedural success rates of main vessel or acute closure of both main vessel and SB during PCI.
Lesion and Procedural Characteristics According to Treatment Strategy in Patients With Bifurcation Culprit Lesions Undergoing Primary PCI
| 1-stent (n = 304) | 2-stent (n = 63) | P | |
|---|---|---|---|
| No. of stents used | 1.48 ± 0.76 | 2.35 ± 0.60 | <.001 |
| Total stent length | 30.1 ± 15.0 | 52.8 ± 17.3 | <.001 |
| Stent type | .02 | ||
| First-generation DES | 227 (74.7) | 56 (88.9) | |
| Second-generation DES | 77 (25.3) | 7 (11.1) | |
| Final kissing balloon | 60 (20.1) | 53 (84.1) | <.001 |
| Intravascular imaging | 68 (22.4) | 34 (54.0) | <.001 |
| True bifurcation | 145 (47.7) | 48 (76.2) | <.001 |
| Medina classification | <.001 | ||
| 1,1,1 | 89 (29.3) | 26 (41.3) | |
| 1,0,1 | 22 (7.2) | 6 (9.5) | |
| 0,1,1 | 34 (11.2) | 16 (25.4) | |
| 1,0,0 | 46 (15.1) | 1 (1.6) | |
| 1,1,0 | 44 (14.5) | 6 (9.5) | |
| 0,1,0 | 65 (21.4) | 5 (7.9) | |
| 0,0,1 | 4 (1.3) | 3 (4.8) | |
| SYNTAX score | 16.5 [11.0-22.5] | 19.0 [13.5-23.0] | .05 |
| Main vessel | |||
| NC ballooning | 92 (30.3) | 18 (28.6) | .91 |
| Angiographic success | 298 (98.0) | 61 (96.8) | .90 |
| Final TIMI flow < 3 | 6 (2.0) | 1 (1.6) | .84 |
| Vessel closure during PCI | 32 (10.5) | 6 (9.5) | .82 |
| SB | |||
| NC ballooning | 17 (5.6) | 12 (19.0) | .001 |
| Angiographic success | 183 (60.2) | 61 (96.8) | <.001 |
| Final TIMI flow < 3 | 19 (6.3) | 1 (1.6) | .14 |
| Vessel closure during PCI | 38 (12.5) | 8 (12.7) | .70 |
| Bifurcation angle (degree) | 59.9 [43.0-75.1] | 62.2 [46.5-79.0] | .24 |
| 1-stenting without SB ballooning | 212 (69.7) | — | |
| 1-stenting with SB ballooning | 92 (30.3) | — | |
| Classic T-stenting | — | 6 (9.5) | |
| Modified-T or TAP | — | 17 (27.0) | |
| Crush | — | 29 (46.0) | |
| Kissing or V stenting | — | 8 (12.7) | |
| Culottes | — | 3 (4.8) | |
| QCA after procedure | |||
| MV RD, mm | 3.0 [2.8-3.4] | 3.2 [2.9-3.5] | .03 |
| SB RD, mm | 2.4 [2.3-2.6] | 2.5 [2.3-2.8] | .01 |
| MV MLD, mm | 2.6 [2.3-2.9] | 2.7 [2.4-2.9] | .20 |
| SB MLD, mm | 1.4 [1.0-1.9] | 2.3 [2.0-2.6] | <.001 |
| MV diameter stenosis, % | 14.8 [6.6-22.6] | 15.7 [8.4-23.5] | .31 |
| SB diameter stenosis, % | 42.7 [27.0-58.8] | 9.7 [3.0-18.3] | <.001 |
DES, drug-eluting stent; MLD, minimal luminal diameter; MV, main vessel; NC, noncompliant; PCI, percutaneous coronary intervention; QCA, quantitative coronary analysis; SB, side branch; RD, reference diameter; TAP, T and protrusion; TIMI, Thrombolysis in Myocardial Infarction.
Data are expressed as No. (%), mean ± standard deviation or median [interquartile range].
On quantitative coronary angiographic analysis of postprocedural data, there was no significant difference in main vessel percent diameter stenosis between the 2 groups. However, percent diameter stenosis of the SB was more improved in the 2-stent group (Table 2).
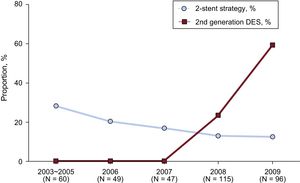
Temporal Trends of Treatment Strategy and Stent TypeFigure 2 shows trends of the proportion of 2-stent strategy and second-generation DES use according to year of enrollment. Use of second-generation DES rapidly increased after 2007 and was significantly lower in the 2-stent strategy group than in 1-stent strategy group (Table 2, Figure 2). In addition, cases from earlier years received the 2-stent strategy more frequently and it seemed to decrease gradually over time (Figure 2).
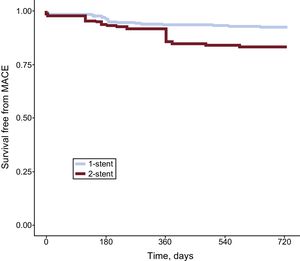
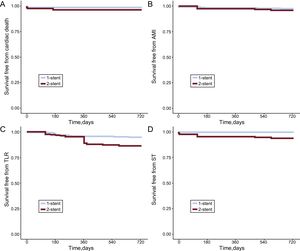
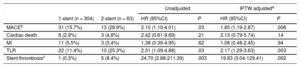
Clinical OutcomeDuring the median follow-up of 38 months [interquartile range 26-50], 44 MACEs occurred among the 367 STEMI patients with bifurcation culprit lesions, including 9 cardiac deaths, 14 myocardial infarctions, 6 STs, and 32 target lesion revascularizations. Compared with the 1-stent strategy, the 2-stent strategy was associated with higher rates of MACE (1-stent vs 2-stent; 15.7% vs 28.9%, HR, 2.10; 95%CI, 1.10-4.01; P = .03) (Table 3, Figure 3), which was mainly driven by ST (0.3% vs 8.4%; HR, 24.70; 95%CI, 2.88-211.39; P = .003) and target lesion revascularization (11.4% vs 25.3%; HR, 2.31; 95%CI, 1.09-4.88; P = .03) (Table 3, Figure 4). Rates of cardiac death and MI were not significantly different between the 2 groups.
Clinical Outcomes of Total Population According to Treatment Strategy in Patients With Bifurcation Culprit Lesions Undergoing Primary PCI
| Unadjusted | IPTW adjusteda | |||||
|---|---|---|---|---|---|---|
| 1-stent (n = 304) | 2-stent (n = 63) | HR (95%CI) | P | HR (95%CI) | P | |
| MACEb | 31 (15.7%) | 13 (28.9%) | 2.10 (1.10-4.01) | .03 | 1.85 (1.19-2.87) | .006 |
| Cardiac death | 6 (2.9%) | 3 (4.8%) | 2.42 (0.61-9.69) | .21 | 2.13 (0.79-5.74) | .14 |
| MI | 11 (5.5%) | 3 (5.4%) | 1.38 (0.39-4.95) | .62 | 1.08 (0.48-2.45) | .94 |
| TLR | 22 (11.4%) | 10 (25.3%) | 2.31 (1.09-4.88) | .03 | 2.17 (1.29-3.63) | .003 |
| Stent thrombosisc | 1 (0.3%) | 5 (8.4%) | 24.70 (2.88-211.39) | .003 | 19.83 (3.04-129.41) | .002 |
95%CI, 95% confidence interval; IPTW, inverse-probability-of-treatment-weighting; MI, myocardial infarction; HR, hazard ratio; MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention; TLR, target lesion revascularization.
Values are expressed as No. (%). The cumulative incidence of events is presented as Kaplan-Meier estimates.
Inverse-probability-of-treatment-weighting adjusted Kaplan-Meier curves of primary outcomes according to treatment strategy. Inverse-probability-of-treatment-weighting adjusted Kaplan-Meier curves for MACE in patients with bifurcation culprit lesions undergoing primary PCI according to the 1-stent or 2-stent strategy. MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention.
Inverse-probability-of-treatment-weighting adjusted Kaplan-Meier curves of secondary outcomes according to treatment strategy. Inverse-probability-of-treatment-weighting adjusted Kaplan-Meier curves for cardiac death (A), AMI (B), TLR (C), and ST (D) in patients with bifurcation culprit lesions undergoing primary PCI according to the 1-stent or 2-stent strategy. AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; ST, stent thrombosis; TLR, target lesion revascularization.
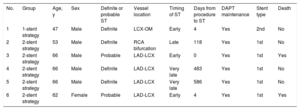
Table 4 shows the detailed characteristics of patients with ST. Most cases occurred in the left main lesion treated with the 2-stent strategy. Three cases occurred early (within 1 month) and the other 3 cases occurred late (between 1 month and 1 year) or very late (after 1 year). All patients developed ST during maintenance of dual antiplatelet therapy.
Clinical and Lesion Characteristics of Patients With Stent Thrombosis
| No. | Group | Age, y | Sex | Definite or probable ST | Vessel location | Timing of ST | Days from procedure to ST | DAPT maintenance | Stent type | Death |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1-stent strategy | 47 | Male | Definite | LCX-OM | Early | 4 | Yes | 2nd | No |
| 2 | 2-stent strategy | 53 | Male | Definite | RCA bifurcation | Late | 118 | Yes | 1st | No |
| 3 | 2-stent strategy | 66 | Male | Probable | LAD-LCX | Early | 0 | Yes | 1st | Yes |
| 4 | 2-stent strategy | 66 | Male | Definite | LAD-LCX | Very late | 483 | Yes | 1st | No |
| 5 | 2-stent strategy | 66 | Male | Definite | LAD-LCX | Very late | 586 | Yes | 1st | No |
| 6 | 2-stent strategy | 62 | Female | Probable | LAD-LCX | Early | 4 | Yes | 1st | Yes |
DAPT, dual antiplatelet therapy; LAD, left anterior descending artery; LCX, left circumflex artery; OM, obtuse marginal; RCA, right coronary artery; ST, stent thrombosis.
After adjustment using the inverse-probability-of-treatment-weighting method, trends of clinical outcomes were similar to the results of overall data. The C-statistic for the propensity-score based prediction model was 0.87 (95%CI, 0.83-0.91), which indicates good discrimination (Hosmer-Lemeshow goodness of fit P = .68). The rate of MACE was significantly higher in the 2-stent strategy group compared with the 1-stent strategy (adjusted HR, 1.85; 95%CI, 1.19-2.87; P = .006) (Table 3). In addition, ST (adjusted HR, 19.83; 95%CI, 3.04-129.41; P = .002) and target lesion revascularization (adjusted HR, 2.17; 95%CI, 1.29-3.63; P = .003) occurred more frequently in the 2-stent group than in the 1-stent group (Table 3).
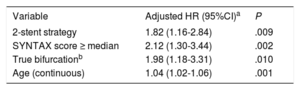
Independent Predictors of Major Adverse Cardiovascular EventsIn the multivariate inverse-probability weighted Cox proportional hazard model, the 2-stent strategy was an independent predictor of MACE (adjusted HR, 1.82; 95%CI, 1.16-2.84; P = .009). This result was consistent after performing competing risk analysis to adjust for noncardiovascular death (adjusted HR, 1.75; 95%CI, 1.16-2.65; P = .008).20,21 Noncardiovascular death occurred in 6 patients during follow-up. Other independent predictors included SYNTAX score (adjusted HR, 2.12; 95%CI, 1.30-3.44; P = .002), age (adjusted HR, 1.04; 95%CI, 1.02-1.06; P = .001), and true bifurcation lesion (adjusted HR, 1.98; 95%CI, 1.18-3.31; P = .010) (Table 5).
Independent Predictors of MACE in the IPTW-adjusted Model
| Variable | Adjusted HR (95%CI)a | P |
|---|---|---|
| 2-stent strategy | 1.82 (1.16-2.84) | .009 |
| SYNTAX score ≥ median | 2.12 (1.30-3.44) | .002 |
| True bifurcationb | 1.98 (1.18-3.31) | .010 |
| Age (continuous) | 1.04 (1.02-1.06) | .001 |
95%CI, 95% confidence interval; HR, hazard ratio; IPTW, inverse-probability-of-treatment-weighting; MACE, major adverse cardiovascular events.
In the present study, we investigated the associations between clinical outcomes and the treatment strategy of bifurcation culprit lesions in STEMI patients with bifurcation culprit lesions undergoing primary PCI. The main findings were as follows. First, among patients with bifurcation culprit lesions who presented with STEMI and underwent primary PCI, the rate of occurrence of MACE was significantly higher in the 2-stent group than in the 1-stent group, despite successful treatment of the SB. In particular, these results were maintained after inverse-probability-of-treatment-weighting analysis to reduce selection bias. Second, in the multivariate inverse-probability weighted Cox regression model, 2-stenting strategy, SYNTAX score, true bifurcation, and old age were independent predictors of MACE in STEMI patients with bifurcation culprit lesions.
The Impact of Bifurcation Culprit Lesion in ST-segment Elevation Myocardial InfarctionST-segment elevation myocardial infarction is a clinical syndrome defined by characteristic symptoms of myocardial ischemia in association with persistent electrocardiographic ST elevation and subsequent release of biomarkers of myocardial necrosis. Primary PCI is the preferred reperfusion strategy for patients with STEMI.22,23 The most important principle in the treatment of STEMI is rapid reperfusion of the occluded coronary artery; in this regard, a simple method such as the 1-stent strategy with a provisional approach to reduce the procedure time may be better. There are 5 previous studies that evaluated the impact of bifurcation lesions on angiographic and clinical outcomes of STEMI patients undergoing primary PCI.10–14 Although the procedural time was a conflicting factor, all of these studies showed similar clinical outcomes of STEMI with or without bifurcation lesions. However, more than 90% of the participants enrolled in the previous 4 studies underwent a 1-stent strategy, and there were no data comparing clinical outcomes and treatment strategy. In contrast to previous studies, the present study included a higher proportion of patients undergoing the 2-stent strategy; therefore, we could analyze the preferred treatment strategy for STEMI patients with bifurcation culprit lesions.
Treatment Technique in ST-segment Elevation Myocardial Infarction With Bifurcation Culprit LesionBifurcation lesion remains one of the most challenging aspects in interventional cardiology and is associated with a lower procedural success rate and increased rates of long-term adverse cardiac events.24 A previous study by our group indicated that MACE occurred more frequently in patients with acute coronary syndrome than in those with stable disease.25 Consistent with a previous study, clinical event rates of our study population were higher than in most previous trials, which excluded patients with STEMI and bifurcation lesion.4–8 The DKCRUSH-II9 was the only randomized controlled trial that included STEMI patients in a comparison between provisional 1-stent and 2-stent strategies. In that study, 12.7% of the randomly assigned population with bifurcation lesion were STEMI patients. Interestingly, the proportion of STEMI patients in our registry data were also 12.7% for nonrandomized registry data.9 The post-hoc analysis of DKCRUSH II showed that clinical outcomes of STEMI patients treated with the double kissing crush technique were comparable to those of patients treated with the provisional 1-stent technique, but there are several limitations in the application of these findings to clinical practice.26 First, it is difficult to determine the preferred strategy due to the very small sample size (33 patients with double kissing crush technique and 30 patients with provisional stenting). Second, patients with left main bifurcation lesion were excluded from the analysis. In contrast to the previous study, the results of our study indicated that the 2-stent strategy was associated with higher rates of MACE than the provisional 1-stent strategy in STEMI patients with bifurcation culprit lesion. In addition, the 2-stent technique was an independent predictor of MACE, mainly due to higher rates of target lesion revascularization and ST. Our data also showed that the proportion of 2-stent strategy gradually decreased over time in the treatment of bifurcation culprit lesion for STEMI patients. This result might have been affected by several large randomized studies, which favored the 1-stent strategy and were published in the late 2000s.4–8 Consistent with previous studies, patients treated with 1-stent strategy had favorable outcomes even in STEMI patients with bifurcation culprit lesion. However, this study was conducted at the same era as previous randomized controlled trials and thus it may not reflect current clinical practice. Well-designed randomized controlled studies would be helpful to confirm this result.
Independent Predictors of Major Adverse Cardiovascular EventsThe present study indicated that independent predictors of MACE were the 2-stent strategy, SYNTAX score, true bifurcation, and old age. SYNTAX score is a comprehensive angiographic scoring system based on coronary anatomy and lesion characteristics27 that has been validated as an independent predictor in patients with STEMI.28 In agreement with the previous study, our study showed that SYNTAX score was an independent predictor of MACE in STEMI patients with bifurcation culprit lesion. In addition, some previous studies indicated that true bifurcation lesion was associated with a higher incidence of procedural complications and unfavorable long-term outcomes compared with other types of lesions.29,30 These results were confirmed in our study. Therefore, physicians should carefully consider the treatment strategy in patients requiring a 2-stent technique with high SYNTAX score or true bifurcation.
Stent ThrombosisStenting bifurcation lesions with DES are associated with an increased risk of ST.31 Ong et al.32 reported that bifurcation stenting (using crush, t-stent, or culotte crush technique) in the setting of acute myocardial infarction was a highly significant independent risk factor for ST. In agreement with previous studies, patients treated with the 2-stent strategy had a higher risk of ST than those treated with the 1-stent strategy. Interestingly, in our study population, all cases of ST occurred during maintenance with dual antiplatelet therapy. In addition, most cases of ST occurred after left main vessel treatment with 2-stenting. These results suggest that 2-stent implantation, especially in the left main vessel, requires additional attention despite maintenance of prolonged dual antiplatelet therapy. However, these results should be interpreted with caution because small vessel ST could remain underdiagnosed.
LimitationsThe present study had several limitations. First, it was a nonrandomized, observational study, which may have affected the results because of confounding factors. In addition, the selection of treatment strategy, medication, stent type, and stenting technique was based on the physician's preference. In particular, some patients in the 2-stent strategy group did not receive the final kissing balloon inflation, which was strongly recommended in bifurcation lesions treated with complex procedures. This could have affected the poorer prognosis of the 2-stent strategy group. Although an inverse-probability-of-treatment-weighting analysis was used to adjust the baseline differences and to reduce selection bias, unmeasured variables were not correctable. Second, some critical variables related to STEMI, such as baseline Thrombolysis in Myocardial Infarction flow, could not be presented because the COBIS II registry focused on bifurcation lesions, not STEMI. Third, sample sizes were probably inadequate for the analysis of ST risk between the 2 groups. In addition, it is not certain that increased risk of ST in the 2-stent group was associated only with the 2-stent strategy, because almost all cases of ST occurred in patients who received first-generation DES, which was more frequently used in the 2-stent group. However, to the best of our knowledge, this is the largest study to compare 1-stent vs 2-stent in STEMI patients with bifurcation culprit lesion. Fourth, we excluded patients with cardiogenic shock or cardiopulmonary resuscitation. In addition, our data did not contain patients who underwent coronary artery bypass graft surgery or balloon-angioplasty only PCI. Therefore, the current results cannot be extrapolated to these patient subsets. Fifth, the primary outcome did not include noncardiovascular death and therefore patients who died for noncardiovascular cause before occurring MACE will be outside the risk pool. Although competing risk analysis was performed and showed consistent results, it might have been affected by very low rates of noncardiovascular death. Furthermore, we had no data on reasons for repeat revascularization of the target lesion, which is one of the main contributing factors of the primary outcome. Therefore, it is possible that the differences in target lesion revascularization might be derived from a nonclinically driven scheduled follow-up angiography. Finally, new P2Y12 inhibitors, such as ticagrelor or prasugrel, which have demonstrated superior outcomes compared with clopidogrel in acute coronary syndrome, were not available in this study due to the enrollment date of the study population. In addition, most of the patients were treated with first-generation DES, which are not used currently. Although few data have reported the efficacy between first- and second-generation DES in bifurcation lesions, second-generation DES might reduce the risk of adverse cardiac events due to reduced strut thickness and improvement in polymer biocompatibility and drug elution. Therefore, a larger study with second-generation DES is needed to confirm the results of the present study and to evaluate the effect of second-generation DES for bifurcation lesions in STEMI patients undergoing primary PCI.
CONCLUSIONSIn STEMI patients with bifurcation culprit lesions undergoing primary PCI, the 2-stent strategy was associated with higher rates of MACE, mainly driven by target lesion revascularization and ST, compared with the 1-stent strategy, despite successful treatment of the SB lesion. If possible, the 1-stent strategy should initially be considered the preferred approach for the treatment of coronary bifurcation culprit lesions in the setting of primary PCI for STEMI. However, careful interpretation is needed because the present study does not reflect current clinical practice and adverse events might be affected by other confounding factors due to the retrospective nature of the study
FUNDINGThis work was supported by the Korean Society of Interventional Cardiology, Seoul, Republic of Korea.
CONFLICTS OF INTERESTNone declared.
- -
Although the provisional 1-stent strategy is preferred as a first approach in bifurcation lesions, most studies have been performed in patients with stable ischemic heart disease.
- -
Limited data are available on the preferred treatment strategy in STEMI patients with bifurcation lesions who received primary PCI.
- -
This study demonstrates that the rate of MACE was significantly higher in the 2-stent group than in the 1-stent group, despite successful treatment of the SB. These results were mainly caused by ST and target lesion revascularization. However, most of enrolled participants received PCI with first-generation DES, which is no longer used.
- -
Therefore, a careful approach may be needed for treatment decisions in bifurcation STEMI patients requiring a 2-stent technique. In addition, a large randomized controlled trial would be needed using second-generation DES for confirmation of this study.
.
We strongly appreciate the statistical support from Joonghyun Ahn, MS, and Keumhee Carriere, PhD.