To the Editor,
In 1999 we reported the results of the first randomized clinical trial using a biodegradable collagen-elastin patch (OVI SA, Martillac, France) as a pericardial substitute.1 In this study, 25 patients undergoing surgical coronary revascularization received a membrane implant made of an elastin complex with bovine collagen reinforced with reabsorbable polygycolate mesh. Results showed no local or systemic inflammatory reaction or hemodynamic changes postoperatively.
Now we report the case of one of these patients that received a pericardial substitute. Eighty-nine months after surgery, re-operation was required due to the development of aortic valvulopathy.
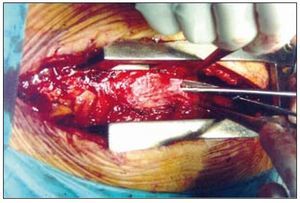
After reopening the sternum (Figure 1), surgical exploration showed a neo-pericardium consisting of a solid, well-defined, membranous laminate, which was greyish in color and approximately 1 mm thick. The membrane uniformly enveloped the epicardium and was clearly distinguishable. Anatomic dissection positions were well defined; a small number of loose, easily removed adhesions by digital dissection were present. There was no evidence of constriction, restriction, or inflammatory reaction in the epicardium, making the identification of mediastinal structures and by-pass conduits relatively easy.
Figure 1. Intra-operative image showing the neo-pericardium after reopening the sternum where a well-defined structure can be seen.
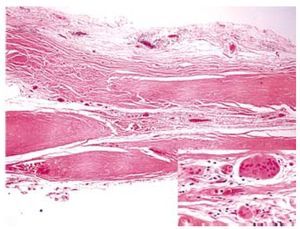
Upon histological analysis of the membrane (Figure 2), bands of collagenized, fibrous tissues were observed with isolated collections of a sparse inflammatory cell infiltration of multinucleated giant cells and a foreign body-type inflammatory reaction, composed of lymphocytes, plasma cells, and histiocytes.
Figure 2. Hematoxylin and eosin stained slide of the re-absorbable collagen-elastin membrane with sparse inflammatory cell infiltration composed of lymphocytes, plasma cells, and histiocytes (see enlargement).
In previous laboratory tests, it was found that peptides released during the degradation of the collagen-elastin complex inhibited native elastase and collagenase activity and minimized the local inflammatory response. Reabsorption of the collagen-elastin material occurs simultaneously with the synthesis of a neo-pericardium, with the patch acting as a framework to facilitate the incorporation of mesothelium-like cells on the epicardial face of the patch.2
In patients with a history of coronary artery bypass grafting (CABG), the requirement for a repeat CABG is dependent upon progression of atherosclerotic disease and the stability and patency of vein grafts. The necessity for re-operation increases progressively and has a direct relationship with the time elapsed since surgery. The need for a second myocardial revascularization after 5, 10, 15, and 20 years is reported to be approximately 4, 12, 27, and 40%, respectively.3
The most accepted opinion is that reoperations are associated with an increase in morbidity and mortality not only derived from patient-specific clinical factors (ie, older age and increased comorbidities) but also from the complexity of the surgical technique due to the absence of pericardial closure after initial heart surgeryand the development of adhesions. Reoperation status remained an independent predictor of operative death after adjusting for confounding factors. The aorta, right ventricle, and bypass grafts may adhere to the underside of the sternum and can be easily injured at reoperation. In-hospital mortality for patients undergoing cardiac reoperation is higher than that of patients undergoing primary surgical intervention4,5. Previous surgical revascularization is a predictive factor for early mortality.6
One of the methods thought to reduce the morbidity and mortality associated with reoperation is the use of pericardial substitutes, serving to conserve the anatomical relationship. The heterogeneity of available materials, both synthetic and biological, is an indicator of the fact that an ideal tissue substitute has yet to be identified.
In conclusion the findings from the patient presented here with the results from a short-term study suggest that the biodegradable collagen-elastin membrane constitutes a safe, effective option for pericardial closure. At reoperation, the use of this membrane appears to reduce the risk of structural damage during dissection while also reducing surgery time and morbidity/mortality.