A 56-year-old man with no cardiovascular risk factors was admitted to our hospital for a 1-week history of exertional angina and asthenia. His medical history included Behçet disease with a previous hospitalization in the ICU for massive hemoptysis related to pulmonary aneurysms requiring a right lung lobectomy, and hepatitis B infection, likely transmitted by blood transfusion. The disease was currently in remission, and he was receiving immunosuppressive (interferon alfa-2a) and antiviral (entecavir) therapy.
On admission, the patient was asymptomatic. An electrocardiogram showed sinus rhythm with a 2:1 atrioventricular block and a wide QRS with right bundle branch block and left anterior hemiblock morphology. Transthoracic echocardiography showed no anomalies.
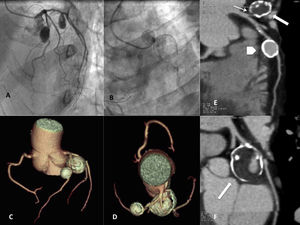
Coronary angiography (Figure A and B), depicted 2 calcified aneurysms in the proximal segment of the left anterior descending artery and the circumflex artery. The aneurysm in the circumflex was partially thrombosed, and distal flow was slowed. Computed tomography coronary angiography confirmed the presence of 2 saccular aneurysms (Figure C and D). The multiplanar reconstructions showed the true size of the aneurysm in the circumflex artery (30×24mm) (Figure E and F, arrows), with a narrow neck (Figure E, thin arrow), calcified wall (“eggshell” appearance), thrombus, and irregular residual lumen. The aneurysm in the left anterior descending artery was smaller (15×14mm; Figure 1E, arrowhead), and also showed a wall calcification.
A and B, coronary angiography; aneurysmal dilatations in the proximal segment of the left anterior descending artery and the circumflex artery. C and D, computed tomography angiography showing 2 calcified, saccular, coronary artery aneurysms; the larger one is located in the circumflex artery. E and F, multiplanar reconstructions. Circumflex artery aneurysm, 30×24mm in size (arrows), with a narrow neck (E, thin arrow), calcified wall (“eggshell” appearance), thrombus (interior, low-density area) and irregular residual lumen; 15×14mm aneurysm in the left anterior descending artery (E, arrowhead), also showing a calcified wall.
Following electrophysiological study, which confirmed the infra-Hisian location of the atrioventricular block, a definitive AAI-DDDR dual chamber pacemaker was implanted. To control the aneurysms and revascularize, aortocoronary bypass surgery was then undertaken, with implantation of the left internal mammary artery to the left anterior descending artery and the right internal mammary artery in Y configuration to the obtuse marginal artery. Both aneurysms were ligated. The patient was discharged on the fifth day following surgery. At the 6-month follow-up visit, he was asymptomatic and free from angina.
Behçet disease is a chronic, multisystemic, inflammatory condition, whose main histopathological characteristic is vasculitis of the large, medium, and small vessels. The etiology of Behçet disease is unknown. Viral, bacterial, genetic, environmental, toxic, and immune factors have been implicated. The most widely recognized genetic factor is HLA-B51. The condition has a low prevalence in Spain (5-10/100 000 population), but it is more widespread in countries along the “Silk Road” (80-370/10 000 in Turkey and 3-20/10 000 in Asian countries). Age of presentation is usually the third or fourth decade of life. Cardiac involvement is estimated to occur in 6% of patients and implies a poor prognosis; hence, a prompt diagnosis is needed.1 The cardiac manifestations include pericarditis, myocarditis, valve injury, endomyocardial fibrosis, acute myocardial infarction, intracardiac thrombosis, and conduction disturbances. Coronary aneurysm is one of the less common forms of presentation (0.5% of patients). Most are single lesions occurring in the right coronary vessels; coronary aneurysms are less common in the left coronary tree. The pathophysiologic mechanism includes obliterative endarteritis of the vasa vasorum and perivascular infiltration by mononuclear cells, with destruction of the media and weakening of the vessel wall.2,3 The form of presentation is usually an acute coronary syndrome. Noninvasive imaging techniques (coronary computed tomography, transthoracic or transesophageal echocardiography or magnetic resonance imaging) are useful for diagnosis, and coronary angiography is the diagnostic technique of choice.2,3 Intravascular ultrasound enables differentiation between the components of the coronary artery wall and is helpful to distinguish between a true aneurysm and pseudoaneurysm. However, it is less useful in large or thrombosed aneurysms.4 The finding of cardiac involvement in a patient with Behçet disease should lead to a search for other affected vascular territories by computed tomography angiography, magnetic resonance angiography, or abdominal ultrasound. There are no treatment recommendations for this condition. The related literature contains 4 cases treated with surgery, which is reserved for huge (> 20mm), rapidly growing aneurysms and those with a high risk of rupture.2,5 Atrioventricular block is an uncommon manifestation of unknown etiology in Behçet disease that has been associated with inflammation of the atrioventricular node and surrounding conduction tissue. Definitive pacemaker implantation is usually required.1 There is no specific treatment for the disease. The aim is to reverse the symptoms and prevent permanent injury. Complete remission of cardiac involvement has been associated with the use of immunosuppressive therapy, colchicine, and anticoagulants.1,6