To the Editor,
Cardiac rupture during stress testing is uncommon and rarely reported, with less than ten cases described in the scientific literature. We present a patient with left ventricular free wall rupture one week after a nontransmural acute myocardial infarction (AMI), when undergoing conventional stress testing.
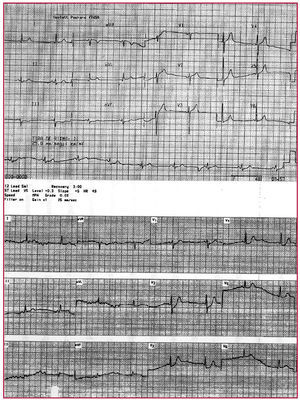
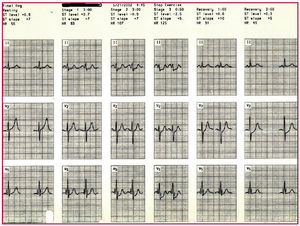
A 70-year-old man, ex-smoker, with no other cardiovascular risk factors, was admitted in May 2002 for precordial pain of coronary characteristics, lasting 1 h, with minimal ST segment depression in LII, LIII, and aVF, and elevated concentrations of creatine kinase MB (CK-MB) isoenzyme (1256/65 U/L). He was diagnosed with non-Q-wave AMI and treated with heparin at anticoagulant doses, aspirin, nitrates, and atenolol. Echocardiography performed at 4 days showed inferolateral hypokinesia with normal ejection fraction. In subsequent follow-ups, the patient remained asymptomatic with no changes in the electrocardiogram). At 7 days, a stress test was performed according to the Bruce protocol; the patient did not experience angina, although there was ST segment depression of 2 mm in V4 through V5 and V6 at 6 min and 50 s (83% of maximum theoretical heart rate) before the test was stopped. At 3 min of rest, he presented severe pain in the back, dizziness, obnubilation, and loss of consciousness and pulse, with sinus bradycardia, persistence of ST segment depression, and increased R voltage in V2 and V3 (Figures 1 and 2). Resuscitation maneuvers and fluid therapy were initiated. The echocardiogram showed considerable pericardial effusion. Drawing 15 mL of blood during pericardiocentesis brought blood pressure and heart rate back to normal. The patient was then transferred to the coronary unit, where he progressed well with conservative treatment. Four years after the event, he remains asymptomatic.
Figure 1. Electrocardiogram at the time of admission and 3 min following exercise, when the patient presented electromechanical dissociation. Note the ST segment depression from V1 to V4 and increased R voltage in V2 and V3.
Figure 2. Electrocardiographic sequence of the stress test
Ventricular free wall rupture is ten-fold more common than septum or papillary muscle rupture and is a rare complication of AMI, with a high mortality. It has a bimodal presentation with greater incidence in the first 24 h and another peak at 3-6 days. In our case, rupture probably occurred at a very early stage of a posterior reinfarction during the stress test, when the myocytes are not necrotic but are severely ischemic. Late fibrinolysis, advanced age, female sex, hypertension, absence of prior history of ischemic heart disease, first transmural AMI, marked ST segment elevation, anterior location, obstruction of the culprit artery, and use of corticosteroids or nonsteroidal anti-inflammatories increase the risk.1,2
Ventricular free wall rupture usually presents as cardiac tamponade with electromechanical dissociation, progressive sinus bradycardia followed by escape rhythm, head and neck cyanosis, and jugular vein enlargement. It may be associated with exertion (coughing, defecation, vomiting), but few cases have been reported with the stress test.3 Although a stress test one week after AMI is safe, an incidence of 0.3% for AMI or cardiac rupture has been described.4 Echocardiography confirms the diagnosis by visualization of pericardial effusion and absence of cardiac motion despite sinus rhythm. Immediate pericardiocentesis associated with increased fluid volume and surgical repair may save some patients. Some groups postulate conservative treatment.5
This case describes a rare, but severe complication of the stress test in a patient in whom the initial disease consisted of a small, probably inferior necrosis without ST segment elevation (unusual characteristic). The stress test showed ECG changes indicative of posterior infarction and left ventricular free wall rupture; however, the patient has survived without surgical treatment at 4 years from the episode.