We have read with interest the expert document1 on the organization of the cardiogenic shock code in Spain. Overall, we agree that the shock code must be correctly organized and involve a gradation of care in the participating centers to improve and optimize the available resources. It is on this latter point that we diverge from the views expressed in the document. It is well known that the first step in the appropriate planning of health care is to quantify the available resources.2 Spain has a practically equal number of centers with on-site catheterization and infarction code programs with and without cardiac surgery,3 and this latter type of center is not represented in the document,1 despite covering almost half of the Spanish population. The leading cause of cardiogenic shock is acute myocardial infarction.4 Its most effective treatment is percutaneous revascularization of the culprit artery (primary percutaneous coronary intervention), which should be performed as soon as possible.5 This procedure should be conducted in the corresponding infarction code center, and this action takes precedence over more complex procedures, as reported recently.6
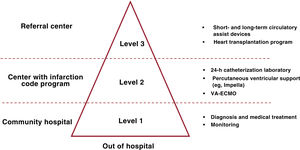
In the expert document, the hierarchy established for the level of care of the centers ranges from “level 3” (regional hospitals) to “level 2” (hospitals with cardiac surgery and an infarction code program), and the document states that, in this type of center, percutaneous techniques can be implemented for the management of shock (percutaneous coronary intervention with or without short-term mechanical circulatory support) and that these approaches are generally effective. “Level 1” is reserved for patients refractory to treatment or with particularly profound cardiogenic shock. This ranking of the different levels of care ignores centers with an infarction code program but without cardiac surgery, which, as mentioned above, represent practically half of all centers and nowadays provide coverage to a population of between 15 and 20 million people in Spain. These hospitals currently provide appropriate care to this type of patient, which includes short-term percutaneous support (involving balloon pump, Impella, or even extracorporeal membrane oxygenation [ECMO]). Crucially, excellent outcomes are achieved without the need for on-site cardiac surgery. In this regard, the cardiogenic shock organization document of the Department of Health of Catalonia (figure 1)7 considers all resources available and performs a more appropriate organization than that proposed in the document published in Revista Española de Cardiología.
Organization of the shock code in Catalonia.7 AMI, acute myocardial infarction; VA-ECMO, venoarterial extracorporeal membrane oxygenation.
Thus, in light of the current evidence and the resources, training and staffing levels of the available centers, we propose that “level 2” should include all hospitals with their own infarction code program, irrespective of whether they perform cardiac surgery. This approach is similar to the inclusion of non-heart transplant hospitals with the ability to implant long-term ventricular assist devices in the “level 1” category. This is because “level 2” centers can implant short-term ventricular assist devices and because primary percutaneous coronary intervention is the most effective approach for the treatment of most of these patients. Indeed, these patients can subsequently be transferred to referral centers if required. By making the best use of already available and functioning resources, by acting in a coordinated manner without generating discord among health care professionals, and by putting the patient at the center of the health care system, this approach is the best way to improve the outcomes of a complex condition like cardiogenic shock.
FUNDINGThe authors state that they have not received external funding for the current work.
AUTHORS’ CONTRIBUTIONSThe representatives of centers with an infarction code program but without cardiac surgery endorsing the present document are listed in the appendix.
J. Caballero-Borrego, J. Casanova-Sandoval, J.C. Fernández-Guerrero, A. Frutos-García, A. Gómez-Menchero, J. Jiménez-Mazuecos, I. Lozano Martínez-Luenga, F.J. Molano-Casimiro, R. Ocaranza-Sánchez, N. Ribas-Barquet, J. Robles-Alonso, J.R. Rumoroso-Cuevas, I. Sánchez-Pérez, M. Tellería-Arrieta, A. Torres-Bosco, F. Valencia-Serrano, and B. Vaquerizo-Montilla have contributed equally to the design of this Letter to the Editor, as well as to the literature search, the drafting and revision of the original manuscript, and its final approval.
CONFLICTS OF INTERESTThe authors have no conflicts of interest to declare.
- •
Juan Caballero-Borrego, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario Clínico San Cecilio, Instituto de Investigación Biosanitaria IBS, Granada, Spain.
- •
Juan Casanova-Sandoval, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario Arnau de Vilanova, Lleida, Spain.
- •
Juan Carlos Fernández-Guerrero, Servicio de Cardiología, Hospital Universitario de Jaén, Jaén, Spain.
- •
Araceli Frutos-García, Servicio de Cardiología, Hospital Universitario Sant Joan d’Alacant, Alicante, Spain.
- •
Antonio Gómez-Menchero, Servicio de Cardiología, Hospital Universitario Juan Ramon Jiménez, Huelva, Spain.
- •
Jesús Jiménez-Mazuecos, Servicio de Cardiología, Complejo Hospitalario Universitario de Albacete, Albacete, Spain.
- •
Íñigo Lozano Martínez-Luenga, Servicio de Cardiología, Hospital Universitario de Cabueñes, Gijón, Asturias, Spain.
- •
Francisco Javier Molano-Casimiro, Servicio de Cardiología, Hospital Universitario de Valme (Área Sanitaria Sur de Sevilla), Sevilla, Spain.
- •
Raimundo Ocaranza-Sánchez, Servicio de Cardiología Intervencionista, Hospital Universitario Lucus Augusti, Lugo, Spain.
- •
Núria Ribas-Barquet, Unidad Coronaria, Servicio de Cardiología, Hospital del Mar, Barcelona, Spain; Grupo de Investigación en Enfermedades del Corazón (GREC), Instituto Hospital del Mar de Investigaciones Médicas (IMIM), Barcelona, Spain; Departamento de Medicina y Ciències de la Vida (MELIS), Universitat Pompeu Fabra (UPF), Barcelona, Spain.
- •
Javier Robles-Alonso, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario de Burgos, Burgos, Spain.
- •
José Ramón Rumoroso-Cuevas, Servicio de Cardiología Intervencionista, Hospital Universitario Galdakao, Galdakao, Vizcaya, Spain.
- •
Ignacio Sánchez-Pérez, Servicio de Cardiología, Hospital General Universitario de Ciudad Real, Ciudad Real, Spain.
- •
Miren Tellería-Arrieta, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario Donostia, Donostia, Guipúzcoa, Spain.
- •
Alfonso Torres-Bosco, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario de Álava, Vitoria, Álava, Spain.
- •
Félix Valencia-Serrano, Unidad de Hemodinámica, Servicio de Cardiología, Hospital Universitario Torrecárdenas, Almería, Spain.
- •
Beatriz Vaquerizo-Montilla, Servicio de Cardiología, Grupo de Investigación en Enfermedades del Corazón (GREC), Instituto Hospital del Mar de Investigaciones Médicas (IMIM), Barcelona, Spain; Departamento de Medicina y Ciències de la Vida (MELIS), Universitat Pompeu Fabra (UPF), Barcelona, Spain.