The Cardiology of the Future is a project of the Spanish Society of Cardiology (SEC) whose objectives are as follows: to define the action policies of the SEC; to analyze the trends and changes in the environment that will influence the practice of cardiology in Spain; to define the profile of the cardiologists needed in the future; to propose policies to achieve the objectives resulting from the identified needs; and to identify the role of the SEC in the development and implementation of these policies. This article describes the methodology and the most relevant findings of the final report of this project and the strategic lines to be developed by the SEC in the immediate future, resulting from the analysis performed.
Keywords
The Spanish Society of Cardiology (SEC) is a scientific society whose main objectives are to promote the study, prevention, and treatment of cardiovascular diseases (CVDs) in Spain by supporting training, research, and public education in this field of medicine. However, the objectives of the SEC also include defense of the professional interests of the specialty of cardiology and unified action before any relevant organization (eg, public bodies and other national and international scientific societies) to encourage measures guaranteeing the quality and development of the specialty and the health system. In accordance with these objectives, the SEC has been involved for many years in the presentation and preparation of proposals that aim to improve the organization and management of CVD care within the Spanish National Health System (SNS) and that contribute to its maintenance and quality. In 2007, the SEC published the study The Future of Cardiology,1–3 which was preceded by a study of the resources, needs, and organization of cardiology patient care4; in 2011, it collaborated on the standards and recommendations document of CVD-related health care units.5 Since 2007, the SEC has developed projects that have allowed it to greatly expand our information on the cardiology departments of the SNS6 and has provided indicators7 and quality standards8 that cover a broad spectrum of cardiological activity. In particular, the SEC-RECALCAR project6 has shed considerable light on the resources and activities of Spanish cardiology departments and units and on the health outcomes of the main cardiovascular processes. In addition, RECALCAR has highlighted differences and inequities among the autonomous communities and has promoted changes in their organizational models, as occurred with the Infarction Code program and the heart failure unit networks. The time elapsed since the publication of The Future of Cardiology, the changes in the environment, and the notable increase in evidence on cardiology care have prompted the Executive Committee of the SEC to produce the report El Cardiólogo y la Cardiología del Futuro (Cardiologists and the Cardiology of the Future).9 Its most noteworthy aspects are presented here.
OBJECTIVESThe objectives of this project were to: a) define the perspective of the SEC on current cardiology and its preferred future direction; b) analyze the current situation and trends and environmental changes that will influence the practice of cardiology in Spain; c) define the profile of cardiologists needed in the future; d) propose policies to achieve the objectives derived from the identified needs; and e) define the role to be played by the SEC in the development and implementation of these policies.
The project Cardiologists and the Cardiology of the Future is part of the commitment of the SEC to professionalism,10,11 understood as the basis of the contract between medicine and society.12 Professional ethics compel us to analyze the health care-related needs of society so that we can adapt to them, in accordance with their fundamental principles (ie, prioritization of patient well-being, patient autonomy, and social justice).
METHODSThe Executive Committee of the SEC appointed a project steering committee and 5 subcommittees: Current situation: Public sector; Professional competencies and training; Subspecialties and fellows; Professional recertification; and Cardiologists in the private sector. After the steering committee was formed in January 2018, the work of the different subcommittees began. As a framework for these studies, the report Los servicios de cardiología en el Sistema Nacional de Salud del s. XXI (Cardiology Departments in the National Health System of the 21st Century) was prepared.6 The first version of the final document was approved by the Executive Committee of the SEC in July and became publicly available (on the SEC website) in September 2018. Once the proposals of the members, scientific sections, and affiliated societies were incorporated, the final document was approved by the Executive Committee in October 2018 at the Spanish National Congress of Cardiovascular Diseases.9
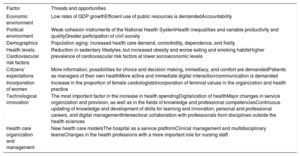
Cardiology departments in the National Health System of the 21st dentury. The trends that will change cardiology in the immediate futureThe report Cardiology Departments in the National Health System of the 21st Century6 analyzed the factors expected to influence the future configuration of cardiology. This article summarizes some of the most relevant aspects of the analysis (Table 1).
Trends changing cardiology in the immediate future
| Factor | Threats and opportunities |
|---|---|
| Economic environment | Low rates of GDP growthEfficient use of public resources is demandedAccountability |
| Political environment | Weak cohesion instruments of the National Health SystemHealth inequalities and variable productivity and qualityGreater participation of civil society |
| Demographics | Population aging: increased health care demand, comorbidity, dependence, and frailty |
| Health levels. Cardiovascular risk factors | Reduction in sedentary lifestyles, but increased obesity and worse eating and smoking habitsHigher prevalence of cardiovascular risk factors at lower socioeconomic levels |
| Citizens’ expectations | More information, possibilities for choice and decision making, immediacy, and comfort are demandedPatients as managers of their own healthMore active and immediate digital interaction/communication is demanded |
| Incorporation of women | Increase in the proportion of female cardiologistsIncorporation of feminist values in the organization and health practice |
| Technological innovation | The most important factor in the increase in health spendingDigitalization of healthMajor changes in service organization and provision, as well as in the fields of knowledge and professional competenciesContinuous updating of knowledge and development of skills for learning and innovation, personal and professional careers, and digital managementIntersectoral collaboration with professionals from disciplines outside the health sciences |
| Health care organization and management | New health care modelsThe hospital as a service platformClinical management and multidisciplinary teamsChanges in the health professions with a more important role for nursing staff |
GDP, gross domestic product.
Expenditure on the publicly-funded health care system as a percentage of gross domestic product (GDP) is one of the lowest in the European Union (6.3% in 2017). It is likely that tensions will increase between the opportunities for health care financing (due to moderate GDP growth in Spain13) and trends in health spending, which is growing in all Organization for Economic Co-operation and Development (OECD) countries at a faster rate than GDP.14 There are basically 2 ways to alleviate this tension: cost control or improved efficiency. Cost control has been the strategy applied in Spain, one of the OECD countries that has made the deepest cuts in health spending.15 While cost control is simple and immediate, the efficiency approach requires wisdom, planning, and involvement of professionals in the management of the system; this is the course of action championed and investigated by the SEC in this project.
Political environmentThe instruments of cohesion of the SNS are weak.16 There are important interterritorial differences in clinical practice in Spain17 and, as shown by RECALCAR, in health service management and health outcomes.18 The differences among health centers are even more marked.19 The limited cohesion of the SNS probably also generates inefficiencies. The principle of social justice embedded in professionalism12 implies a fight against health inequalities produced by organizational and management aspects, clinical practice variabilities, and resource distribution. For Cardiologists and the Cardiology of the Future, the involvement of the SEC in health policy is not just a choice, but an ethical obligation20 in a society that is evolving toward a greater distribution of power,21 and the society should promote greater participation of civil society.22
Aging and demographic changesLife expectancy in Spain has increased more rapidly than in many other OECD countries and is currently the second highest in the world (83.2 years), largely due to decreased cardiovascular mortality.23 Consequently, the patients managed in the health system are increasingly older, with a higher prevalence of comorbidities such as malnutrition24 and dementia, and are frailer.25–28 Hospitalization of these patients can aggravate their vulnerabilities.29,30 Without a change in the health care model, the current attendance rates will probably be maintained, with a notable increase in the number of admissions,31 which may compromise the viability of the SNS. This factor, along with the others reviewed below, has a significant effect on the disease chronification process, which already places a severe strain on the system and requires a change in the current management model, currently focused on managing acute problems.
Cardiovascular risk factorsIn terms of cardiovascular risk factors, lifestyles trends in Spain show a mixture of positive signs (a decline in sedentary lifestyles) and negative signs (increased obesity, worse eating and smoking habits)32; these patterns are worse at lower socioeconomic levels.33,34 A reduction in risk factors, particularly in the most disadvantaged population, would help to decrease overall preventable mortality rates35 and reduce the burden on the health system.
Citizens’ expectationsThe demand for more information, greater opportunities for choice and decision making, improved immediacy, and greater comfort will tend to increase in the immediate future and will be a critical factor for the social legitimization of the health system.36,37 Quality of care standards should be based on patient experience38 and physicians will have to implement communication skills that foster patient involvement.39 Increased patient involvement is one of the strategies to increase the efficiency of health care,40,41 particularly for complex chronic patients such as those with heart failure.42,43 The health system must adapt to the needs of a more informed and associative population. Such individuals will be more involved in the management of their own health and will be more computer literate and demand a more active and immediate digital interaction/communication.
Incorporation of womenOne of the most important social factors is the greater protagonism and involvement of women in the political, social, and economic terrain. In 2017, 66.3% of Spanish medical residents (MIRs) who completed their training were women. Their integration into health care and the wide-ranging impact of feminist values on the system will undoubtedly influence medical practice and its organization.
Technological innovationTechnology is the most important factor behind the increase in health spending in developed Western countries,44,45 and it will likely remain so in the immediate future.46 The reports of the OPTI Foundation indicate the following as relevant aspects for the incorporation and efficient use of technology: flexibility, the establishment of multidisciplinary teams, the retooling of professional skills, and the development of job profiles that reflect and incorporate the technological changes.47–52 However, the SNS does not have a human resource management system based on professional competencies. The working group that prepared the report Cardiology Departments in the National Health System of the 21st Century6 identified a considerable number of technological innovations that will alter the practice of cardiology, from an increase in endovascular procedures to technologies related to the concept of health digitization, and it is very likely that these advances will transform cardiology care in both the immediate future and the next 10 years.
Digitization will have a huge impact on health care, facilitating comprehensive care, promoting precision medicine, establishing new ways to communicate with patients, and increasing system efficiency.53–56 However, digitization also carries certain risks, such as the potential development of insufficiently validated algorithms driven by market interests. An independent agency, with the participation of scientific societies, that certifies predictive models and proposes ways to implement them in clinical practice could address some of these challenges.54,57
Advances in knowledge and technological innovations will produce a profound change in the fields of knowledge and in professional competencies. These advances will necessitate not only a permanent updating of knowledge in the traditional sense, but also training in skills for learning and innovation, for the development of personal and professional careers, and for digital management.58 They will also require a wider intersectoral collaboration with professionals from disciplines outside the health sciences.
Health care organization and managementThe factors that will modify the environment are driving changes in health systems that affect the following:
- •
The health model, particularly its systematic approach to complex chronic patients,40,41,59,60 with greater integration and cooperation between primary and specialized care.61,62
- •
The hospital, which must become a platform within an integrated service network.63
- •
The role of cardiologists, particularly within multidisciplinary teams,64 such as the important role that must be played by clinical cardiologists in these teams. Clinical management65 should actively involve physicians in improving the quality and efficiency of the health system.
- •
The changes in the health professions. These changes refer both to multidisciplinarity and interdisciplinarity and to relationships of complementarity and substitution among health professions.66–68 Quality improvements, technological innovations, and efficiency increases will modify professional barriers.69
- •
The role of nurses. Nursing staff will be more autonomous and will play a larger role in decision making. Specific training and specialization of these professionals will be necessary and will include advanced practice nursing.70,71 Nurses will be key figures in the continuity of care.19
The scientific and health care level of Spanish cardiology is high and is similar to that of other European countries. However, the analysis reveals storm clouds on the horizon.
RECALCAR and health care in SpainRECALCAR19 reports have repeatedly shown that there is wide variability in clinical management and health outcomes among the health services of the autonomous communities, as well as among hospitals and cardiology units, which translate into differences in the quality of care and in the efficient resource use.72 During the RECALCAR study period (2012-2018), considerable progress was made in the implementation of good practices in cardiology units, a trend that is probably not too different from the strategy of continuous quality improvement promoted by the SEC.8 Because RECALCAR provides complete information on cardiology in the SNS, we do not expand further on this aspect here.
Cardiologists in the Spanish National Health SystemBetween 2200 and 2300 cardiologists work in the SNS, equivalent to a rate of 4.8 to 5.0 cardiologists per 100 000 population. Compared with European countries with public health care models of the “national health service” type, Spain is in the lower ranks in terms of cardiologist availability. Of the cardiologists working in the SNS, 63.4% are male; the overall average age is 45.7 years. Increasingly, the SNS contains a higher proportion of female cardiologists (in 2017, 49% of Cardiology MIRs were women), mainly in less complex subspecialties; the trend should be toward a balanced sex ratio in all fields of cardiology.
The salaries of Spanish physicians are among the lowest in the European Union73 and there are notable remuneration differences among the health services of the autonomous communities.74 In addition, 51% of cardiologists have a permanent position in the SNS, 11% have a fixed-term contract, and 38% have an open-ended contract.
The SEC and the European Society of Cardiology have developed certifications for certain subspecialties (eg, arrhythmias and electrophysiology, catheterization and interventional cardiology, imaging, and heart failure). However, these certifications currently lack official recognition in the SNS. Royal Decree 639/2015, which regulates Accreditation Diplomas and Advanced Accreditation Diplomas, empowers the development of subspecialties within cardiology, an approach that should be applied.
Directive 2013/55/EU of the European Parliament and the Council of Europe establishes the obligation to promote the continuous professional development of physicians. Recertification, understood as requirements introduced by scientific societies to ensure that specialist physicians can be considered specialist members throughout the years,75 should be promoted not only to comply with a European directive, but because it is one of the requirements of professionalism.
Private sectorThe private health sector76–78 accounts for 3.4% of Spanish GDP. Health care spending represents 4.3% of household final consumption expenditure, with approximately 20% of this expenditure corresponding to health and accident insurance. A major source of funding for private health insurance comes from agreements with the mutual societies of civil servants.
In recent years, there has been a progressive incorporation of cardiologists who have completed their MIR training into the private sector. The technological investment in this sector has been considerable (private health care has 57% of the magnetic resonance and 49% of the positron emission tomography equipment in Spain), with attention also given to research and training. The growth strategies of these groups for the coming years will be based on an expansion and differentiation of the portfolio of services, reduction in costs, and development and enhancement of marketing actions. The most relevant data of an ad hoc survey of cardiologists conducted by the Working Group of Cardiology in the private sector are the following:
- •
Most are men (71%), younger than 50 years old (52%), and with MIR training (83%) and work experience in public health (87%).
- •
76% work in groups and most (78%) contributed to congresses or had published in the last 5 years.
- •
45% of those who completed the survey worked in hospitals. The technological endowment of these hospitals (eg, advanced cardiac imaging, catheterization) is high.
- •
66% of cardiologists working in the private sector work 10hours per week or more, with a significant proportion of patients with private insurance and a low average number of admissions per visit. In addition, 35% of cardiologists work more than 35hours per week.
- •
The level of satisfaction with private activity is high and the work-family balance was considered to be similar to that in the SNS.
- •
As possible improvements, remuneration was more frequently indicated, as well as formalization of employment contracts (72% are self-employed) and health care and training certification.
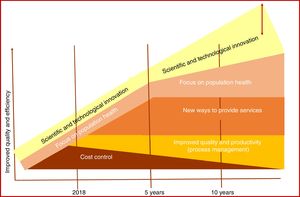
The analysis framework developed by the Health Foundation78 was used to evaluate the impact of different strategies to ensure the sustainability of the SNS (Figure 1). The cutback strategy initiated in 2008 is losing effectiveness and, in the absence of additional resources or structural reforms, will threaten the quality of the SNS. The strategies that are valuable for facing the challenges of the immediate future will require the application of structural measures that promote the establishment of: a) approaches to improve quality and productivity, such as process management, which allow cost control to be maintained without undermining quality, and b) the development of new health care models with a population-based approach to health. Increased knowledge and technological innovation will probably be a vitally important factor for improving efficiency and quality (although the magnitude of the impact cannot be predicted). However, to benefit from its potential, major reforms of the SNS are required, as well as a profound cultural shift.
Analysis of the strategies that can improve the quality and efficiency of the Spanish National Health System. The 2-way arrow in the “innovation” component symbolizes the high degree of uncertainty about its potential impact. Prepared by the authors for the Spanish National Health System, with data adapted with permission from The Health Foundation.82
In summary, structural, functional, and cultural reforms of the SNS are necessary to enable the establishment of new strategies addressing the changing health care needs of society and to improve the quality and efficiency of the system.
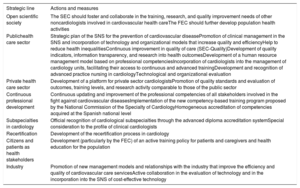
Strategic lines of the Spanish Society of Cardiology for Cardiologists and the Cardiology of the FutureBased on the analysis, the report Cardiologists and the Cardiology of the Future proposes some strategic lines, which are summarized below (Table 2).
Strategic lines of the Spanish Society of Cardiology for Cardiologists and the Cardiology of the Future
| Strategic line | Actions and measures |
|---|---|
| Open scientific society | The SEC should foster and collaborate in the training, research, and quality improvement needs of other noncardiologists involved in cardiovascular health careThe FEC should further develop population health activities |
| Publichealth care sector | Strategic plan of the SNS for the prevention of cardiovascular diseasePromotion of clinical management in the SNS and incorporation of technology and organizational models that increase quality and efficiencyHelp to reduce health inequalitiesContinuous improvement in quality of care (SEC-Quality)Development of quality indicators, information transparency, and research into health outcomesDevelopment of a human resource management model based on professional competenciesIncorporation of cardiologists into the management of cardiology units, facilitating their access to continuous and advanced trainingDevelopment and recognition of advanced practice nursing in cardiologyTechnological and organizational evaluation |
| Private health care sector | Development of a platform for private sector cardiologistsPromotion of quality standards and evaluation of outcomes, training levels, and research activity comparable to those of the public sector |
| Continuous professional development | Continuous updating and improvement of the professional competencies of all stakeholders involved in the fight against cardiovascular diseasesImplementation of the new competency-based training program proposed by the National Commission of the Specialty of CardiologyHomogeneous accreditation of competencies acquired at the Spanish national level |
| Subspecialties in cardiology | Official recognition of cardiological subspecialties through the advanced diploma accreditation systemSpecial consideration to the profile of clinical cardiologists |
| Recertification | Development of the recertification process in cardiology |
| Citizens and patients as health stakeholders | Development (particularly by the FEC) of an active training policy for patients and caregivers and health education for the population |
| Industry | Promotion of new management models and relationships with the industry that improve the efficiency and quality of cardiovascular care servicesActive collaboration in the evaluation of technology and in the incorporation into the SNS of cost-effective technology |
FEC, Spanish Heart Foundation; SEC, Spanish Society of Cardiology; SNS, Spanish National Health System.
- •
The SEC should broaden its focus to include other professionals and establish alliances with scientific societies and professional bodies in order to develop interdisciplinary training, research, and public health activities and improve the quality of all persons involved in cardiovascular health.
- •
The Spanish Heart Foundation (FEC) should further the development of population health activities by establishing alliances with public bodies, civil society entities, and patient associations.
The SEC should strengthen its role in the development of health policy, in collaboration with other scientific societies. Among other relevant topics, the following is proposed:
- •
Prepare a strategic plan for the SNS for CVD prevention.
- •
Develop comprehensive and shared health care models for the management of complex chronic patients.
- •
Promote clinical management in the SNS and the incorporation of technology and organizational models that improve SNS quality and efficiency.
- •
Help to reduce health inequalities.
- •
Continue with the strategy of continuous improvement in the quality of care and patient safety initiated with the SEC-Quality project. One priority in this line of action is information based on real-life data. It is thus imperative to develop mandatory national registries of the activity and outcomes of the most important diseases.
- •
Develop quality indicators of cardiological care performance by promoting information transparency in health service results and research into health outcomes.
- •
Establish a model of human resource management based on professional competencies.
- •
Technological and organizational evaluation.
- •
Incorporation of cardiologists into the governing bodies of the society and into the management of cardiology units to facilitate their access to continuous and advanced training.
- •
The SEC will develop a specific platform for cardiologists working in the private sector to promote their integration and participation.
- •
The fundamental objective of the SEC in this sector should be the promotion and achievement of quality standards and evaluation of results, training levels, and research activity that are comparable to those of the public sector.
- •
The SEC should spearhead the continuous updating and improvement of the professional competencies of all stakeholders involved in the fight against CVD.
- •
The SEC should help to shorten the learning curve in the incorporation of knowledge and innovations that have been shown to cost-effectively improve cardiovascular health.
The new competency-based training program proposed by the SEC through the National Committee of the Specialty of Cardiology should be implemented as soon as possible. The professional competencies acquired should be homogeneously accredited at the national level. This program defines cardiology skills, some of which are new ones related to clinical management and the ability to work in teams, as well as more advanced understanding of the main comorbidities of complex, frail, or dependent heart disease. In addition, there are new competencies overlapping with those of other medical specialties or diagnostic imaging, with the number continually increasing.
Subspecialties in cardiology- •
The SEC proposes official recognition of cardiology subspecialties through the advanced diploma accreditation system. Thus, a national training and curricular program should be prepared for each cardiology subspecialty.
- •
The SEC will promote special consideration to the profile of clinical cardiologists.
The SEC is taking on the challenge of developing the cardiology recertification process as one more component of its commitment to Spanish society and patients with CVD. The recertification requirements (training, care, teaching, and research) should be defined and assessed by the SEC itself and should include a general section and specific headings for each cardiology subspecialty. The final objective needs to be their recognition by the appropriate public body.
The Spanish Society of Cardiology, citizens, and patients as health stakeholdersThe SEC should develop an active policy in relation to educational entities and citizens’ and patients’ associations, as well as in the training of patients and caregivers and the health education of the population.
The Spanish Society of Cardiology and the biomedical industry- •
The SEC will encourage new management models and relationships with the industry that improve the efficiency and quality of cardiovascular care services. Such relationships should be governed by the principles of the defense of ethics, transparency, and independence.
- •
The SEC should actively help to evaluate new technologies and incorporate cost-effective technology into the SNS.
This report on the perspective of the SEC on the current situation of cardiology in the SNS, the predicted changes, and the proposals for its improvement represents another chapter in one of the fundamental strategic lines of the SEC, that of its involvement in the development and maintenance of the Spanish system, vital for supporting the Spanish welfare state. The SEC wants to influence policy and health care management in Spain, based on objective data and independent forecasts and free from any ideological position, with the sole purpose of helping to improve and sustain the SNS. This document identifies and summarizes the master lines that are considered most important and that will be presented in greater detail to the health authorities, other scientific societies, and all bodies of the SEC. We want these measures to not merely be a position paper, but be put into practice. Accordingly, the Executive Committee of the SEC, the project steering committee, and the various subcommittees that have developed each of its paragraphs will continue working to define the priorities, develop the criteria for each proposal, and establish the timetable for their presentation and application.
FUNDINGThe project Cardiologists and the Cardiology of the Future and the creation of this article have been financed through the resources of the SEC.
CONFLICTS OF INTERESTNone declared.
We thank all members of each of the subcommittees and working groups that have generously and selflessly strived to develop this project and draft the document, as well as the staff of the SEC president's office for the important coordination work carried out; the names of those involved can be found at https://secardiologia.es/institucional/reuniones-institucionales/cardiologo-cardiologia-futuro. We also thank the members of the affiliated societies, SEC sections, and members who have contributed to the preparation of the report: Cardiologists and the Cardiology of the Future. A Report of the Spanish Society of Cardiology on the Current Situation and the Challenges of the Specialty in Future Scenarios.