Refractory in-hospital cardiac arrest (RIHCA) refers to an arrest that persists beyond 10minutes of advanced cardiopulmonary resuscitation.1,2 The probability of return of spontaneous circulation drops rapidly after 15minutes, and survival is less than 5%.2,3 Most RIHCAs due to ventricular fibrillation are secondary to heart disease, especially acute coronary syndrome, for which revascularization is essential but normally not possible without return of spontaneous circulation.
In this context, there is a role for venoarterial extracorporeal membrane support oxygenation (VA-ECMO), or “extracorporeal CPR” (E-CPR). In previous series, E-CPR helped reach survival rates of more than 25%.4,5 However, barriers to its use include availability, potential complications, and the need for a team specialized in its implantation and management.
We report here on the experience of our center, in which VA-ECMO was considered in RIHCA with early (< 5minutes) initiation of basic CPR, with the call for ECMO made after 10minutes of advanced life support. The interventional cardiologist implanted the device (Cardiohel) via percutaneous cannulation with fluoroscopy guidance (if implanted in the cardiac catheterization laboratory) and/or ultrasound (transesophageal ultrasound was not used routinely). Implantation was performed at the site of RIHCA occurrence to minimize the time to E-CPR. All cases were attended by 2 clinical cardiologists, 2 catheterization laboratory nurses, and 1 or 2 interventional cardiologists. The priming of the ECMO was managed by the nurses or clinical cardiologists (who had undergone a specific training period). Patients were subsequently transferred to the catheterization laboratory or the coronary care unit.
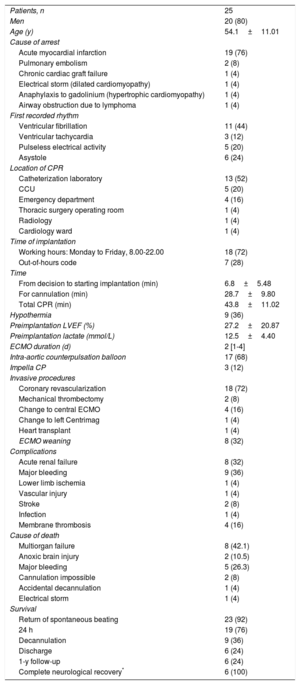
Between November 2013 and October 2018, E-CPR was used in 25 patients. The baseline patient characteristics are shown in Table 1. The mean age was 54.2 years, 80% were men, and 76% of cases were due to acute myocardial infarction. ECMO placement was performed in the catheterization laboratory in 13 patients (52%), in the coronary care unit in 5 (20%), and in the emergency department in 4 (16%). Eighteen patients (72%) were treated during normal working hours and 27 (28%) out of hours. The mean time from arrest to starting VA-ECMO (total CPR time) was 43.8minutes and the mean time required for cannulation was 28.7minutes. ECMO was used to induce hypothermia at 34Cin 9 patients (35%), and in the rest, temperature was controlled at 36°C, according to the clinical judgement of the treating cardiologist, depending on the hemodynamic and electrical instability and the presence of coagulopathy. Cannulation was successful in 23 patients (92%), who had return of spontaneous beating within a few minutes. This allowed treatment to progress to percutaneous coronary revascularization in 18 patients (72%) and percutaneous mechanical thrombectomy in 2 patients with pulmonary thromboembolism (8%). The median time spent on ECMO was 2 (range, 1-10) days; 4 patients subsequently required central VA-ECMO. One of the patients received a successful transplant after E-CPR with peripheral VA-ECMO changed to central VA-ECMO due to left ventricular distension. The leading cause of death was multiorgan failure in 8 patients (32%), followed by major hemorrhage in 5 (20%). Decannulation was possible in 9 patients: 3 with percutaneous closure (33.3%) and 6 with surgical repair (66.6%). Six patients (24%) survived to discharge with good neurological recovery, significantly more in shockable than nonshockable rhythms (38.5% vs 8.3%; P < .001). After 1 year of follow-up, the surviving patients remained stable with no further cardiac events. However, active treatment was limited in 2 patients with irreversible neurological damage, 1 of whom was an organ donor.
Patient characteristics
| Patients, n | 25 |
| Men | 20 (80) |
| Age (y) | 54.1±11.01 |
| Cause of arrest | |
| Acute myocardial infarction | 19 (76) |
| Pulmonary embolism | 2 (8) |
| Chronic cardiac graft failure | 1 (4) |
| Electrical storm (dilated cardiomyopathy) | 1 (4) |
| Anaphylaxis to gadolinium (hypertrophic cardiomyopathy) | 1 (4) |
| Airway obstruction due to lymphoma | 1 (4) |
| First recorded rhythm | |
| Ventricular fibrillation | 11 (44) |
| Ventricular tachycardia | 3 (12) |
| Pulseless electrical activity | 5 (20) |
| Asystole | 6 (24) |
| Location of CPR | |
| Catheterization laboratory | 13 (52) |
| CCU | 5 (20) |
| Emergency department | 4 (16) |
| Thoracic surgery operating room | 1 (4) |
| Radiology | 1 (4) |
| Cardiology ward | 1 (4) |
| Time of implantation | |
| Working hours: Monday to Friday, 8.00-22.00 | 18 (72) |
| Out-of-hours code | 7 (28) |
| Time | |
| From decision to starting implantation (min) | 6.8±5.48 |
| For cannulation (min) | 28.7±9.80 |
| Total CPR (min) | 43.8±11.02 |
| Hypothermia | 9 (36) |
| Preimplantation LVEF (%) | 27.2±20.87 |
| Preimplantation lactate (mmol/L) | 12.5±4.40 |
| ECMO duration (d) | 2 [1-4] |
| Intra-aortic counterpulsation balloon | 17 (68) |
| Impella CP | 3 (12) |
| Invasive procedures | |
| Coronary revascularization | 18 (72) |
| Mechanical thrombectomy | 2 (8) |
| Change to central ECMO | 4 (16) |
| Change to left Centrimag | 1 (4) |
| Heart transplant | 1 (4) |
| ECMO weaning | 8 (32) |
| Complications | |
| Acute renal failure | 8 (32) |
| Major bleeding | 9 (36) |
| Lower limb ischemia | 1 (4) |
| Vascular injury | 1 (4) |
| Stroke | 2 (8) |
| Infection | 1 (4) |
| Membrane thrombosis | 4 (16) |
| Cause of death | |
| Multiorgan failure | 8 (42.1) |
| Anoxic brain injury | 2 (10.5) |
| Major bleeding | 5 (26.3) |
| Cannulation impossible | 2 (8) |
| Accidental decannulation | 1 (4) |
| Electrical storm | 1 (4) |
| Survival | |
| Return of spontaneous beating | 23 (92) |
| 24 h | 19 (76) |
| Decannulation | 9 (36) |
| Discharge | 6 (24) |
| 1-y follow-up | 6 (24) |
| Complete neurological recovery* | 6 (100) |
CCU, coronary care unit; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenator; LVEF, left ventricular ejection fraction.
Unless otherwise indicated, values are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The results of our experience overlap with those found in the literature.4,5 Of note, percutaneous implantation has been demonstrated to be feasible in this situation, with relatively short cannulation times and even better results than surgical implantation.6
In line with previous reports, we observed higher complication rates in cannulation than in elective implantation, the most common being major bleeding at the insertion site (33%), in the context of an emergency implantation in a pulseless patient and with the coagulopathy associated with prolonged CPR.6
In our experience, the use of E-CPR in patients with RIHCA is feasible and appears to improve survival in selected patients, especially those with acute myocardial infarction and shockable rhythms, with substantially worse outcomes in nonshockable rhythms. The success of the treatment is based on the creation of a protocol, with early call for E-CPR and prompt placement at the location where the arrest occurs. We also consider the role of the critical care specialist to be key in the management of VA-ECMO and postarrest care. In our opinion, undergoing VA-ECMO implantation and post-care managed wholly by the cardiology department provides results comparable to those published, with the benefit of the potential expansion to centers with interventional cardiology teams and the organization of a care network for shock and RIHCA.
This study has the limitations inherent to its retrospective nature, small sample size, and lack of control group. However, it is interesting because it is the first series on E-CPR in Spain, and to our knowledge the only one reporting treatment entirely managed by cardiologists.