Multiple deleterious cardiovascular effects produced by coronavirus disease 2019 (COVID-19) have been reported, affecting both the heart and the systemic vascular endothelium.1,2 This is reflected by the frequent and varied cardiovascular manifestations described in the acute phase of the disease.3,4 However, there are limited data on its manifestations in the mid- and long-term.
To analyze the cumulative incidence of major cardiovascular events (MACE) during the first year after hospitalization for COVID-19, we performed a prospective analysis of all patients discharged following COVID-19 hospitalization in a center of excellence between 10 March and May 4, 2020 and followed up until 18 April 2021. Patients were deemed to have COVID-19 on the basis of clinical signs and symptoms compatible with the disease and positive polymerase chain reaction for severe adult respiratory syndrome coronavirus type 2 (SARS-CoV-2).
MACE included acute coronary syndrome, cerebrovascular event, venous thromboembolic disease (VTED), hospitalization for heart failure, and cardiovascular death. Survival analysis was performed with a Kaplan-Meier model followed by Cox regression analysis that included the variables with a heterogeneous distribution between the groups with and without events to analyze the factors associated with events. The study was approved by a research ethics committee, who waived the need to obtain informed consent in light of the ongoing epidemic.
The analysis included 673 patients (53.9% men; mean age, 66.7±15.8 years). The prevalence of cardiovascular risk factors was high: 17.9% were smokers, 30.3% had diabetes, and 20.8% were obese. Among the different comorbidities analyzed, the most prevalent were cardiac comorbidities (23.1%).
The baseline population characteristics and the main details of the COVID-19 hospital admissions are reported in table 1.
Population characteristics
| Whole population (n=673) | Patients without combined event(n=633) | Patients with combined event (n=40) | P | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age, y | 66.7±15.8 | 66.2±15.7 | 75.5±15.0 | <.001 |
| Male sex | 363 (53.9) | 343 (54.2) | 20 (50.0) | .606 |
| Hypertension | 363 (53.9) | 338 (53.4) | 25 (62.5) | .263 |
| Diabetes mellitus | 125 (18.6) | 117 (18.5) | 8 (20.0) | .815 |
| Dyslipidemia | 238 (35.4) | 221 (34.9) | 22 (42.1) | .330 |
| Smoking | 94 (14.0) | 88 (13.9) | 6 (15.0) | .846 |
| Obesity | 99 (14.7) | 94 (14.9) | 5 (12.5) | .681 |
| Ischemic heart disease | 52 (7.7) | 45 (7.1) | 7 (17.5) | .017 |
| Heart failure | 50 (7.4) | 41 (6.5) | 9 (22.5) | <.001 |
| Atrial fibrillation | 54 (8.0) | 46 (7.3) | 8 (20.0) | .004 |
| Cerebrovascular disease | 46 (6.5) | 39 (6.2) | 12 (17.5) | .022 |
| Dementia | 43 (6.4) | 35 (5.5) | 8 (20.0) | <.001 |
| Liver disease | 16 (2.4) | 14 (2.2) | 2 (5.0) | .264 |
| Chronic kidney disease | 54 (8.0) | 47 (7.4) | 7 (17.5) | .023 |
| Renal replacement therapy | 7 (1.1) | 6 (1.0) | 1 (2.5) | .451 |
| Chronic obstructive pulmonary disease | 39 (5.8) | 31 (4.9) | 8 (20.0) | <.001 |
| Asthma | 30 (4.5) | 28 (4.4) | 2 (4.8) | .864 |
| OSAHS | 42 (6.3) | 41 (6.5) | 1 (2.4) | .312 |
| History of cancer | 55 (8.1) | 49 (7.8) | 6 (14.0) | .266 |
| Previous institutionalization | 107 (15.9) | 93 (14.7) | 24 (35.0) | .001 |
| Variables relating to COVID-19 admission | ||||
| Duration of symptoms before admission | .090 | |||
| <7 days | 378 (56.2) | 349 (66.5) | 29 (71.8) | |
| >7 days | 280 (41.6) | 269 (43.5) | 11 (28.2) | |
| Unknown | 15 (2.2) | 15 (2.5) | 0 | |
| CURB-65 score | 0.98±0.9 | 0.88±0.9 | 1.57±0.8 | .003 |
| Radiological pattern | .356 | |||
| No infiltrate | 9 (1.3) | 9 (1.4) | 0 | |
| Unilateral infiltrate | 167 (24.8) | 154 (25.6) | 13 (35.1) | |
| Bilateral infiltrate | 462 (68.6) | 438 (72.8) | 24 (64.9) | |
| Other | 26 (3.8) | 22 (2.2) | 4 (11.7) | |
| ARDS during admission | .024 | |||
| No | 316 (47.4) | 300 (49.1) | 16 (29.1) | |
| Mild | 21 (38.2) | 157 (25.7) | 21 (38.2) | |
| Moderate | 17 (30.9) | 133 (21.8) | 17 (30.9) | |
| Severe | 22 (3.3) | 21 (3.4) | 1 (1.8) | |
| Need for IMV | 16 (2.4) | 14 (2.3) | 2 (3.7) | .522 |
| Acute renal failure during admission | 77 (11.5) | 64 (10.4) | 13 (23.6) | .003 |
| Hospital stay, d | 9.3±6.2 | 9.2±6.1 | 11.1±6.7 | .060 |
ARDS, adult respiratory distress syndrome; CURB-65, score based on the presence of confusion, blood urea level, respiratory rate, blood pressure, and age>65 years; IMV, invasive mechanical ventilation; OSAHS, obstructive sleep apnea/hypopnea syndrome.
Values are expressed as No. (%) or mean±standard deviation.
Most of the patients were symptomatic for at least 1 week before their admission (56.2%), and the most common radiological pattern was bilateral consolidation (72.6%). During hospital stay, most of the patients had some degree of acute dyspnea, although only 2.4% required invasive mechanical ventilation. All patients received some form of treatment for the infection, the most common being hydroxychloroquine (93.3%). The mean hospital stay was 9.3±6.2 days.
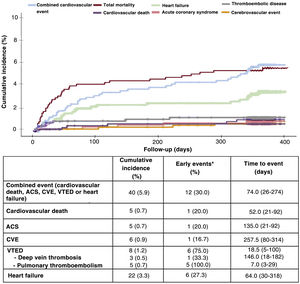
After a follow-up of 352.2±70.4 days, the combined event occurred in 40 patients (5.9%). One third of the events occurred during the first 30 days after hospital discharge, with a median time to first event of 74.0 [range, 26-274] days.
Independently, the most common cardiovascular event during follow-up was hospitalization for heart failure (3.3%), while 0.7% had acute coronary syndrome.
Although most of the events were late (more than 1 month after hospitalization), 75% of the cases of VTED occurred in the first 30 days, with a median time to event of 18.5 [5-100] days. Of note, 62.5% of the cases of VTED were pulmonary thromboembolisms, all of them occurring early after hospitalization, with a median 7.0 [3-29] days until the event.
Thirty-six patients (5.3%) died during follow-up, although cardiovascular mortality was low (0.7%). The events recorded during follow-up are shown in figure 1.
A history of dementia (hazard ratio=3.06, 95% confidence interval, 1.16-8.08; P=.024) and history of chronic obstructive pulmonary disease (hazard ratio=4.11; 95% confidence interval, 1.64-10.30; P=.003) were independently associated with the occurrence of the combined event.
The main finding was the increased incidence of cardiovascular events after hospitalization: 1 in every 16 patients hospitalized for COVID-19 had a MACE in the first year after admission and one third of these occurred during the first 30 days. Admission for heart failure was the most common event after COVID-19 admission, and VTED, particularly pulmonary embolism, was the earliest.
These data further highlight the association between COVID-19 and cardiovascular disease. Although further studies are needed to obtain more detail on the pathophysiological basis for this association, some studies have revealed a high prevalence of structural myocardial damage in the months following the infection.5 In addition, the short time until the onset of VTED is in line with the existing evidence, which has described a high association of venous events in these patients.6 These data lend plausibility to the hypothesis that SARS-CoV-2 acts as a modifying factor of cardiovascular disease, analogous to the interaction of other more studied agents such as the influenza virus. However, more detailed studies on the long-term cardiovascular effect of the virus are needed to allow characterization of the underlying pathophysiological mechanisms.
FUNDINGThe authors declare that they have received no external funding for this study.
AUTHORS’ CONTRIBUTIONSAll authors made a substantial contribution to this manuscript, in terms of writing (M. Negreira-Caamaño; J. Piqueras-Flores), design (M. Negreira-Caamaño; J. Martínez-Del Río; D. Águila-Gordo; C. Mateo-Gómez), execution (M. Negreira-Caamaño; J. Martínez-Del Río; D. Águila-Gordo; C. Mateo-Gómez; M. Soto-Pérez; J. Piqueras-Flores), data collection (M. Negreira-Caamaño; J. Martínez-Del Río; D. Águila-Gordo; C. Mateo-Gómez; M. Soto-Pérez; J. Piqueras-Flores) and data analysis (M. Negreira-Caamaño; J. Martínez-Del Río; D. Águila-Gordo; C. Mateo-Gómez; D. Águila-Gordo).
CONFLICTS OF INTERESTThe authors declare no conflicts of interest in relation to the present study.