"Prevention is better than cure"
Erasmus of Rotterdam, Dutch humanist (1466-1536)
INTRODUCTION
This year, we are devoting our Update section to the subject of cardiovascular prevention. By referencing 8 carefully selected review articles, written by recognized international experts, we offer an in-depth review of the most relevant aspects of this permanently ongoing issue (Table 1). Our aim is to provide a serious, rigorous, and critical update—challenging concepts that do not have an adequate scientific basis—of the beneficial effects of cardiovascular prevention in all its aspects. We review this subject based on information provided by various studies recently published in Revista Española de Cardiología.
PRIMARY VERSUS SECONDARY PREVENTION
In general, we might assume that professionals dedicated to treating cardiovascular disease are reasonably aware of our responsibility to perform the secondary prevention tasks required during follow-up of cardiac patients. However, the data show that this does not always translate into appropriate therapeutic control.1-5 The recent results from the EUROASPIRE-III registry1 indicate that European patients with ischemic heart disease not only have a high prevalence of coronary risk factors, but that the control of these factors is very poor. In Spain, treatment of patients with ischemic heart disease is beginning to meet the evidence-based recommendations of the scientific societies, but is still far from being optimal.2-5 This is a cause of great concern. Some data indicate that a correct control of risk factors after acute myocardial infarction improves long-term clinical outcome6 and that many of these patients can benefit from cardiac rehabilitation programs which, in general, are rarely used.7
However, if all the emphasis is only placed on the relevance of controlling risk factors in secondary prevention then the fact of always arriving too late is implicitly accepted. In fact, and perhaps paradoxically, our involvement in the area of primary prevention is even less, and thus we think it important to emphasize some aspects related to implementing preventive measures in the general population.8-10 Due to its enormous impact on the population, it is reasonable to focus our efforts on preventing the onset of atherosclerotic disease in general, with manifestations in several vascular beds, and of ischemic heart disease in particular. In regard to this disease, no one rejects the idea that prevention is a high-priority strategy. However, as we will see in this update, the actual healthcare situation often calls into question the real efficacy of the measures aimed at guaranteeing the application of such knowledge to clinical practice.8-10
Cardiovascular Prevention
1. Epidemiology. Cardiovascular risk factors
2. Risk prediction algorithms
3. Physical exercise and physical activity guidelines
4. Tobacco use
5. Type of diet. Diets promoting cardiovascular health
6. Diabetes and obesity
7. Comprehensive treatment of risk factors
8. Global policies on cardiovascular disease prevention
SOME REFLECTIONS ON CARDIOVASCULAR RISK FACTORS
Prevention strategies are fundamentally based on the concept that atherosclerotic disease develops silently, slowly progressing from very early ages onwards, and that its first manifestation may be the sudden onset of an irreversible event: death or myocardial infarction.8 From this moment on, all our therapeutic efforts will at best be palliative. We know that risk factors are not only key elements in this entire process, but can also normally be modified and that appropriate control drastically decreases the onset of adverse cardiovascular events.8
Six decades ago, the Framingham studies already established the crucial role played by risk factors in the development of ischemic heart disease.11 In a population of 15 152 patients and 14 820 control subjects recruited in 52 countries, the recent INTERHEART study12 identified modifiable risk factors for myocardial infarction; tobacco use, dyslipidemia, diabetes, hypertension, and obesity were predictors, whereas fruit and vegetable intake, physical activity, and alcohol consumption had a protective effect.12 These factors not only explain more than 90% of the risk of a myocardial infarction, but they also clearly have a cumulative effect. On the other hand, despite their enormous physiopathological relevance, to date, many analytical or genetic parameters associated with inflammation, or vascular thrombogenicity have not demonstrated their usefulness in improving the predictive capacity offered by studying the classic risk factors and, thus, have not been incorporated into clinical practice.13 Something similar occurs in relation to the so-called emerging risk factors.
Roughly but graphically speaking, we can say that less than half the individuals presenting some risk factor know their diagnosis, that less than half of them receive specific treatment and, in turn, less than half of those treated fulfill the therapeutic aims recommended by the clinical practice guidelines.8-10,14-16 Thus, we very clearly still have a long way to go. Furthermore, recent studies in Spanish children and adolescents have highlighted the high prevalence of risk factors, such as hypercholesterolemia, sedentary lifestyle, and obesity.17-21
Some longitudinal studies conducted in postgraduates also show that as they age many of these factors become worse.22-26 Neither are the data obtained from large studies in Spanish workers very encouraging.27,28 Finally, age distribution is being significantly affected by the demographic changes occurring in the population and should be taken into account when making predictions, since the prevalence of a sedentary lifestyle, obesity, hypertension, hypercholesterolemia, and diabetes significantly increases with age.8-10,25 Although there has been an obvious reduction in blood pressure and cholesterol figures in developed countries, the prevalence of obesity and diabetes continues to increase.8-10,25
The treatment of some classic risk factors, such as hypertension and hypercholesterolemia, will be addressed in specific sections in this update (Table 1). It is worth recalling that any increase in blood pressure figures, even within what is considered to be the normal range, is associated with greater morbidity and mortality.8,9 In a cohort of Spanish university graduates, the incidence of hypertension was relatively high and the cumulative probability of a medical diagnosis of hypertension at 65 years was 50% in women and 70% in men.26 We have already pointed out that blood pressure control is normally poor in clinical practice.14-16 In this context, our therapeutic effort basically depends on the severity of hypertension and to what degree the target organs are affected.8,9 We are also well aware of the importance of controlling cholesterol levels both in primary and secondary prevention. Once again, several studies have shown that in clinical practice many patients do not fulfill the recommended lipid levels .8,14-16 This is especially striking taking into account that there are effective, safe, and powerful hypolipidemic agents within our current available therapeutic arsenal, and that there is overwhelming evidence on the beneficial effects of statins, both in patients with hyperlipidemias and those with coronary heart disease.8 One of the most spectacular therapeutic effects—due to its mechanism of action— is the recently demonstrated capacity of aggressive hypolipidemic treatment (high-dose statins) to inhibit the increase—and even reverse—atherosclerotic plaque volume in a surprisingly short time.29,30 Finally, the adverse effects of tobacco use are unquestionable; we also devote a complete section to analyzing the consequences of this habit, as well as measures aimed at its elimination (Table 1).
A sedentary lifestyle is one of the most relevant preventable causes of death and an inverse linear relationship has in fact been demonstrated between the quantity of physical activity carried out and mortality from any cause.31 Specifically, regular physical activity decreases the risk of cardiovascular disease and various risk factors.31 During the last decade, the relevance of the benefits obtained by children, adolescents, and the elderly engaging in sport has been demonstrated. Recent recommendations indicate that men should engage in at least moderate physical activity for at least 30 min daily and children should do the same for 1 h, preferably every day.31 In Spain, recent data17 have indicated that 41% of Spanish adolescents should be regarded as physically inactive, that female adolescents form the greatest proportion of the physically inactive population, and that there is a clear trend toward this situation becoming worse.17,18 Thus, it is extremely important to promote physical activity programs during childhood and adolescence, and lifestyles that prevent obesity.31 The increasingly sedentary lifestyle found in the population seems to be involved in the current obesity pandemic and in the increase in metabolic syndrome.31
The increasing prevalence of overweight and obesity will lead to an increase in type 2 diabetes mellitus with its known association with cardiovascular complications.8,9 The relevance of abdominal obesity, and thus anthropometric measurements such as waist circumference, as well as body mass index, has been clearly demonstrated.32 We know that cardiovascular risk is practically double in patients with metabolic syndrome and some studies indicate that patients who accrue a greater number of metabolic risk factors have a particularly adverse prognosis.33 In turn, diabetes is also acquiring epidemic proportions. This affects us closely, since two-thirds of diabetic patients die of cardiovascular disorders. A recent systematic review confirmed that type 2 diabetes mellitus has a similar cardiovascular risk as the presence of coronary heart disease, particularly in women.34 We cannot overemphasize the importance of strict control of risk factors in diabetic patients and especially in diabetic women.9 The duration of diabetes progression and the presence or absence of microalbuminuria should also be taken into account.8,9,33 Although we note that there are new and promising pharmacological measures against obesity, diabetes, and smoking, it is clear that the emphasis should focus on the prevention of all these factors and the promotion of lifestyles which benefit cardiovascular health.8-10
NEW CLINICAL PRACTICE GUIDELINES
The multifactorial involvement of all risk factors explains why the clinical practice prevention guidelines were developed from the very beginning by several scientific societies in collaboration and embracing different medical specialties. This has obviously contributed to the multidisciplinary character of the guidelines and the final consensus has made it possible to design campaigns and unified action strategies, capable of having a greater impact on the population.8 The involvement of nursing personnel in these campaigns is vital. Several clinical practice guidelines on cardiovascular prevention have recently been released on hypertension, diabetes, and prevention.8-10,31 These have been translated and discussed in our Journal to facilitate their dissemination and implementation.
The current cardiovascular prevention guidelines8 point out that, before searching for levels of evidence and grades of recommendation, we should recall that, in the area of prevention, pharmacological studies are much more suited to randomized designs, and thus may gain unjustified prominence at the expense of general recommendations on changes in diet and lifestyle, which are more difficult to analyze in studies with this type of design. In other words, in the context of cardiovascular prevention, not all high-quality evidence should necessarily lead to strong recommendations.8 Currently, we have moved from talking about coronary heart disease prevention to cardiovascular prevention in general,8-10 emphasizing atherosclerosis as a systemic progressive disease. On the other hand, it should be borne in mind that interaction between risk factors is very strong and that the risk due to simultaneous exposure to several factors is much higher than the result of simply adding the factors together.8-10
Our perception of risk factors has recently undergone changes.8 First, although classic dichotomous criteria have proven very useful from the diagnostic standpoint, their value has been widely questioned and we currently have sufficient epidemiological evidence showing that it is better to analyze these factors using continuous criteria. Second, the approach to therapeutic recommendations has also changed due to atherosclerosis being considered a multifactorial disease. Thus, when estimating individual cardiovascular risk, we should assess all the risk factors in combination to design an overall therapeutic approach. Thus, therapeutic aims should be modified in relation to a given risk factor (we should be more aggressive) if other risk factors are present. We have also learned that these factors are closely interrelated and that adopting several therapeutic approaches would enable their simultaneous modification in the desired direction, thus reduce total cardiovascular risk. For this reason, attempting to establish the real effect of modifying just one of them could prove futile. Finally, it is important to emphasize that preventive measures should not convert previously healthy people into patients.8-10
The new diabetes guidelines9 also stress the need to intensify general measures (pharmacological or otherwise) to reduce total cardiovascular risk, with therapeutic intent, while reserving specific cardiology tests for highly selected patients. The initial therapeutic strategy in type 2 diabetes mellitus patients, in addition to lifestyle changes, includes treatment with metformin. In Spain,14 just 40% of diabetic patients with ischemic heart disease present HbA1c levels less than 7% and the degree of control over the remaining risk factors is far from that recommended.9
The new hypertension guidelines10 emphasize the importance of effective blood pressure control (independently of drug selected) and also encourage the use of drug combinations to guarantee achieving the therapeutic targets. These guidelines differentiate normal blood pressure from normal-high blood pressure, but do not recognize the concept of prehypertension.10 They also highlight the importance of early intervention in case of organic injury or additional risk factors. The MESYAS registry27 indicated that 30% of hypertensive patients presented metabolic syndrome, but prevalence increased up to 54% when hypertension and obesity were both present.
In general, the guidelines recommend estimating an individual's total risk as a necessary tool to achieve efficient interventions.8-10 However, risk estimations have a very low predictive value, since most people who undergo cardiovascular events are not labeled as high-risk. In this sense, it appears that techniques that enable the identification of patients with subclinical atherosclerosis could be of help. Thus, the ankle-brachial index is an easily available, simple, reproducible, and inexpensive test, which is particularly useful for detecting silent atherosclerosis and identifying high-risk cardiovascular patients.35,36 In addition, modern noninvasive imaging techniques help us to directly visualize atherosclerotic disease in different vascular beds. Finally, the recent technological revolution in cardiac imaging techniques (multislice spiral computed tomography and magnetic resonance imaging) has enabled the noninvasive visualization of coronary lesions.37-39 The high negative predictive value of these techniques makes them, in principle, very attractive for screening selected populations, although their real value to clinical decision algorithms is still pending confirmation.37-39 The SHAPE40 study prospectively analyzed the incremental value of these diagnostic techniques in predicting total cardiovascular risk.
WHICH RISK FUNCTION SHOULD WE USE?
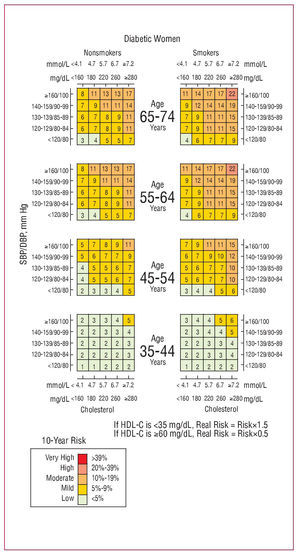
Risk scales are a very useful tool in cardiovascular prevention decision-making, but should always be analyzed in the context of a comprehensive clinical assessment of the patient.41-49 Cardiovascular risk should be estimated by age and sex and should ideally be based on following up sufficiently large population cohorts to obtain high accuracy. The classic Framingham study, whose results remain highly relevant,11 provides equations that enable estimating the 10-year risk of suffering a coronary episode (fatal or nonfatal). In lower-risk populations, this scale should be calibrated and adjusted —using validated methodologies—for the reference parameters. In recent years, our Journal has helped to promote the passionate debate surrounding this subject.41-49 The Framingham scale overestimates risk in southern European countries; nevertheless, this scale has already been calibrated in the population of Gerona, Spain (REGICOR),41 and thus can be used with confidence in our country (Figure 1). Recently, the accuracy and validity of this adaptation have been confirmed in Spain (VERIFICA study).48 The SCORE (Systematic COronary Risk Evaluation) function42 is also another valuable tool that was developed in Europe to calculate total cardiovascular risk. This enables determining the 10-year risk of cardiovascular death (high risk >5%) and is based on simple and easy-to-obtain parameters (age, sex, tobacco consumption, total cholesterol, and systolic blood pressure). Based on this model, some user-friendly charts have been developed for high-risk European countries (northern Europe) and low-risk ones, such as Spain.42 More recently, the SCORE model has also been specifically calibrated for Spain47 (Figure 2). Its use leads to slightly higher risk estimates than those found using the SCORE general function for low-risk countries. The fact that diabetes—a determining factor in cardiovascular disease progression in such patients—is not incorporated in the main decision algorithm remains a source of surprise. In fact, these charts are not suitable to assess risk in diabetic patients, those with known vascular disease, or with a severe risk factor, all of whom are automatically considered high-risk patents.46-49 It has been suggested that other scales may be more accurate in these patient subgroups, and in patients more than 65 years old.49
Figure 1. Estimation of coronary risk using the Framingham equation calibrated for Spain. Chart for diabetic women. Adapted from Marrugat et al.41
Figure 2. The SCORE cardiovascular risk chart for men calibrated for Spain. Adapted from Sans et al.47
Efforts to calibrate these screening instruments are important, since the equation used should ideally take into account the epidemiological situation of the population to which it is applied.41-49 Regardless of the model chosen, the mentioned functions enable estimating risk at the population scale, but involve a high degree of uncertainty when assessing the individual patient. Furthermore, in young people with a relative high risk of complications for their age—but with low absolute risk—and in elderly people, who are always at high risk, the advisability of prescribing aggressive treatment should be evaluated very carefully. In particular, patients who are candidate to receive hypolipidemic and antihypertensive treatment, which is normally for life, should be selected with great care.
The phenomenon of most community deaths specifically occurring in the lowest-risk population (being the most numerous), is known as the Rose paradox.50 This phenomenon shows that, although pharmacological treatment produces more benefit in higher-risk patients, general hygiene-dietary measures, due to affecting the entire population, have a greater impact on the social and economic burden attributed to cardiovascular diseases.
HOW CAN WE DEVELOP HEALTH STRATEGIES AT THE POPULATION SCALE?
The cardiovascular disease epidemic is a serious public health problem in Spain whose spread can only be checked by implementing suitable preventive measures. In light of the above, we should be prepared to challenge the great inertia and conformism that leads to overfocussing on secondary prevention, while disregarding key strategies for reducing risk exposure in the community as a whole. Urgent and necessary multilevel interventions must be adopted to promote and maintain more active and healthier habits in the entire population. Strategies aimed at promoting a lifestyle that enhances cardiovascular health rest on 5 basic pillars: developing, disseminating, adopting, implementing, and finally, maintaining such programs. The beneficial effects of these strategies have already been confirmed in different countries and public health models.8-10 Thus, we should be able to make society aware of the importance of developing lifestyles which promote cardiovascular health. In Spain, interesting results have been obtained by assessing the effect of maintaining a Mediterranean diet.51 A change in mentality, beginning with the family and school, should lead to a healthy and active working population. These words should also reach out to different legislators to make them aware of their responsibility to promote policies aimed at developing and implementing the guidelines of the scientific societies, in a coordinated and ongoing manner. Some initiatives, such as the legal duty to describe not only the number of calories, but also the composition and type of fats in food offered by commercial enterprises, and more recently, even in restaurants, seem to be a step in the right direction. In Spain, the restricted-smoking law and, recently, the measures against child obesity, approved unanimously by the Senate, have created a certain optimism. Finally, we should continue to promote new research studies, since the efficacy of the current preventive strategies is still limited.
CONCLUSIONS
As this update has shown, it is clear that the cardiologist should play a key role in not only secondary prevention strategies but also primary prevention strategies. We cannot go on accepting always arriving too late. We hope that, as in previous years,52,53 reading this new Update in Revista Española de Cardiología will help us to both update ourselves on this burning issue and increase awareness of our responsibilities in relation to cardiovascular prevention. As all physicians dedicated to treating patients with cardiovascular diseases are well aware, despite current and impressive diagnostic, and therapeutic progress, prevention continues to be far better than cure.
Correspondence:
Revista Española de Cardiología. Sociedad Española de Cardiología.
Nuestra Señora de Guadalupe, 5-7. 28028 Madrid. España.
E-mail: rec@revespcardiol.org