Keywords
"Research into illness has progressed so much that it is almost impossible to find someone who is completely healthy"
Aldous Huxley
The primary prevention of cardiovascular disease (CVD) focuses on controlling risk factors, that is, elements associated with the incidence of and mortality from these diseases.1-4 The best tool to establish priorities in cardiovascular primary prevention is to accurately estimate the risk of developing them.5,6
In recent years, the debate in Europe and Spain on the role of cardiovascular risk functions has been intense and the topic has included a stimulating range of issues while at times the discussion has been stormy.7-17 The range of this debate is indicted by the sheer amount of arguments offered; stimulating, because of the involvement of many medical sectors that often remain silent; and turbulent, due to some misunderstandings caused by the complexity of the problem that have emerged during this process. Most professionals have maintained a prudent silence while waiting for more clarity, conciseness and, obviously, scientific support in the expert recommendations.
The aim of this review is to determine the usefulness and limitations of the different functions available for estimating cardiovascular risk in Spain, and to analyze possible new strategies on population screening for CVD risk.
CARDIOVASCULAR RISK ESTIMATION IN PRIMARY PREVENTION
Risk Functions Available in Spain
Risk charts are simplified estimation methods based on mathematical functions that model risk in individuals in different population cohorts followed up, in general, for 10 years.18 These functions make it possible to estimate excess risk in individuals compared to the average of the population to which they belong. That is, based on the information on the prevalence of cardiovascular risk factors in a representative sample of the population, a mathematical algorithm makes it possible to obtain the percentage of participants with each combination of factors who will develop an event at 10 years. This estimation, made at the individual scale, supports decision-making, and facilitates prioritizing preventive action. The design process demands that the data used to model the functions are representative of the population whose risk is going to be estimated.19
The first version of the Framingham risk function18 was published in 1990 and the second20 in 1998. The authors established a calibration method for its adaptation to different populations; the main requirement was to have data available on the prevalence of cardiovascular risk factors and the incidence of events in such a population.19 The constant overestimation of risk observed when using the original function in different countries, including Spain,21-26 led the REGICOR (Registre Gironí del Cor [Gerona Heart Registry])27,28 researchers to adapt this tool to the Spanish population in 2003. The result was a function that can correctly predict the coronary event rate at 5 years in the Spanish population aged 35-74 years,29 in contrast to the original function.26,30
The SCORE (Systematic Coronary Risk Evaluation) project developed a risk function based on following up 200 000 people in 12 cohorts from 11 European countries over 10 years. The risk tables based on the new function were published in 2003.31 This function has a special formula for low-incidence countries that has already been applied in Spain.32 The baseline risk in low-incidence and Banegas et al.39 countries was obtained mainly from Belgium and Italy, where risk is approximately 30% higher than in Spain.33,34
Table 1 provides a comparative summary of the characteristics of the main functions available in Spain.35 The Framingham function and the calibrated REGICOR function make it possible to estimate the risk of coronary morbidity and mortality in subjects aged 35 to 74 years and to differentiate diabetic patients from nondiabetic patients.20,29 The SCORE function estimates the combined risk of coronary mortality, cerebrovascular mortality, heart failure, peripheral artery disease, and other diseases such as dissecting aortic aneurysm in subjects aged 40 to 65 years, but does not differentiate between diabetic and nondiabetic patients.31,32
Risk Estimation Based on Classic Risk Factors
The starting point for constructing the Framingham functions was the estimation of the risk attributable to risk factors in the development of ischemic heart disease (IHD) in this population.18,20 As age, sex, lipid profile, blood pressure, glucose intolerance, smoking, and left ventricular hypertrophy have a demonstrated association with IHD, hypertension, and left ventricular hypertrophy play a predominant role in stroke. In turn, smoking, glucose intolerance, and left ventricular hypertrophy would be the risk factors predictive of peripheral artery disease.36 On the other hand, attributable risk also varies between geographical areas. Thus, whereas dyslipidemia was found to be the most relevant risk factor in the development of IHD in the USA,18,20,36,37 in Spain obesity and particularly smoking among men could have a greater population impact (Figure 1).38,39
Figure 1. Population attributable risk for ischemic heart disease (IHD) and stroke for the 5 classic cardiovascular risk factors in Spain. Adapted from Medrano et al38
South European Mediterranean countries have demonstrated a high prevalence of classic cardiovascular risk factors together with an unexpectedly low incidence of stroke.40,41 This observation, known as the "south European paradox," indicates that the analysis of classic cardiovascular risk factors would explain only a part of cardiovascular risk but may not take into account the contribution of possible protective factors.
Analysis of the VERIFICA (Validez de la Ecuación de Riesgo Individual de Framingham de Incidentes Coronarios Adaptada [Validity of the Adapted Individual Framingham Risk Function for Coronary Events]) study cohort showed that the low concentration of high-density lipoprotein cholesterol (HDL-C) was the only difference in lipid profile between the 180 individuals who underwent a cardiovascular event in contrast to the 5552 individuals who were event-free at 5-year follow-up.29 In fact, various cohort and clinical trial studies have conducted in-depth analyses of the role of HDL-C as a protective factor.42,43 Its predictive capacity was analyzed in the context of the Framingham study, which concluded that the total cholesterol/HDL-C ratio was the best lipid measurement for predicting atherosclerosis.44,45 Despite this, during the process of designing the function, the results were not very different if this ratio was included or just the HDL-C concentrations alone. For this reason, the 1998 version—and the REGICOR function derived from it— include HDL-C as a risk factor modifier.20,28 The SCORE function, however, does not include information related to HDL-C concentrations, since, during the design phase, the researchers found no differences in risk estimation if the total cholesterol/HDL-C ratio was included or just the low-density lipoprotein cholesterol (LDL-C) concentrations alone.31,32
Validation of Risk Functions
The validation of risk prediction instruments is of great importance given that risk estimation is considered the best tool to set priorities in primary prevention.5,6 The validation method of a cardiovascular risk function involves having a cohort available from which the following characteristics can be assessed with sufficient statistical power:
- Accuracy: the number of events predicted in a population are compared to those observed at follow-up. To this end a goodness-of-fit test is performed by estimating the event rate using a Cox proportional hazards function for each sex, with its corresponding confidence interval, in a minimum of 3 risk groups
- Reliability: establishes the capacity for classifying individuals in the cohort in relation to whether an event will or will not occur in the period under study. This involves comparing the area under the receiver-operating characteristic (ROC) curve of the original function to the one obtained from the cohort study data used for the validation process with the Cox proportional hazards model obtained19,29
An initial aim of the VERIFICA study was to assess the accuracy and reliability of the 3 risk functions in Spain. Thus, 2 cohorts were recruited. One was studied retrospectively and was representative of the population served by primary care centers in Spain including a total of 4427 participants; the other was studied prospectively and was representative of the population of Gerona (Spain), including a total of 1305 participants, none of whom had IHD. The sample covered a very wide range of risks, which is a requirement when validating a risk function. Follow-up was performed at 5 years and all symptomatic coronary events were taken into account.46 However, almost half the cardiovascular events in the cohort recruited for this study occurred in individuals aged between 65 and 74 years, as occurs at the population scale.47 The statistical power was not sufficient to validate the SCORE function, which only predicts mortality in individuals aged between 45 and 64 years.31,32
The study concluded that the risk function adapted for the Spanish population based on the original Framingham function was valid, that is, accurate and reliable, at time of predicting coronary events at 5 years in a population aged between 35 and 74 years.29 To date, no study has validated the SCORE function for its use in the Spanish population. However, its validity and the results obtained from its use have been assessed in other countries, and a degree of agreement has been observed between different studies regarding the fact that the function does not achieve the level of accuracy required.48-52
Risk Function Performance: Sensitivity and Specificity
Risk functions are instruments designed to estimate risk in a population that shares certain risk factor characteristics, sex and age, which involves a high degree of uncertainty when applied at the individual level.53
The VERIFICA study was the first to analyze the operational performance of the risk functions available in Spain.54 In high-incidence countries, where these types of studies have already been conducted, the sensitivity of the functions is around 40%.55 These figures would be unacceptable for a diagnostic test; however, the importance of this is relatively less for a screening test intended to structure primary prevention for cardiovascular disease. However, well-established screening tests, such as that for breast cancer (focusing on disease detection as well as the risk of contracting it) have a sensitivity of around 60% in women aged 45-69 years.56
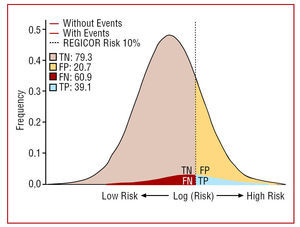
Achieving 100% sensitivity in detecting the group of people who will develop a cardiovascular event at 10 years would involve treating the entire population (Figure 2), and even so it would be impossible to prevent all events, since preventive methods are of limited efficacy.53 The results of the VERIFICA study showed that, given the observed incidence of events, each 1-unit increase in sensitivity would be equivalent to identifying 1.8 individuals who will undergo some coronary event, and each 1-unit increase in specificity would identify 55 individuals who will not undergo such an event.54 This information should make it possible to determine how much effort to put into preventive measures taking into account that the balance between sensitivity and specificity is defined by the threshold established to guide action. This threshold is completely arbitrary, although it is accepted that the corresponding risk is close (a fraction) to that in patients who have already presented a cardiovascular event. When choosing this threshold, the specificity of the test is the most relevant factor, as the decision to treat has a greater impact on the number of those treated unnecessarily (false positives) than on the number of those treated correctly (true positives) (Figure 2).53
Figure 2. Distribution of the results of the risk logarithm in the participants who developed ischemic heart disease and those who remained disease-free at 5-year follow-up in the VERIFICA study. FN indicates false negative; FP, false positive; TN, true negative; TP, true positive. Adapted from Marrugat et al.53
Risk Estimation and the South European Paradox
Societies in industrialized countries are undergoing a gradual aging process that is leading to an increase in average cardiovascular risk in this population, as the disease predominantly affects people aged more than 55 years.57 In 2005, life expectancy in Spain was over 77 years in men and 84 in women, with an upward secular trend.58 In epidemiological terms, this fact has led to a decrease in mortality in age-standardized CVD, even though the crude death rate from this cause continues to increase.59 In Spain, IHD was the leading individual cause of death in men (10.9%) and the second in women (9.2%)60 in 2005; furthermore, almost half of the incident coronary events, and two-thirds of mortality from this cause occur at ages above 65 years.47 The myocardial infarction incidence rates (AMI) in Spain between 1997 and 1998 were 207/100 000 (men) and 45/100 000 (women), that is, approximately 70% of morbidity and mortality due to IHD, according to the IBERICA (Investigación, Búsqueda Específica y Registro de Isquemia Cardiaca Aguda [Research, Specific Search, and Acute Cardiac Ischemia Registry]) study in 6 regional communities.61 These figures have remained stable in Spain during the 1990s and have been accompanied by a significant decrease in hospital case-fatality.47 The final outcome is an increase in the number of AMI survivors and, thus, an increase in the number of individuals with IHD.57 However, the incidence in Spain is between one-half and one-fourth that found in north, east, and west European countries, the USA, and other English-speaking countries, even though the prevalence of risk factors in the Spanish population is similar to these. This phenomenon is known as the "south European paradox."40,41
In Spain, the age-standardized mortality rate of stroke in people older than 24 years was 58 and 43 per 100 000 in men and women, respectively. In the last 30 years, the decrease in the stroke rate has been faster than that of IHD. The cumulative incidence rate has been estimated at 218 per 100 000 men and 127 per 100 000 women. Similar to IHD rates, these are among the lowest figures currently found in developed countries.62
The size of the CVD problem in Spain indicates that the ideal risk function would be one constructed based on data from a Spanish population cohort, with a sample size large enough to estimate probabilities with accurate ranges, capable of calculating the risk of morbidity, and mortality due to IHD and stroke separately, and applicable to diabetic patients separately, including all the variables relevant to Spain. It would also include people aged up to 74 years, especially to estimate risk in women, as their life expectancy is longer.
Thus, it seems justified to create a cohort of suitable size such that a sufficient number of cardiovascular events occur within 5 and 10 years to enable estimating the coefficients of each risk factor. Given that the Framingham function needed around 5000 people, at least double this figure would be necessary in Spain, as the incidence is less than half that in the USA.47,61
The establishment of a risk function for the prediction of CVD that is more accurate, valid and applicable to Spain will increase the scientific basis for decision-making related to the primary prevention of CVD. At present, and with this aim, a study is underway that will definitely provide a better reflection of the situation in Spain.63 However, until new evidence is available, we should base our decisions on using the most accurate tools available.
USEFULNESS OF RISK FUNCTIONS IN PRESCRIBING PHARMACOLOGICAL TREATMENT
Estimation of Cardiovascular Risk and Dyslipidemia
Risk estimation is a key factor when deciding to begin pharmacological treatment for dyslipidemia.5,6
Hypolipidemic therapy seems to be effective only in the primary prevention of combined coronary events,64-66 but no proof is available showing that it is able to reduce peripheral vascular events or stroke in primary prevention.67,68 The results of a recent clinical trial have even shown that secondary prevention with hypolipidemic therapy does not decrease fatal stroke.69 Thus, current treatment recommendations on the use of statins for stroke prevention exclude patients without a history of atherosclerotic disease in any of its manifestations,70 even though some authors have suggested the existence of a reduction in mortality based on a metaanalysis which included primary and secondary prevention studies.71,72
The use of risk functions to predict cardiovascular events in different countries may translate into overprescribing treatment for dyslipidemia.73
When making decisions on pharmacological hypolipidemic therapy, it is also important to take into account individual factors, which are not included in the actual function. The convention by which individuals at a high level of risk according to the Framingham function (greater than 20% at 10 years) receive this type of treatment has been formed by consensus. According to the NCEPIII (National Cholesterol Education Program) guidelines, it is not cost-effective to treat individuals with a risk lower than 10%.6 The problem is apparent when we assess the management of individuals in the intermediate risk band (10%-20%) to decide at which point they should receive treatment. According to several clinical trials in primary prevention,64-66,74-77 treating populations with an IHD risk 316% is effective, whereas there is no proof that in individuals with a coronary risk less than 13% the benefits of statins counterbalance their potential adverse effects on mortality at 10 years.78,79 Even so, when setting therapy thresholds we should take into account that the main clinical trials on the primary prevention of IHD were conducted in high-incidence countries,64-66,74,75 except for the MEGA (Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese) study, which was conducted in Japan, a low-incidence country.76 The reduction in absolute risk in Spain was much smaller than in other countries, even though blood lipid levels were greater in the individuals enrolled. At the population scale, this fact involves greater clinical benefit and economic advantages when reducing the risk of IHD in high-incidence countries (Table 2).35
The adaptation of prevention strategies is achieved by adopting realistic and feasible aims. Strategies aimed at reducing low-density lipoprotein cholesterol (LDLC) attempt to move its distribution toward the left of the population scale, thus obtaining a reduction in total risk.4 The most recent European guidelines suggest achieving LDL-C concentrations of 115 mg/dL in healthy individuals and 100 mg/dL in high-risk individuals.5 Data for the year 2005 show that 50% of the population of Gerona presented LDL-C concentrations of 130 mg/dL.80 Taking into account that this was a low-incidence population,47,61 a reasonable aim in this situation could be to achieve concentrations of <130 mg/dL in high-risk individuals and <150 mg/dL for the rest of the population.
Estimating Cardiovascular Risk and Hypertension
The clinical practice guidelines recommend treating hypertension in primary prevention based on the actual blood pressure value, the presence of target-organ lesions, and the coexistence of other risk factors.81,82 In prehypertension or normal-high pressure, the decision to begin treatment is based, among other things, on the presence of other risk factors, and it is likely that in this situation the estimation of combined cardiovascular risk could prove useful regarding decisions on pharmacological therapy.
Estimation of Cardiovascular Risk and Diabetes Mellitus
One of the characteristics of patients with type 2 diabetes mellitus is their greater risk of morbidity and mortality due to CVD.83-85 Generally, the relative risk of a diabetic patient of suffering some of the forms of CVD is 1.8 versus 3.3 in non-diabetic men and women, respectively.83
Two studies conducted in Finland concluded that diabetic patients, due to their high risk of undergoing an event, could be considered and treated as cardiovascular patients, even before the disease manifests.86,87 However, other authors suggest that coronary risk in diabetic patients without IHD is about half that of non-diabetic patients with IHD.88-92 Lee et al attribute the differences between the studies to a sample selection problem, among other reasons.89 The studies that suggested there was a similar risk between diabetic patients without a CVD background and non-diabetic patients with a CVD background excluded diabetics who were only being treated via diet and had undergone a first coronary event, whereas they included individuals with a background of stroke, cancer, or coronary revascularization.91,92
A study conducted on the population of 6 counties in Gerona, showed a prevalence of age-standardized diabetes of 10% and abnormal basal glycemia values of 7.6% in individuals aged 25 to 74 years, according to the criteria of the American Diabetes Association of 1997.93 The demographic characteristics and lifestyle changes suggest that there will be a strong increase in prevalence in the near future. The socioeconomic cost of treating all diabetic patients as coronary patients leads to the need for greater accuracy when making recommendations. Thus, the CARDS (Collaborative Atorvastatin Diabetes Study) clinical trial (Table 2) on primary prevention with statins, concluded that the subgroup of diabetic patients with low LDL-C concentrations warrant this type of treatment.77
The results of the VERIFICA study showed that the function adapted from the REGICOR study very accurately estimated the coronary event rate at 5 years in these patients.29 Although these patients were included in the cohort used to create the SCORE function, it cannot identify them when estimating risk.31,32 The loss of accuracy in estimation due to this circumstance should be taken into account, since it leads to overestimating the average risk in the cohort participants. Thus, during primary prevention, it is recommended that diabetic patients should be treated individually based on accurate risk estimation, despite their being at greater risk.
NEW SCREENING STRATEGIES FOR CARDIOVASCULAR DISEASE
New Coronary Risk Markers
During recent years, a large number of factors have been proposed as possible markers and predictors of CVD.94 However, the added value of including other factors in the risk functions to improve the area under the ROC curve of risk estimation remains under discussion.
High-sensitivity C-reactive protein and other inflammation and oxidation markers have been proposed as candidate factors for improving cardiovascular risk prediction.95 This could be of importance due to the inflammatory component of these diseases.95,96 However, the long-term effect of intervention on these markers is to a great extent hypothetical and their contribution to improving the area under the ROC curve is modest when compared to functions that only include classic factors97,98 (Table 3).
The predictive capacity of genetic factors was analyzed in the context of the ARIC (Atherosclerosis Risk in Communities) study and Framingham Offspring study. The former study developed a function that included genetic markers as well as the classic risk factors.99 The latter study assessed the capacity of family background to be an independent predictor of CVD.100 Both studies found that there was a minimal, though clinically irrelevant, improvement in risk prediction, and there was no appreciable improvement in the area under the ROC curve.99,100
The assessment of subclinical atherosclerosis through non-invasive imaging tests has gained the most momentum in recent years. The detection of coronary artery calcium through computerized tomography showed improved risk prediction in individuals presenting intermediate coronary risk (10%-20%) according to the Framingham function.101,102 However, it is expensive, technically complex and involves unacceptably high levels of radiation.103
Carotid intima-media thickness as measured by ultrasound imaging is another of the proposed markers. Even though it is affordable, its predictive value is no better than that provided by classic risk factors and neither does it improve the area under the ROC curve. The main limitation found is that the results vary in relation to the degree of complication of the atherosclerotic lesion and the duration of the disease.103-106
Finally, an ankle-brachial index <0.9, in addition to correlating with a high prevalence of cardiovascular risk factors,107 is a better predictor of atherosclerotic disease than high-sensitivity C-reactive protein and waist circumference.108,109 However, similar to the carotid intima-media index, its predictive value is no better than that of the classic risk factors, despite being affordable.103
Identifying the Vulnerable Individual
The discussion thus focuses on knowing what action is suitable once risk has been estimated, especially for individuals classified in the average risk group who, finally, will present the greatest proportion of cardiovascular events.110,111
Most fatal coronary events have as their starting point the rupture of atheromatous plaque. Based on this finding, a group of experts coined the term "vulnerable patient."112-116 This is an individual identified as likely to suffer a cardiovascular event, based on vulnerable plaque markers (unstable or high-risk), vulnerable blood (tendency to thrombosis), and vulnerable myocardium (electrically unstable or arrhythmogenic).114-116 Detecting vulnerable plaque is obviously the most important of these 3 elements, due to the large number of events that, at least theoretically, would make it possible to predict. As a result of this line of thinking, the SHAPE (Screening for Heart Attack Prevention and Education), report was published which went a step further by recommending the screening of subclinical atherosclerosis through non-invasive tests (detection of coronary artery calcium or carotid intima-media thickness) in men older than 45 years and women older than 55.116
Figure 3 presents a possible algorithm that could be employed in the near future for the primary prevention of IHD. The strategy would consist in detecting risk through the combined use of cardiovascular risk functions, plaque instability markers, imaging techniques, and diagnostic tests for ischemia.111 In principle, classifying the patient using the selected risk function at first screening could lead to taking into account other complementary factors, such as a family background of CVD, obesity, overweight, or the waist circumference, measurement of high-sensitivity C-reactive protein, lipoprotein (a), microalbuminuria, or kidney failure, standardized evaluation of diet quality, and physical activity habits, or even measuring the ankle-brachial index or, in its absence, pedal pulse, whose absence, or weakness may be an adverse cardiovascular sign.
Figure 3. A proposed algorithm for classifying risk in patients in primary prevention for coronary disease. CV indicates cardiovascular. *High-sensitivity C-reactive protein >1 mg/L, family history of early-onset cardiovascular disease, weak/ nonexistent pedal pulse or ankle/brachial index <0.9 or obesity (body mass index >30), waist circumference greater than recommended, microalbuminuria, or kidney failure. Adapted from Braunwald et al110 and Marrugat et al.53
In low-risk patients, the clinical diagnosis may lead to reclassifying those patients who present an unfavorable profile as medium-risk; for example, if they present more than 2 positive complementary factors. In patients initially classified at medium risk, the presence of more than one complementary factor would be sufficient to reclassify them as high risk. Finally, the situation regarding high-risk individuals is clear. These patients present a level of risk close to that of individuals who have already suffered from some manifestation of atherosclerotic disease in whatever location and are candidate for a more intense intervention regarding their classic cardiovascular risk factors, including applying all the pharmacological means necessary for their control.
Unless new evidence becomes available, advice on lifestyle—supported by robust scientific evidence— including giving up smoking, taking physical exercise, following a healthy diet, and reducing weight, is the most widely accepted prevention strategy and should be systematically applied in CVD prevention regardless of the level of cardiovascular risk.5,6
CONCLUSIONS
The primary prevention of CVD is crucial in clinical practice for 3 reasons. First, CVD is the leading cause of mortality in the world, and continues to increase in developing countries. Second, the long induction period— generally asymptomatic—of atherosclerosis means that its first manifestation is frequently an event such as AMI or stroke, and is fatal in more than 35% of cases. Finally, the control of risk factors, that is, factors associated with this disease, leads to a reduction in its incidence.
The estimation of cardiovascular risk makes it possible to structure the primary prevention of CVD toward the best candidates, and thus this procedure should entail the highest level of reliability and accuracy possible. In southern European countries, the burden of classic risk factors in the development of CVD is different from that found in English-speaking countries. In Spain, almost half the incident coronary events and two-thirds of the mortality from this cause occur in people aged more than 65 years. Thus, a function with the required validity can only be constructed based on data specific to the population to which it will be applied and their needs.
The clinical guidelines for the control of CVD, whose morbidity and mortality is very high, will have an impact not only on the individual at risk, but on the population as a whole, as many individual attitudes are shaped by the community's attitude toward health problems. The interventions with greater cardiovascular benefit, such as correctly choosing healthy food, giving up tobacco, taking regular exercise, or losing weight, depend on the individual. It is worth mentioning the current and future impact on the National Health System and its sustainability of the treatment needed to prevent a given number of cardiovascular events from occurring.
During recent years, the low sensitivity of risk functions has led to a large number of factors being proposed as possible markers and predictors of CVD. The screening problem centers on the medium risk group, which is the one presenting the highest proportion of cardiovascular events. Regarding risk estimation, the inclusion of new markers in risk functions remains to be clarified. Despite this, experts persevere in their search for new population screening strategies for atherosclerosis at the population scale to identify the "vulnerable patient" through the use of biological markers and non-invasive imaging techniques that may help increase the effectiveness of the primary prevention of CVD.
Section Sponsored by Laboratorio Dr Esteve
Correspondence: Dr. J. Marrugat.
Unitat de Lipids i Epidemiologia Cardiovascular. IMIM-Hospital del Mar. Dr. Aiguader, 88. 08003 Barcelona. España.
E-mail: jmarrugat@imim.es