We would like to draw attention to the above document, which was recently published simultaneously in Medicina Clínica,1Revista Española de Geriatría y Gerontología,2and SEMERGEN-Medicina de familia.3 Chronic ischemic heart disease affects 5% to 7% of elderly patients, and the treatment approach requires a holistic assessment including comorbidities, frailty, functional status, polypharmacy, and drug interactions. These factors are so common and significant in making patient-centered decisions that some authors consider a subspecialty of geriatric cardiology warranted.4 Asymptomatic or atypical presentation is more common in individuals older than 75 years, and a high percentage of patients cannot exercise to a level sufficient to allow interpretation of stress testing. We advocate medical treatment in most patients. This should include lifestyle modifications. Drugs are often underused in elderly patients, compliance decreases with age,5 effectiveness is lower, adverse effects are more common, and there are more treatment interruptions. Statins are not indicated for patients older than 80 years with severe comorbidity or life expectancy < 3 years, moderate to severe dementia, or significant functional deterioration.6 With the exception of statins, the targets for low-density lipoprotein cholesterol levels and other factors (heart rate, blood pressure) are similar for elderly and general adult patients, although a target blood pressure of < 160 mmHg is sometimes acceptable. In elderly patients, the decision of whether or not to perform coronary revascularization should be made with caution, as interventional procedures and surgery carry a higher complications rate. Elderly patients with chronic ischemic heart disease frequently have comorbidities, frailty, or geriatric syndromes that limit the therapeutic possibilities and confer a worse prognosis. Most elderly patients demonstrate frailty criteria. Such criteria confer a 2-4 fold increase in mortality. Cognitive decline is also very common, which can make treatment adherence difficult. Likewise, depression, which confers a worse prognosis, and other comorbidities (diabetes mellitus, kidney disease) are frequently present. A holistic biopsychosocial assessment is essential, taking into account functional assessment, frailty, cognitive function, social situation, life expectancy, and the patient's wishes and directives (Table). Such an assessment is required to balance the risk-benefit ratio and be confident that in the prognostic prediction, the competing risk associated with these geriatric conditions is not higher than that associated with the coronary disease itself.
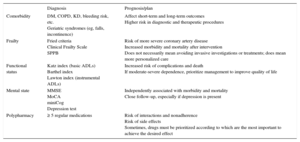
Geriatric Factors Evaluated
| Diagnosis | Prognosis/plan | |
|---|---|---|
| Comorbidity | DM, COPD, KD, bleeding risk, etc. Geriatric syndromes (eg, falls, incontinence) | Affect short-term and long-term outcomes Higher risk in diagnostic and therapeutic procedures |
| Frailty | Fried criteria Clinical Frailty Scale SPPB | Risk of more severe coronary artery disease Increased morbidity and mortality after intervention Does not necessarily mean avoiding invasive investigations or treatments; does mean more personalized care |
| Functional status | Katz index (basic ADLs) Barthel index Lawton index (instrumental ADLs) | Increased risk of complications and death If moderate-severe dependence, prioritize management to improve quality of life |
| Mental state | MMSE MoCA miniCog Depression test | Independently associated with morbidity and mortality Close follow-up, especially if depression is present |
| Polypharmacy | ≥ 5 regular medications | Risk of interactions and nonadherence Risk of side effects Sometimes, drugs must be prioritized according to which are the most important to achieve the desired effect |
ADLs, activities of daily living; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; KD, kidney disease; miniCog, Mini-Cognitive Assessment Instrument, a simple test (2 questions and drawing a clock) for screening of cognitive decline; MMSE, Mini Mental Examination; MoCA, Montreal Cognitive Assessment; SPPB, Short Physical Performance Battery (assesses balance, walking speed, and ability to rise from sitting to standing).
Fried Criteria: assesses 5 criteria (involuntary weight loss, exhaustion, low physical activity, slow walking speed, and low muscle strength); 3 or more criteria indicate frailty. Clinical Frailty Scale: scale between 1 (very fit) and 9 (terminally ill); the assessment includes different deficits, illnesses, and disabilities.
Reproduced with permission from Martínez-Sellés et al.1
E. Abu-Assi is Associate Editor of Revista Española de Cardiología.