Chronic thromboembolic pulmonary hypertension (CTEPH) treatment has evolved in the last decade. However, there is scarce information on the long-term impact of this progress in a real-life population at a national level. This study was designed to analyze the characteristics of CTEPH patients in Spain over the last decade.
MethodsWe prospectively collected epidemiological, clinical, and prognostic data from CTEPH patients consecutively included in the Spanish REHAP registry from January 1, 2007, to December 31, 2018. We evaluated differences over time, establishing 2013 as the reference date for analysis. Propensity scores for interventional treatment were calculated using a multivariable logistic regression model.
ResultsA total of 1019 patients were included; 659 (64.4%) were evaluated at a national CTEPH center. Overall, 350 patients (34.3%) were selected for surgery and 97 (9.6%) for percutaneous treatment. Patients diagnosed between 2007 and 2012 died more frequently than those diagnosed from 2013 onward (HR, 1.83; 95%CI, 1.07-3.15; P=.027). Within the subgroup of patients adjusted by propensity score, baseline pulmonary vascular resistance and the 6-minute walk test distance also determined the outcome (HR, 1.24; 95%CI, 1.15-1.33; P=.011; and HR, 0.93; 95%CI, 0.90-0.97; P=.001, respectively). High survival rates were found in patients who underwent an invasive procedure (pulmonary endarterectomy or balloon pulmonary angioplasty).
ConclusionsCTEPH diagnosis and prognosis have consistently improved in the last decade. Baseline disease severity determines the risk profile. Patients who undergo pulmonary endarterectomy or balloon pulmonary angioplasty have better outcomes.
Keywords
Chronic thromboembolic disease represents a potentially curable cause of pulmonary hypertension (PH).1 Whereas pulmonary endarterectomy (PEA) was the sole evidence-based treatment for chronic thromboembolic pulmonary hypertension (CTEPH) in 2007, the landscape of the disease has undoubtedly changed over the last decade with the subsequent implementation of balloon pulmonary angioplasty (BPA) programs2,3—available in Spain since 2013 4—and the evidence supporting the clinical benefit of riociguat therapy—commercialized in Spain since 2015—for inoperable and persistent CTEPH.5 Unfortunately, epidemiological and clinical studies are still scarce. Accordingly, specific registries are particularly useful to deepen our understanding of low-prevalence diseases such as CTEPH. One such registry of Spanish patients with PH, the REHAP registry, provides useful information on real-life practice. It comprises 40 Spanish hospitals and provides demographic, clinical, and prognostic data on these patients.6
Regarding the assessment of rare disease outcomes, the difficulties associated with the proper development of clinical trials, based on traditional statistical methods, are already well-known. In this respect, propensity score analysis has been described as a particularly useful tool to avoid potential confounders and to adjust for treatment biases in observational studies of uncommon pathologies.7 However, this approach had not been specifically applied to the study of CTEPH prognosis.
Accordingly, this study was designed to describe the demographic and clinical profile of CTEPH patients in Spain and to evaluate the outcomes of these patients over the last decade.
MethodsStudy setting and populationWe conducted a multicenter, nationwide, long-term cohort study of a population with CTEPH diagnosis in Spain. Patients’ data were prospectively included in the Spanish REHAP registry from January 1, 2007, to December 31, 2018, and retrospectively analyzed. Because the BPA program was implemented in Spain in 2013, we considered this year the reference date for comparisons.
All patients met CTEPH diagnostic criteria: mean pulmonary artery pressure (mPAP) estimated by right heart catheterization> 25mmHg, pulmonary capillary wedge pressure <15mmHg, pulmonary vascular resistance (PVR)> 240 din/s/cm5, perfusion defects on lung scintigraphy, and radiologic signs of pulmonary thromboembolic disease on computed tomography or pulmonary angiography. Patients <18 years old were excluded.
The day of the first right heart catheterization was considered the date of CTEPH diagnosis. Each hospital had its own process for assessing the therapeutic approach, including whether or not to refer the patient to an expert PH center. Residual PH at least 6 months after PEA or the last BPA procedure was considered significant if the final PVR exceeded 416 din/s/cm5 and/or if the final mPAP exceeded 30mmHg.8,9 Patients were followed up until death or study end (December 31, 2018). The study was approved by the appropriate research ethics committee.
Statistical analysisBaseline characteristics were compared using a t test for continuous variables and the chi-square or ANOVA tests of proportions for categorical variables. Analyses were conducted by using SPSS version 22.0 software (SPSS Inc, Chicago, IL, United States).
A propensity score model was used to predict the probability of interventional treatment (PEA and/or BPA). Propensity scores facilitated a similar distribution of baseline characteristics between interventional treatment and medical therapy groups, minimizing the selection bias of observational studies. We selected baseline variables that were significantly associated with PEA/BPA in the univariate analysis (age, treatment with prostanoid analogs, PVR at diagnosis, period of diagnosis). Patients who underwent BPA or PEA were matched 1:1 with those who did not, based on the propensity scores calculated using the nearest-neighbor technique (standardized difference <0.05%). The internal validation error of the constructed model was 0.03. This matching process selected 2 cohorts of 294 patients. These patients were divided into 2 subgroups according to the treatment strategy selected (table 1 of the supplementary data) to further compare differences related to their characteristics and prognoses.
We first described survival in the general population. Overall mortality was defined as death from any cause during the study period. In a subsequent analysis, we evaluated prognostic data from the matched population. Cox regression analysis and Kaplan-Meier curves were used to assess mortality. The final multivariate regression model for the matched sample included all variables showing a significant association in the univariable analysis (table 2 of the supplementary data) and those considered clinically relevant (age and sex).
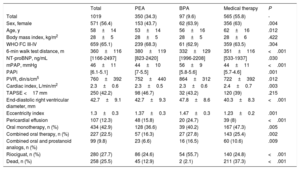
ResultsBaseline characteristicsA total of 1019 patients were included during the study period, 451 (44.3%) from 2007 to 2012. The mean age was 61±15 years and 56.5% were women. In total, 97 patients (9.6%) were selected for percutaneous treatment with BPA and 350 (34.3%) for surgery (table 1). The median duration of follow-up for the patients in this study was 1095 days [0-7665 days].
Baseline characteristics of patients included in the REHAP registry from 2007 to 2018
| Total | PEA | BPA | Medical therapy | P | |
|---|---|---|---|---|---|
| Total | 1019 | 350 (34.3) | 97 (9.6) | 565 (55.8) | - |
| Sex, female | 571 (56.4) | 153 (43.7) | 62 (63.9) | 356 (63) | .004 |
| Age, y | 58±14 | 53±14 | 56±16 | 62±16 | .012 |
| Body mass index, kg/m2 | 28±5 | 28±5 | 28±5 | 28±6 | .422 |
| WHO FC III-IV | 659 (65.1) | 239 (68.3) | 61 (62.9) | 359 (63.5) | .304 |
| 6-min walk test distance, m | 360±116 | 380±119 | 332±129 | 351±116 | <.001 |
| NT-proBNP, ng/mL | [1166-2497] | [823-2420] | [1996-2208] | [533-1937] | .030 |
| mPAP, mmHg | 46±11 | 44±10 | 56±9 | 44±11 | <.001 |
| PAPi | [6.1-5.1] | [7-5.5] | [5.8-5.6] | [5.7-4.6] | .001 |
| PVR, din/s/cm5 | 760±392 | 752±440 | 864±312 | 722±392 | .012 |
| Cardiac index, L/min/m2 | 2.3±0.6 | 2.3±0.5 | 2.3±0.6 | 2.4±0.7 | .003 |
| TAPSE <17 mm | 250 (42.2) | 98 (46.7) | 32 (43.2) | 120 (39) | .215 |
| End-diastolic right ventricular diameter, mm | 42.7±9.1 | 42.7±9.3 | 47.8±8.6 | 40.3±8.3 | <.001 |
| Eccentricity index | 1.3±0.3 | 1.37±0.3 | 1.47±0.3 | 1.23±0.2 | .001 |
| Pericardial effusion | 107 (12.3) | 48 (15.8) | 20 (24.7) | 39 (8) | <.001 |
| Oral monotherapy, n (%) | 434 (42.9) | 128 (36.6) | 39 (40.2) | 167 (47.3) | .005 |
| Combined oral therapy, n (%) | 227 (22.5) | 57 (16.3) | 27 (27.8) | 143 (25.4) | .002 |
| Combined oral and prostanoid analogs, n (%) | 99 (9.8) | 23 (6.6) | 16 (16.5) | 60 (10.6) | .009 |
| Riociguat, n (%) | 280 (27.7) | 86 (24.6) | 54 (55.7) | 140 (24.8) | <.001 |
| Dead, n (%) | 258 (25.5) | 45 (12.9) | 2 (2.1) | 211 (37.3) | <.001 |
BPA, balloon pulmonary angioplasty; mPAP, mean pulmonary artery pressure; NT-proBNP, N-terminal pro-B-type natriuretic peptide; PAPi, pulmonary artery pulsatility index; PEA, pulmonary endarterectomy; PVR, pulmonary vascular resistance; TAPSE, tricuspid annular plane systolic excursion; WHO FC, World Health Organization functional class.
Data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
Most patients (55.8%) received medical therapy exclusively with specific PH drugs. These patients were older than those who were selected for PEA or BPA (table 1). Patients included in the BPA program had the worst hemodynamic condition at diagnosis. Interestingly, 7 patients underwent lung transplantation, 6 of whom were diagnosed before 2013.
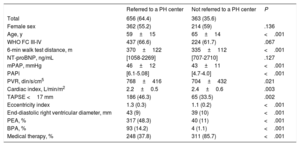
Referral to national chronic thromboembolic pulmonary hypertension centersOf the 1019 patients, 656 (64.4%) were referred to an expert CTEPH center. There were significant differences between the 2 groups (table 2). Patients who were evaluated at an expert CTEPH center were younger and had more advanced disease at presentation (higher PVR, signs of severe right ventricular dysfunction). They also benefited from interventional treatment more than those who were exclusively evaluated at their local centers.
Demographic and clinical differences between patients evaluated at local and referral centers
| Referred to a PH center | Not referred to a PH center | P | |
|---|---|---|---|
| Total | 656 (64.4) | 363 (35.6) | |
| Female sex | 362 (55.2) | 214 (59) | .136 |
| Age, y | 59±15 | 65±14 | <.001 |
| WHO FC III-IV | 437 (66.6) | 224 (61.7) | .067 |
| 6-min walk test distance, m | 370±122 | 335±112 | <.001 |
| NT-proBNP, ng/mL | [1058-2269] | [707-2710] | .127 |
| mPAP, mmHg | 46±12 | 43±11 | <.001 |
| PAPi | [6.1-5.08] | [4.7-4.0] | <.001 |
| PVR, din/s/cm5 | 768±416 | 704±432 | .021 |
| Cardiac index, L/min/m2 | 2.2±0.5 | 2.4±0.6 | .003 |
| TAPSE <17 mm | 186 (46.3) | 65 (33.5) | .002 |
| Eccentricity index | 1.3 (0.3) | 1.1 (0.2) | <.001 |
| End-diastolic right ventricular diameter, mm | 43 (9) | 39 (10) | <.001 |
| PEA, % | 317 (48.3) | 40 (11) | <.001 |
| BPA, % | 93 (14.2) | 4 (1.1) | <.001 |
| Medical therapy, % | 248 (37.8) | 311 (85.7) | <.001 |
BPA, balloon pulmonary angioplasty; mPAP, mean pulmonary artery pressure; NT-proBNP, N-terminal pro-B-type natriuretic peptide; PAPi, pulmonary artery pulsatility index; PEA, pulmonary endarterectomy; PH, pulmonary hypertension; PVR, pulmonary vascular resistance; TAPSE, tricuspid annular plane systolic excursion; WHO FC, World Health Organization functional class.
Data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The incidence rate described here expresses the number of new cases of CTEPH reported to the REHAP registry in the Spanish adult population, as defined by the Spanish census, within the selected period of time. The CTEPH incidence based on Spanish adult population data10 was 0.9 cases per year per million individuals in 20076 and rose to 1.7 cases per year per million population in 2018. Similarly, the recorded CTEPH prevalence (based on cases reported to the REHAP registry) increased from 3.2 in 200710 to 22.5 per million population in 2018. Changes concerning CTEPH treatment during the study period are displayed in table 3 of the supplementary data.
Clinical and hemodynamic responses after pulmonary endarterectomy and balloon pulmonary angioplastyClinical and hemodynamic improvement after pulmonary endarterectomyOf the 350 PEA patients, exercise tolerance and pulmonary hemodynamic consistently improved after surgery (figure 1 and table 4 of the supplementary data). Right heart catheterization (6 months after surgery) revealed significant PH in 59 patients (16.8%). Seven patients who underwent PEA were later included in the BPA program. The overall perioperative mortality rate was 3.8% (13 patients).
Clinical and hemodynamic improvement after balloon pulmonary angioplastyOf the 97 BPA patients, 66 (68%) had completed the BPA sessions by the cutoff date. BPA patients underwent a total of 443 sessions, with an average of 4.5±2.4 procedures per patient. Four patients were excluded from the program due to a lack of improvement. Regarding safety, 1 death occurred during the entire study period due to complications related to the BPA procedure.
A comparison of baseline and post-BPA characteristics among patients who had completed the BPA program revealed a significant improvement in clinical and hemodynamic parameters (figure 1 and table 4 of the supplementary data).
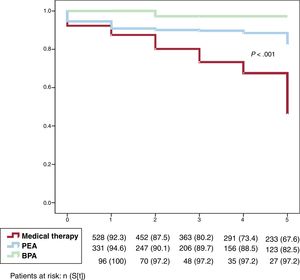
OutcomesMortality in the general populationDuring follow-up, 259 patients (25.4%) died. Those who died were more likely to have a worse hemodynamic condition at diagnosis. The long-term global impact of the chosen therapeutic strategy on outcome is shown in figure 2. Patients who underwent PEA or those selected for BPA had better survival rates than patients exclusively treated with PH-specific drugs (P <.0001).
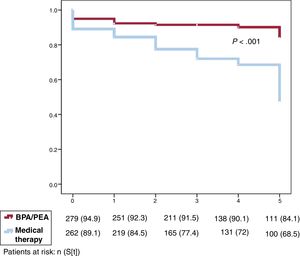
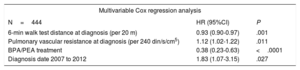
Propensity scoring and predictors of mortality within the matched cohortThe survival curves of the 2 propensity-matched cohorts were similar to those obtained for the whole sample (figure 3). Results for variables independently associated with mortality in the univariable analysis are summarized in table 2 of the supplementary data.
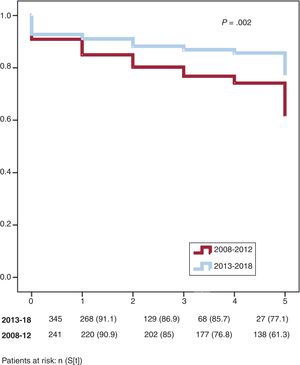
Multivariable Cox regression analysis adjusted to the matched cohort revealed that the patients with the worst prognosis were diagnosed before 2013, were ineligible for surgical or percutaneous intervention, and had more severe disease (figure 4 and table 3).
Analysis of the survival of patients within the matched cohort
| Multivariable Cox regression analysis | ||
|---|---|---|
| N=444 | HR (95%CI) | P |
| 6-min walk test distance at diagnosis (per 20 m) | 0.93 (0.90-0.97) | .001 |
| Pulmonary vascular resistance at diagnosis (per 240 din/s/cm5) | 1.12 (1.02-1.22) | .011 |
| BPA/PEA treatment | 0.38 (0.23-0.63) | <.0001 |
| Diagnosis date 2007 to 2012 | 1.83 (1.07-3.15) | .027 |
95%CI, 95% confidence interval; BPA, balloon pulmonary angioplasty; HR, hazard ratio; PEA, pulmonary endarterectomy.
Here, we describe the evolving trends in the demographic and prognostic profile of CTEPH patients in Spain from 2007 to 2018. To the best of our knowledge, this is the first specific study to evaluate long-term outcomes, based on a national registry data including BPA patients.
Our research reveals at least 3 key findings with significant implications for improving the standard of CTEPH care in Spain. First, we showed a remarkable increase in CTEPH survival throughout the study period. Second, we found that CTEPH outcome was strongly determined by access to specific resources, such as BPA or PEA. This was in turn related to the relationship with expert national CTEPH centers in the network. Finally, and despite the observational nature of our investigation, the application of a propensity score-matching model allowed us to obtain an unbiased estimation of treatment effects, mimicking some of the characteristics of a randomized study.
An epidemiological perspective on chronic thromboembolic pulmonary hypertension: from center-based expertise to national registriesWe prospectively analyzed data from the Spanish REHAP registry. Unlike other countries,11–14 the assessment and prescription of PH treatment in Spain is not strictly limited to expert PH centers and can be made by any specialist in the public health system. Therefore, the Spanish REHAP registry is open to voluntary participation by all physicians who treat patients with PH (subgroups 1 and 4), all over the country. This approach enables a more comprehensive picture, accurately reflecting the national CTEPH landscape.
Observational registries represent a feasible way to deepen knowledge about the clinical history of uncommon diseases such as CTEPH and to assess their long-term outcomes. Accordingly, it is crucial to determine the primary source of information, which depends on each country's health care system. In this regard, Gibbs et al.15 have described the role and structure of PH networks in France and the United Kingdom. Their registries are both based on data from expert PH centers, which usually organize the patients’ entire medical care. Likewise, the ASPIRE registry16 and the German13 and Swiss17 national series share the same design. A major strength of our study is that we also provide epidemiological information related to patients who were assessed and treated at nonreferral hospitals.
National registries are usually used to calculate the incidence and prevalence rates for entire populations.18 Because the REHAP data do not consider the entire Spanish National Health System, we offer the most approximated epidemiological information we could obtain. We found a growing trend in reported incident cases throughout the study period. Although our findings are still far from those of German registries (reported incidence of 5.7/million in 201613), an increasing awareness of the disease has resulted in a substantial growth in reported CTEPH cases in Spain over the last decade (from 0.9 in 2007 to 1.7/million in 2018).
According to Skride et al.,19 who compared different CTEPH registries in Europe, the lowest CTEPH prevalence was reported in Spain (2012) and the highest in Sweden. However, the current Spanish CTEPH prevalence has increased to 22.5/million population, data more consistent with the Swedish series. This dramatic increase in prevalence (from 3.2/million in 2007 to 22.5/million in 2018) could be explained by the reduction in disease-specific mortality and the standardization of patient registry data fostered by the REHAP.
National chronic thromboembolic pulmonary hypertension centersThere are 2 national CTEPH centers in Spain (Hospital 12 de Octubre, Madrid, and Hospital Clínic, Barcelona). Each local hospital evaluates and provides PH treatment according to its own criteria. In our series, 64.4% of the patients were referred to expert centers for a more thorough evaluation. Although the Spanish referral rate for PEA evaluation is above average (44% in Europe19), this decentralized health care model results in nonhomogeneous medical assistance: patients who were assessed at the national CTEPH centers were much more likely to benefit from PEA or BPA techniques (table 2).
This reinforces the argument that access to expert centers ensures optimal care. As has been previously stated by Escribano et al.,20 patients who were not assessed in a CTEPH referral hospital were less likely to undergo surgery. Consistent with these results, an international prospective registry found that low-volume PEA centers (< 10 PEA/y) reported a significantly higher rate of “nonoperable” patients,21 also suggesting that accessibility to high-volume specialized PEA centers might influence the final therapeutic approach.
Trends in chronic thromboembolic pulmonary hypertension over the last decade: clinical profiles and therapeutic strategiesThe rise in the reported incidence of CTEPH in Spain was associated with a major shift in the clinical profile of CTEPH patients, with the hemodynamic status at diagnosis improving with time. Patients diagnosed between 2007 and 2012 had a worse clinical and hemodynamic condition at inclusion (table 3 of the supplementary data). The diagnosis date was also related to a poorer prognosis (figure 4). Changes in CTEPH treatment over the last decade may have influenced these outcomes. Remarkably, even with the implementation of BPA programs, the number of patients referred for PEA consistently increased from 2007 to 2017 (P <.0001). On the other hand, medical therapy with prostacyclin analogs drastically decreased from one period to the other (P <.0001), probably due to the wider pool of resources for treating these patients. Similar to the national series from the United Kingdom,12 a small number of patients underwent transplantation.
Chronic thromboembolic pulmonary hypertension treatment in SpainPulmonary endarterectomyPEA, when suitable, remains the best choice for CTEPH treatment.1 In our series, patients undergoing surgery were younger but had a similar baseline hemodynamic condition to inoperable patients, as has been described in previous studies.12,21
Patients who underwent surgery experienced a significant improvement in both hemodynamic and clinical status. This perfectly aligns with the findings of a recent meta-analysis including 4868 CTEPH patients: PEA significantly reduced mPAP and PVR and increased the 6-minute walk distance.22 They also reported that 16.7% to 35% of patients experience PH after PEA, which places CTEPH surgery in Spain (with a 16.8% rate of significant residual PH) in good stead.
Balloon pulmonary angioplastyPromising therapies for inoperable patients have been developed during the last 10 years. For example, BPA improves outcomes in inoperable CTEPH patients.2 In our series, patients selected for BPA were significantly older and had the worst baseline hemodynamic situation. In terms of other series, Brenot et al.9 have recently described the experience of BPA implementation in a French CTEPH center (184 patients, included in 2014-2017). The BPA patients in their cohort were less symptomatic and had a lower PVR and higher cardiac index than in ours. They reported 4 peri-procedural deaths (2.2% vs 1%) and similar 1- and 3-year overall survival curves.
Despite these adverse conditions, BPA significantly increased the cardiac index, with a remarkable reduction in PVR and mPAP. Our results are consistent in terms of hemodynamic and functional improvements and safety with those of a recently published meta-analysis23 indicating BPA as a plausible adjunctive therapy for CTEPH patients.
Pulmonary hypertension medical therapyMost of the patients (55.2%) exclusively received PH-targeted medical therapy. Riociguat, the only approved therapeutic option for inoperable or persistent/recurrent CTEPH patients,1,5 was the chosen drug for treatment in 280 of the patients (27.5%). Interestingly, an aggressive combined therapy that included prostacyclin pathway agonists was the selected option in several patients. In such cases, PH-specific therapy was given to improve clinical outcomes, in accordance with evidence-based treatment recommendations for arterial PH,1 although this treatment schedule is not approved for CTEPH management. Our results differed from those published by Mueller-Mottet et al.17 concerning data from the Swiss PH registry collected from 1998 to 2012 (no drug, 27%; single drug, 65%; double combination, 19%; triple combination, 0.4%): the use of pulmonary vasodilators was markedly higher among Spanish patients. Our series also reflects how often specific vasodilators are used off-label to treat CTEPH patients and also reinforces the recommendation to refer these patients to expert PH centers to improve their diagnosis, treatment, and prognosis.
Current outcomes in chronic thromboembolic pulmonary hypertensionOur mortality rate was slightly better than those reported by other European CTEPH registries.8,13,19 Compared with a national study conducted before 2013, CTEPH prognosis in Spain has considerably improved.20 Mortality in the PEA subgroup was comparable to that reported by Delcroix et al.24 for 679 patients included in an international European registry. In the BPA subgroup, the survival rates of percutaneous therapy intervention were remarkably high, despite the particularly unfavorable hemodynamic conditions at diagnosis. Our results were similar to those reported in a Japanese series.25 The safety and efficacy of this procedure make this technique a favorable choice for CTEPH management.
Multivariable Cox regression analysis of the propensity-matched cohort showed that, ultimately, prognosis mainly depended on disease severity and the chosen therapeutic strategy. Those who were not selected for any interventional procedure (PEA or BPA) had a particularly somber outcome. We cannot exclude the possibility that some of the patients of the medical subgroup were suitable candidates for PEA or determine if BPA was considered an alternative for every CTEPH patient declared inoperable. It is therefore important to underscore the relevance of reference PH centers to raise the overall quality of care and improve long-term outcomes.
LimitationsBecause REHAP is a voluntary observational registry, incomplete reporting may lead to missing data. The BPA program was not finalized for every patient by the end date. As such, the results are incomplete in terms of the ultimate improvement. Because we compared historical cohorts, changes introduced from 2013 onward may have biased the results (the Will Rogers phenomenon). Although observational investigations are not the most appropriate method to evaluate survival improvements, the propensity score-matching analysis method aims to reduce the statistical bias by distributing the patient's baseline characteristics as uniformly as possible.
ConclusionsIn summary, our results confirm that CTEPH management has already changed over the last decade in Spain. The risk profile, which has evolved over time due to improvements in diagnosis and treatment, was mainly determined by the severity of the disease. Without interventional therapies, the overall long-term CTEPH prognosis is adverse. BPA is an encouraging therapy for inoperable patients in the near future.
ConflictS of interestP. Martínez-Santos has received personal fees from MSD and Actelion (fees for medical education services). M.T. Velázquez-Martín has received grants from MSD and Actelion (consulting fees and fees for medical education services). M. López-Meseguer has received personal fees from MSD and Actelion (fees for medical education services and advisories). J.A. Domingo-Morera has received grants from MSD and Actelion (consulting fees and fees for medical education services). I. Blanco has received personal fees from MSD and Actelion (consulting fees). P. Escribano-Subías has received grants from MSD, GSK, and Actelion (consulting fees and fees for medical education services). The other authors declare no conflicts of interest.
- –
CTEPH represents a potentially curable cause of PH.
- –
There is growing interest in the impact of therapies developed in recent years on real-life populations.
- –
The reported incidence of CTEPH has substantially increased in Spain over the last decade.
- –
Baseline condition at diagnosis, referral to expert PH centers, and access to PEA and BPA have also improved from 2007-2012 to 2013-2018.
- –
The survival rates of patients who underwent PEA or BPA were notably higher than those who received targeted medical therapy alone.
We gratefully acknowledge the support of all of the investigators of the REHAP registry and the S&H Medical Science Service coordinating center.
The Spanish Registry of Pulmonary Arterial Hypertension (Registro Español de Hipertensión Arterial Pulmonar) investigators are: P. Escribano, I. Blanco, J. De Miguel, M. Lázaro, A. Castro, M.S. Alcasena, S. Alcolea, J.A. Barberá, E. Barrios, P. Bedate, S. Cadenas, J.M. Cifrián, J.A. Domingo, L. Dos, T. Elías, F.J. García-Hernández, J. Gaudó, J. Gil Carbonell, A. González, L. Jara, A. Lara, M. López, R. López-Reyes, M.J. López-Gude, M. López-Meseguer, A. Martínez, P. Martínez, L. Molina, T. Mombiela, R. Otero Candelera, I. Otero, F. Pastor, C.A. Quezada, A. Román, J. Rueda, E. Sala, L. Sebastián, J. Segovia, M.T. Subirana.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.06.006