Low-density lipoprotein cholesterol (LDL-C) is a major risk factor for the development of acute coronary syndrome (ACS).1,2 The objective of this study was to describe the clinical characteristics and prognosis of patients hospitalized for ACS with an LDL-C concentration of <70mg/dL.
This was a prospective, observational, single-center study, including all consecutive patients hospitalized for ACS. Among the 680 candidate hospitalized patients, the following were excluded: 17 patients in whom LDL-C could not be determined because triglyceride levels were >400mg/dL, 10 who died before analytical determinations could be obtained, and 4 who did not have test results from the first 72h following hospitalization. The final sample comprised 649 patients.
The main objective of the study was to determine the incidence of death from any cause, and the secondary aim was the incidence of death or nonfatal ACS. A fasting blood sample was taken for lipid profile analysis in the first 24 to 72 h following hospital admission. Patients were divided into two groups according to whether their LDL-C level was <70 or ≥70 mg/dL.
Statistical analyses were performed with SPSS 16.0 (SPSS Inc.; Chicago, Illinois, United States). Qualitative variables were evaluated using the chi-square test or Fisher exact test. Quantitative variables were compared with the Student t test and ANOVA. Survival during follow-up was analyzed by Cox proportional hazards regression with a forward stepwise selection procedure. Statistical significance was set at P<.05.
One fourth of patients presented LDL-C values <70mg/dL and a more unfavorable cardiovascular risk profile (Table 1). At hospital discharge, these patients were prescribed diuretics (P=.02), anticoagulants (P=.04), and oral antidiabetic agents (P=.04) more often than patients with higher LDL-C values, with no differences in statin treatment (92.8% vs 94.2%, respectively; P=.53) or other treatments. The most commonly used statin was atorvastatin (79.4%). Patients with LDL-C <70mg/dL received a lower daily dose (60.1±23.8 vs 67.9±20.5; P<.01) and a dose of 80 mg/day less often (56.5% vs 72.8%; P<.01) than those with higher values.
General Characteristics of Patients According to Low-density Lipoprotein Cholesterol Values
| Total | LDL-C ≥70 mg/dL | LDL-C <70 mg/dL | P | |
| Patients | 649 | 484 (74.6) | 165 (25.4) | |
| Age, years | 69.4±12.5 | 68.0±12.5 | 73.6±11.3 | <.01 |
| Men, % | 72.7 | 71.0 | 77.6 | .10 |
| BMI, kg/m2 | 27.5±4.7 | 27.7±4.9 | 26.9±3.8 | .07 |
| Diabetes mellitus, % | 38.8 | 34.6 | 50.9 | <.01 |
| Hypertension, % | 71.2 | 67.1 | 83.0 | <.01 |
| Smokers, % | 29.0 | 32.1 | 20.0 | <.01 |
| Dyslipidemia, % | 52.9 | 51.5 | 57.0 | .22 |
| Previous IHD, % | 34.6 | 30.4 | 46.7 | <.01 |
| Previous HF, % | 3.6 | 2.5 | 6.7 | .01 |
| Previous stroke, % | 5.6 | 4.4 | 9.1 | .02 |
| LVEF, % | 56.7±11.2 | 57.4±10.5 | 54.5±12.6 | .01 |
| STEACS, % | 30.2 | 29.4 | 32.7 | .42 |
| Revascularization, % | 91.2 | 91.4 | 90.6 | .75 |
| Treatment with statins, % | 29.6 | 25.5 | 41.5 | <.01 |
| Total cholesterol, mg/dL | 160.5±43.9 | 175.7±39.1 | 116.0±21.3 | <.01 |
| LDL-C, mg/dL | 96.5±36.2 | 109.9±31.9 | 57.2±10.0 | <.01 |
| HDL-C, mg/dL | 37.0±10.0 | 37.8±10.1 | 34.7±9.3 | .10 |
| Triglycerides, mg/dL | 122.0 (96.0-160.0) | 129.0 (103.0-166.8) | 105.0 (79.0-136.0) | <.01 |
| Non-HDL cholesterol, mg/dL | 123.5±41.6 | 137.9±37.1 | 81.2±19.4 | <.01 |
| Glucose, mg/dL | 116.0±39.6 | 114.6±39.7 | 119.9±39.2 | .16 |
| Creatinine, mg/dL | 1.1±0.5 | 1.1±0.5 | 1.1±0.5 | .50 |
| GF, mL/min/1.72 m2 | 75.4±25.9 | 76.0±24.7 | 73.6±29.0 | .31 |
BMI, body mass index; GF, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; HF, heart failure; IHD, ischemic heart disease; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; STEACS, ST-elevation acute coronary syndrome.
Unless otherwise indicated, values are expressed as n (%), mean±standard deviation, or mean (range).
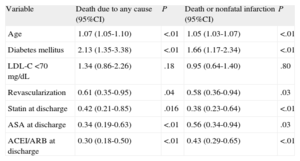
During follow-up (mean, 447.3±110.6 days), patients with LDL-C <70mg/dL presented a higher incidence of all-cause death than patients with higher LDL-C levels (31 [18.8%] vs 53 [11.0%]; P=.01) mainly because of deaths due to a cardiovascular cause (23 [13.9%] vs 43 [8.8%]; P=.05), and a trend to a higher incidence of ACS (45 [27.3%] vs 99 [20.6%]; P=.07); there were no differences according to previous treatment with statins in patients with LDL-C <70mg/dL. However, on multivariate Cox regression analysis adjusted for risk factors, revascularization, and treatments at discharge, LDL-C <70mg/dL was not associated with a worse prognosis (Table 2). Similar benefits of statins, medical treatment, and revascularization were observed in both groups.
Results for Variables Associated With Death Due to Any Cause and Death or Nonfatal Infarction During Follow-up, Analyzed by Cox Regression
| Variable | Death due to any cause (95%CI) | P | Death or nonfatal infarction (95%CI) | P |
| Age | 1.07 (1.05-1.10) | <.01 | 1.05 (1.03-1.07) | <.01 |
| Diabetes mellitus | 2.13 (1.35-3.38) | <.01 | 1.66 (1.17-2.34) | <.01 |
| LDL-C <70 mg/dL | 1.34 (0.86-2.26) | .18 | 0.95 (0.64-1.40) | .80 |
| Revascularization | 0.61 (0.35-0.95) | .04 | 0.58 (0.36-0.94) | .03 |
| Statin at discharge | 0.42 (0.21-0.85) | .016 | 0.38 (0.23-0.64) | <.01 |
| ASA at discharge | 0.34 (0.19-0.63) | <.01 | 0.56 (0.34-0.94) | .03 |
| ACEI/ARB at discharge | 0.30 (0.18-0.50) | <.01 | 0.43 (0.29-0.65) | <.01 |
95%CI, 95% confidence interval; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blocker; ASA, acetylsalicylic acid; LDL-C, low-density lipoprotein cholesterol.
An LDL-C value <70g/dL has been established as a treatment objective for patients at high or very high cardiovascular risk.3 Nonetheless, up to 21% of patients who achieve LDL-C <70mg/dL present coronary plaque progression, attributed to other coronary risk factors.4 Our results are in keeping with these findings and may indicate that having an ACS despite very low LDL-C values reflects the presence of more advanced coronary disease with especially vulnerable coronary lesions. The baseline characteristics of these patients indicate a larger number of comorbid conditions, some of which may not have been collected in this study, and this might explain the higher rate of complications in the group with LDL-C <70. Furthermore, it is known that other lipoproteins (apolipoprotein B, non-high density lipoprotein cholesterol) have a higher predictive value than LDL-C.5
The best lipid-lowering strategy in patients with ACS and low LDL-C is not well established. One observational study showed that patients with ACS and LDL-C <70mg/dL benefited from treatment with statins in the combined objective, cardiovascular complications.1 Our data are in accordance with these results, and additionally show the benefit of revascularization and other treatments in patients with LDL-C <70mg/dL, as well as the poor prognosis of those receiving acetylsalicylic acid.
Our study has certain limitations. It was carried out in a single center and there may have been a change in LDL-C measurement, although the clinical characteristics and lipid values are similar to those of other studies.2 We cannot exclude the effect of comorbidities that would explain why statins or other drugs were not prescribed.
In conclusion, one fourth of patients presenting an ACS had LDL-C values <70mg/dL at the time of hospitalization. Although they later presented higher crude rates of cardiovascular complications, this seems to be explained by other factors. Patients with LDL-C <70mg/dL would equally benefit from treatment with statins following an ACS.