The term embolic stroke of undetermined source (ESUS) was defined some years ago and is aimed at standardizing the diagnostic process to establish the etiology of cerebral infarct and at finding a new antithrombotic strategy (with direct oral anticoagulants [DOACs]) to reduce the high percentage of recurrences experienced by these patients (5% a year).1 The first objective has been achieved, and the routine diagnostic workup now includes laboratory tests, cranial computed tomography or magnetic resonance imaging, a study of the supra-aortic trunks and intracranial arteries, a cardiologic study including echocardiography, and heart monitoring for at least 20 hours.1 Nevertheless, 20% to 25% of strokes are still classified as cryptogenic strokes, usually ESUS, where the potential origin of the culprit embolus is unknown. These emboli may be related to atheromatous plaques in the aortic arch or supra-aortic trunks with no significant stenosis or with the presence of known or occult neoplasms. They may also be heart-related in the case of hidden atrial fibrillation (AF) or minor cardioembolic sources, such as some valve diseases or cardiac contractility abnormalities.2 Among these cardiac abnormalities, patent foramen ovale (PFO) should be considered.
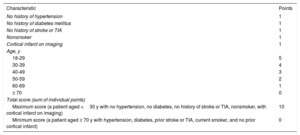
Approximately 25% of the general population has a PFO, but the condition is not known to lead to a higher risk of stroke.3 However, the prevalence of PFO is significantly higher in patients with a history of cryptogenic stroke than in patients with a stroke of known cause or in the general population.4 This potential causal relationship is clearer in younger compared with older patients, and weaker in patients with risk factors for atherosclerosis.5 In most cases of cryptogenic stroke associated with PFO, a direct causal mechanism cannot be established between the two. A cause-and-effect relationship can be established only in very rare and specific cases, such as economy-class stroke syndrome (paradoxical embolism secondary to deep vein thrombosis in prolonged air travel), stroke associated with venous thromboembolic disease, some cases of perioperative stroke, or exceptional cases where thrombus is observed in the PFO.6 Although various pathophysiologic mechanisms have been proposed to explain this association, none have been fully accepted. Several clinical scales have been drawn up for more specific differentiation between cryptogenic stroke actually associated with PFO and the presence of PFO as a mere noncausative “spectator,” with RoPE (Risk of Paradoxical Embolism) being the most widely accepted (table 1).7 This scale exhibits good correlation between the patient's clinical characteristics and the risk of PFO-associated stroke (with attributable fraction values between 0% for patients with RoPE scores of 0-3 and 88% for patients with RoPE of 9-10), as well as with the recurrence rate of cerebral ischemic events.
Patient's clinical characteristics and RoPE score calculator
| Characteristic | Points |
|---|---|
| No history of hypertension | 1 |
| No history of diabetes mellitus | 1 |
| No history of stroke or TIA | 1 |
| Nonsmoker | 1 |
| Cortical infarct on imaging | 1 |
| Age, y | |
| 18-29 | 5 |
| 30-39 | 4 |
| 40-49 | 3 |
| 50-59 | 2 |
| 60-69 | 1 |
| ≥ 70 | 0 |
| Total score (sum of individual points) | |
| Maximum score (a patient aged <30 y with no hypertension, no diabetes, no history of stroke or TIA, nonsmoker, with cortical infarct on imaging) | 10 |
| Minimum score (a patient aged ≥ 70 y with hypertension, diabetes, prior stroke or TIA, current smoker, and no prior cortical infarct) | 0 |
TIA, transient ischemic attack.
Modified from Kent et al.7 with permission from Wolters Kluwer and the American Academy of Neurology. Wolters Kluwer Health and its Societies take no responsibility for the accuracy of the translation from the original text and are not liable for any errors which may occur.
Once percutaneous PFO closure became technically possible, a more pragmatic approach was possible when PFO was associated with cryptogenic stroke. The efficacy of the procedure (compared with antithrombotic therapy, mainly aspirin) in terms of stroke recurrence has thus been studied over decades. Several clinical trials with long follow-up periods have shown that percutaneous closure is superior in patients carefully screened to rule out other causes and to include only cryptogenic stroke.8–11 However, these clinical trials only included patients younger than 60 years, who have a much higher incidence of cryptogenic stroke than older patients, with the latter group more likely to have cerebrovascular risk factors.8–10
An interesting article recently published by Wintzer-Wehekind et al.12 in Revista Española de Cardiología analyzed a retrospective series to determine the safety and efficacy of percutaneous PFO closure in patients younger and older than age 60 years. Despite the single-center retrospective design, the study yielded noteworthy data. The series spanned a lengthy period (2001-2018) and included 475 consecutive patients (90 of them older than 60 years) who underwent PFO closure and received follow-up for a number of years. To evaluate the conclusions reached, it is very important to analyze the population included in this kind of retrospective study. In the Wintzer-Wehekind series, the diagnostic workup performed to classify the stroke as cryptogenic was similar to that of recent clinical trials,8–10 and mainly included high-risk PFO (large shunt and/or interatrial septal aneurysm). Vascular risk factors were significantly more common in patients older than 60 years, as usually seen in clinical practice, although they are becoming increasingly more prevalent in young stroke patients.13 However, this study included a very high percentage of patients with transient ischemic attack (TIA) (32.2%). Currently, TIA is diagnosed clinically and is often confused with processes other than cerebral ischemia and, therefore, clinical trials on PFO closure have only included patients with a diagnosis of cerebral infarct established by neuroimaging or with neurologic symptoms lasting> 24 hours.8–10 The inclusion of patients with TIA dramatically lowers the rate of possible recurrence or vascular complications. This is a well-known fact in clinical trials with TIA patients, and lately, only patients with high-risk TIA (according to the ABCD2 scale) or minor strokes are included, in order to prevent the inclusion of “stroke mimics.”
In this single-center study, which reports on extensive experience with PFO closure, the safety data for the procedure were very good, with a low rate of periprocedure complications, a remarkably low presence of residual shunt, and no differences between groups. One of the more notable risks of this technique is the possibility of AF runs in the postoperative period, which would obviously be considered more understandable in an older population. However, this study saw only 1 case of AF, observed in the younger group.12 Waht et al.14 published a series that also reported few complications, but Merkler et al.15 described a high rate of major complications in patients older than 60 years (10.9% vs 4.9%).
During the patient follow-up period, the combined rate of cerebral infarct/TIA was 5.5% in the older group vs 2.6% in the younger group (nonsignificant differences). There were 4 cerebral infarcts, but none were related to PFO. To establish the possible efficacy of closure, the investigators estimated the percentage of stroke recurrence that the older group would have had according to the RoPE scale.7 After analyzing the data, they concluded that the theoretical percentage of recurrence was lower than if the procedure had not been performed.12
In patients younger than age 60 years, neurologists and cardiologists should work together to decide whether PFO closure is indicated for ESUS. For diagnosis, transcranial Doppler plus transesophageal echocardiography can determine the shunt size and morphologic characteristics.16 A meta-analysis has recently shown that PFO closure is most beneficial in patients with large shunts and/or interatrial septal aneurysm. In small PFOs, the benefits of closure are much lower.11
Until clinical trials are undertaken with patients older than 60 years, the diagnostic workup for cryptogenic stroke should be the same as in young patients and should include a study of the PFO to define its characteristics, particularly in patients with no vascular risk factors.1,16 In these cases, cardiology and neurology should cooperate even more closely, as patients at risk of hidden AF (older age, hypertension, or left atrial enlargement) should be monitored for at least 3 weeks.2 Last, this population group should be screened for factors predisposing them to thromboembolic venous disease, such as immobilization, recent surgeries, or thrombophilia.
An important point made by this study was the need to maintain antiplatelet therapy indefinitely. After the procedure, dual antiplatelet therapy is used routinely (3-6 months), with antiplatelet therapy taken indefinitely thereafter. In our opinion, this kind of therapy should not be discontinued because a direct relationship cannot usually be established between PFO and stroke.
The possible role of DOACs in this subtype of stroke is under consideration. The RESPECT-ESUS and NAVIGATE-ESUS studies compared dose-titrated dabigatran and rivaroxaban 15 mg every 24 hours, respectively, against aspirin in preventing the recurrence of ESUS.17,18 The safety results were good in RESPECT-ESUS, but neither study showed that DOACs were superior to aspirin.17,18 These 2 studies included a few patients with PFO. However, the studies were not designed to determine the effect of surgery on PFO, as prior PFO study was not a requirement, nor were data collected on the type of PFO. Therefore, no conclusions can be made on the potential role of DOACs vs aspirin.
Antithrombotic therapy and percutaneous PFO closure are not the only measures to be taken for the secondary prevention of all cerebral infarcts. As mentioned earlier, the presence of risk factors in both populations (young and old) is very common. Although the stroke may have been PFO-related, patients should understand that reducing recurrences requires PFO closure and antiplatelet therapy as well as other standard cardiovascular prevention measures, such as lifestyle changes plus control of blood pressure, low-density lipoprotein levels, and blood glucose concentrations.16 If none of these factors are present, then PFO can be considered to have caused the stroke. Unfortunately, in clinical practice, it is common for many patients to discontinue other preventive measurements after PFO closure, under the mistaken impression that PFO was the sole culprit.
In conclusion, this study provides valuable information on the possible role of PFO closure in patients older than 60 years who have been excluded from clinical trials. Until new trials are conducted specifically in this population subgroup, PFO closure should be reserved for moderate-to-large PFOs with or without interatrial septal aneurysm in recurrent cryptogenic stroke despite optimal medical treatment, after exclusion of other potential causes.19 Another possible subgroup would be patients in whom the stroke exhibited a clear temporal relationship with some of the aforementioned predisposing causes for venous thrombosis.
CONFLICTS OF INTERESTJ. Masjuan has received consulting and speaking fees from Abbott.