We read with interest the Letter to the Editor by Díez-Delhoyo et al. regarding 1 of the patients who died from massive hematemesis, described in our article on percutaneous stent placement to treat coarctation of the aorta due to atresia.1 We would like to make a few points with regard to this case.
This patient received a late diagnosis of coarctation of the aorta with highly developed collateral circulation and an intercostal aneurysm distal to the area of atresia. The case was discussed in a clinical session and a percutaneous approach with selected due to the extremely high surgical risk in these patients, with potentially serious complications.2
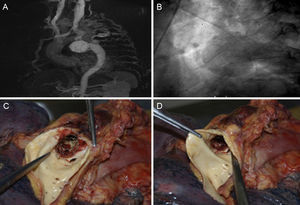
In this patient, the aneurysm was previously under low pressure, given that it was distal to the area of coarctation. In such cases, after the obstruction is resolved, the pressure increases and, unless correct isolation is achieved, there is a higher risk of rupture, as occurred in our patient. Autopsy revealed that the stent had lost its cover, which remained in the delivery sheath due to friction (Figure).
A: magnetic resonance image showing extensive collateral circulation, contrast enhancement of the descending aorta, and a giant intercostal aneurysm. B: late phases of the aortic angiogram show extensive collateral circulation to the descending aorta and a giant intercostal aneurysm. C and D: autopsy image showing loss of the stent cover.
Our group has begun to use a new all-in-one system (Nudel delivery system, Numed) with success in several patients. This system is similar to that used with the Melody pulmonary valve, which increases safety during implantation because it prevents both stent migration and loss of the expanded polytetrafluoroethylene (ePTFE) cover.
On the basis of our experience and a literature review, we conclude that, in this type of coarctation of the aorta with extensive collateral circulation and intercostal aneurysms, the percutaneous approach is the treatment of choice to ensure complete isolation of aneurysms through coil embolization or Amplatzer devices2,3 or the use of covered stents.3 Consequently, preprocedural imaging study with computed tomography or magnetic resonance is essential for an adequate approach in these cases.2,3