The new syncope guidelines significantly increase the volume of information on how to diagnose and manage this entity, which is of considerable importance not only to cardiologists, but also to all physicians involved. A welcome addition is the incorporation of emergency specialists, neurologists, and geriatricians into the working group.
The new document1 comprises 69 pages and 440 references vs the 41 pages and 213 references of the previous guidelines.2 The increase is even greater if one considers the new online section of additional material called “Practical Instructions”. This material includes an extensive glossary that establishes a general vocabulary, a definition of criteria, and a description of techniques and management instructions. This hugely valuable supplement comprises 38 pages and 192 references.
The recommendations continue to operate in an environment of pervasive uncertainty. Quantitatively, the number of recommendations has increased by 7%; however, 40% are level I (49% in 2009) and only 3% are level III (14% in 2009). Neither has the level of evidence changed substantially: only 5% of recommendations are level A (3% in 2009) and most–50%–are level C (52% in 2009).
In addition to specific novel aspects, which are addressed in each section, the role of syncope units (SUs) is emphasized in a commitment to improved patient-focused safety and efficiency. This same commitment is reflected in the definition of the initial evaluation and risk stratification in the emergency department.
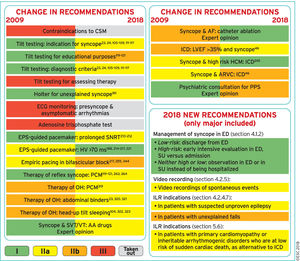
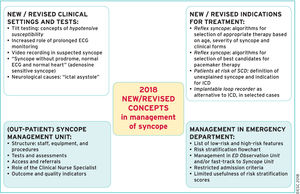
Beyond the specific novelties (Figure 1), we also highlight the conceptual aspects that have been updated and describe them in the same order as the headings of the original document (Figure 2).
What is new in the 2018 syncope guidelines? AA, antiarrhythmic; AF, atrial fibrillation; ARVC, arrhythmogenic right ventricular cardiomyopathy; CSM, carotid sinus massage; ECG, electrocardiogram; ED, emergency department; EPS, electrophysiological study; HCM, hypertrophic cardiomyopathy; ICD, implantable cardioverter defibrillator; ILR, implantable loop recorder; LVEF, left ventricular ejection fraction; OH, orthostatic hypotension; PCM, physical counter-pressure maneuvers; POTS, postural orthostatic tachycardia syndrome; PPS, psychogenic pseudosyncope; SNRT, sinus node recovery time; SU, syncope unit; SVT, supraventricular tachycardia; VT, ventricular tachycardia. Reproduced with permission of Brignole et al.,1 courtesy of the European Society of Cardiology and European Heart Journal, through OUP.
Changes in recommendations between the 2009 and 2018 guidelines. Reproduced with permission of Brignole et al.,1 courtesy of the European Society of Cardiology and European Heart Journal, through OUP.
The definition of syncope is unchanged, although the new document emphasizes the pathophysiological differences from other transient losses of consciousness.
The pathophysiological classification of syncope shows no significant differences from the 2009 guidelines. The guidelines reiterate that reduced cardiac output or peripheral resistance mechanistically underlie the drop in global cerebral blood flow, the defining characteristic of syncope.
The differentiation between reflex syncope, syncope due to orthostatic hypotension, and cardiac syncope is maintained, and the authors of the guidelines stress that several mechanisms can participate in the genesis of a single syncopal episode. The presence of vasodepression, cardioinhibition, or both, bears no relationship to the cause of reflex syncope.
Nonsyncopal forms of loss of consciousness (real or apparent). The types of epileptic seizures involving loss of motor control, as well as psychogenic loss of consciousness and other rare triggers, are briefly described to distinguish them from true syncopal episodes.
DIAGNOSTIC EVALUATION AND MANAGEMENT ACCORDING TO RISK STRATIFICATIONInitial EvaluationEmphasis is placed on a detailed clinical history obtained from patients or eyewitnesses. The history taking has multiple aims: to establish whether loss of consciousness occurred, to determine whether the loss of consciousness was of syncopal origin, to identify its etiology, and to stratify the risk. A novel inclusion is the additional material in the “Practical Instructions”. The recommended diagnostic criteria of reflex syncope, orthostatic hypotension, and cardiac syncope have not undergone substantial changes from the previous guidelines. Helpfully, the guidelines offer practical solutions based on the extensive experience of the members of the ESC working group.
Management of syncope in the emergency department according to risk stratification. One of the most novel aspects of the guidelines is the recommendations for the management of syncope in the emergency department. The main objective of this approach is to reduce the hospital admission rate without compromising patient safety. The guidelines clearly detail the low- and high-risk factors that can be obtained from the clinical history, physical examination, and electrocardiogram. The indications for other complementary examinations are established (hospital monitoring for suspected arrhythmic syncope, echocardiography if there is evidence of structural heart disease, carotid sinus massage in patients older than 40 years of age, tilt-table (TT) testing when there is a suspicion of reflex or orthostatic syncope, and laboratory analyses to rule out secondary causes when required). The authors note that high-risk patients are more likely to have cardiac syncope and, therefore, have a higher risk of sudden death than low-risk patients who, in contrast, are more likely to have reflex syncope and good prognosis.
Not all high-risk patients require hospitalization. The document stresses that SUs are a safe and effective alternative. The guidelines recommend (class I B) that low-risk patients without recurrence be discharged from emergency departments, that high-risk patients be admitted or exhaustively evaluated in emergency departments or SUs, and that patients without high- or low-risk criteria be studied in emergency department observation units or referred to SUs instead of being admitted. Low-risk patients requiring specific treatment (eg, due to multiple recurrences) can be referred to SUs. Risk stratification algorithms are noted to not be superior to clinical judgment in predicting severe short-term events: their use is a class IIb recommendation. A novelty is the equal consideration of presyncope and syncope, introduced because evidence indicates that they have the same prognosis.
The published experience on the implementation of SUs in Spain is scarce,3 although the SEC-EXCELENTE project provides a unique opportunity for the creation of units with specific and homogeneous quality standards.
Diagnostic TestsThere are no changes to diagnostic tests, but a change in “philosophy” is seen with the promotion of the study of dysautonomia as a possible cause of neuromediated syncope. A reasoned step is the incorporation of the neurologist's viewpoint and of neurological tests into the diagnosis and, although to a lesser extent, into the treatment.
Carotid sinus massage. Because it is one of the most cost-effective tests, the guidelines insist that carotid sinus massage be performed in the initial evaluation of patients older than 40 years. There are no changes in the level of indication or in the positive diagnostic criteria (presence of syncope together with ventricular pause> 3seconds or a systolic blood pressure fall> 50mmHg). There is another major consideration: the guidelines no longer deem the test contraindicated in patients with stroke in the previous 3 months or with carotid murmurs. Other considerations deserving comment are as follows:
- •
Carotid sinus massage must be performed first in decubitus and then in orthostatism (usually in the TT, unless the test was already positive).
- •
A somewhat confusing comment is added: carotid sinus massage is indicated for syncope of unknown origin “compatible with a reflex mechanism”. It appears that this statement has been added so that a more serious form of syncope is not diagnosed in a patient with a positive test result.
- •
Greater emphasis could have been placed on the diagnosis of carotid hypersensitivity because its value is supported in the literature.4 The guidelines do mention that asymptomatic pauses exceeding 3seconds (carotid sinus hypersensitivity) have little value in the diagnosis of syncope etiology.
- •
With a positive test result, both components (vasodepressor and cardioinhibitor) must be identified. This requires 2 actions: repeating the test with noninvasive “beat-to-beat” blood pressure measurement after atropine and a TT test. Detection of a dominant vasodepressor component would contraindicate pacemaker (PM) implantation.
Orthostatic challenge. This initial test is basic but cost-effective and has high diagnostic value. Its level of indication has fallen from I B to I C but the classic diagnostic criteria are maintained (I C if syncope occurs during the test and IIa C if there is a significant fall in blood pressure but no syncope). The initial orthostatic intolerance (that occurring <30seconds after the orthostatism) cannot be diagnosed with a sphygmomanometer and a “beat-to-beat” measurement is necessary (IIb C indication). Postural orthostatic tachycardia syndrome (POTS) is precisely defined as an increase in heart rate of more than 30 beats or a rate exceeding 120 bpm with associated symptoms and without hypotension. The definition does not note that the increase should exceed 40 bpm in adolescents, as recommended by the consensus statement on orthostatic hypotension and POTS.5
Tilt-table. The subtlest change in the document is related to this test. Initially, it seems downgraded–as a diagnostic test, its recommendation drops from I B to IIa B–and the diagnostic criteria indication falls from I to IIa. In addition, its lack of ability to direct management is maintained. However, its applications are numerous: vasodepressor component assessment, differential diagnosis (epilepsy, psychiatric syncope), ventricular pause evaluation, prodrome recognition training, research, or videoelectroencephalography. The TT is now considered useful for assessing “hypotensive tendency”. Its usefulness is clear in the context of orthostatic intolerance (either POTS or neurogenic hypotension).
Basic autonomic function testsIf there is suspected orthostatic intolerance, the Valsalva maneuver is awarded a level II indication, in addition to the deep breathing test and other tests. Ambulatory blood pressure monitoring is a class I indication if there is a suspicion of nocturnal hypertension.
Electrocardiographic monitoringIn-hospital monitoring. Immediate monitoring is recommended in high-risk patients (I C), without changes.
A clear recommendation for monitoring time is missing, and the lack of evidence is notable. In another section, a 6-hour emergency department time and a 24-hour hospitalization time are recommended in high-risk patients, without scientific support. This evidence gap is important: a too-short monitoring time can be a risk for some patients, but a too-long time signifies unnecessary resource consumption.
Holter monitoring, event recorders, smartphone applications, and external loop recorders. There are no major changes. Smartphone applications, although innovative, are undermined by their need to be activated by patients before the syncope.
In the case of external loop recorders, the guidelines again apply a class IIa B recommendation for patients with an intersymptom interval less than 4 weeks.
Implantable loop recording. The recommendations remain class I, but with a higher level of evidence, for patients “not at high risk” with recurrent syncope of uncertain origin and a high probability of recurrence during the battery life of the device and for high-risk patients after an exhaustive and unsuccessful investigation.
Emphasis is placed on the usefulness of prolonged monitoring exceeding 3 years. Another notable and widely supported innovation is the early implantation of the device during the diagnostic process. Not only is this approach clinically useful, but it also simplifies patient care and confers significant savings.
The implantation recommendation remains unchanged for patients with confirmed or suspected reflex syncope and multiple or frequent episodes: IIa C.
Two new recommendations with clinical implications are added: for patients with unexplained falls and for patients with suspected epilepsy whose treatment is ineffective. The first recommendation is especially relevant in elderly patients, due to the high prevalence of falls and the diagnostic difficulty. The second is also important: an erroneous diagnosis of epilepsy results in a treatment that is not without adverse effects and leaves the patient improperly treated.
A novelty is the mention of the possibility of remote monitoring, which improves the diagnostic performance by shortening the detection time.
Diagnostic criteria of implantable loop recording findings. The number of recommendations decreases to 2: the findings are diagnostic when there is a correlation between syncope and arrhythmia and when, in the absence of syncope during the recording, prolonged pauses are observed, as well as third-degree or Mobitz II atrioventricular block or rapid tachycardia.
It is presented as advice, and not as a recommendation, that the absence of arrhythmia during syncope rules out arrhythmic syncope and that the presence of significant arrhythmia during presyncope can be considered a diagnostic finding.
Video recording. This technique appears as a recommendation for the first time, in 2 situations. In the first case, for syncope occurring at home, patients and their relatives are encouraged to record the event; relatives should also provide immediate assistance if necessary. Although new technologies (smartphones) enable this approach and it may play a role in diagnosis, there is no clear scientific evidence. In addition, recording can be difficult due to the brevity of most episodes and the emotional context.
The second situation is the use of video recording during the TT test to improve the clinical observation of the events induced. Although class IIb, this recommendation is better documented and more feasible.
Electrophysiological study. The guidelines recognize the reduced diagnostic value of the electrophysiological study (EPS). Its use would be restricted to 2% to 3% of syncopes of uncertain origin. Its limitations include the low negative predictive value and the nonspecificity of the induction of polymorphous ventricular tachycardia or ventricular fibrillation in most structural heart diseases.
It continues to be useful in specific situations such as:
- •
Asymptomatic sinus bradycardia. Recommended when noninvasive tests are unable to correlate the syncope with the bradycardia (new IIb B indication, without basis in new studies). If the corrected sinus node recovery time is prolonged (> 525ms), PM implantation is recommended (IIa B).
- •
Bifascicular block (IIa B, unchanged). If the HV interval exceeds 70ms or there is second- or third-degree atrioventricular block with pacing or pharmacological stress, PM implantation is recommended (I B) (earlier if the HV is 70-100ms (IIa B) and when the HV> 100ms (I B)).
- •
Suspected tachycardia. Without significant changes. In the presence of a previous AMI or other structural heart disease (with a scar-based substrate) with syncope of uncertain origin after a noninvasive study, electrophysiological study has a I B indication.
In syncope preceded by palpitations: a IIb C indication. The electrophysiological study is diagnostic if monomorphic ventricular tachycardia or supraventricular tachycardia is induced that reproduces the spontaneous symptoms or hypotension (I C). Because the usefulness of the electrophysiological study remains controversial in Brugada syndrome with syncope, the previous IIb B recommendation has been withdrawn.
Endogenous adenosine and other biomarkersAdenosine test. The guidelines newly introduce adenosine-sensitive syncope, a type of asystolic syncope seen in patients without prodromes and heart disease and with normal baseline ECG that could be due to endogenous adenosine release.6 The usefulness of the adenosine test to select PM candidates is analyzed: its systematic use is hindered by its low predictive value.
Cardiovascular and immunological biomarkers. The possible future usefulness of biomarkers and autoantibodies for autonomic dysfunction is mentioned, although the authors stress the need for more evidence.
Echocardiography. Echocardiography is still indicated (I B) when there is a suspicion of structural heart disease. The indication for exercise stress echocardiography (I C) is introduced to detect an inducible obstruction in the left ventricular outflow tract in patients with hypertrophic cardiomyopathy and postural or exertional syncope with a gradient less than 50mmHg at rest or after induction.
Stress testing. Same indication as for syncope during or soon after exertion (I C). The difference is emphasized between syncope occurring during exercise (almost exclusively of cardiac origin) and that occurring after exercise (mostly of reflex origin). The diagnostic criteria are maintained for cardiac stress tests (I C).
Coronary angiography. The indication for coronary angiography is the same in both patients with and without syncope (IIa C). The guidelines insist that angiography cannot determine the cause of syncope and that percutaneous intervention is not associated with fewer readmissions for syncope.7
SYNCOPE TREATMENTGeneral PrinciplesThe guidelines maintain the treatment framework based on risk stratification and identification of the specific mechanism when possible. Greater emphasis is placed on the importance of the syncope mechanism to ensure effective prevention of recurrences with treatment.
Clear differentiation of the treatment objectives is missing: to prolong life, to eliminate or diminish the physical (or mental) consequences, and to avoid recurrences. Based on the text, the only evident treatment objective is to avoid recurrence.
Treatment of Reflex SyncopeThe favorable prognosis of this entity and the probability of recurrence are reiterated. The guidelines stress lifestyle recommendations and the identification and prevention of triggering factors as a critical element of treatment. Education is associated with reduced mortality and fewer complications in other cardiovascular diseases.8,9 The novelty here is the introduction of a patient instruction sheet, written for patients and family members, which is highly useful for strengthening health education. The main limitation is the lack of scientific evidence in the area of syncope.
A novel inclusion is a practical and clear schematic on the treatment of reflex syncope. The aforementioned educational measures stand out as the first therapeutic step to be performed in all cases.
The recommendation level of the indication for isometric physical counterpressure maneuvers is reduced (from I B to IIa B). This reduction is due to its low usefulness in the ISSUE-3 trial in elderly patients without prolonged and recognizable prodromes. Because the maneuvers can be useful in young patients with a prolonged prodromal period, they are detailed in the “Practical Instructions”.
The recommendation for tilt training remains class IIb B. It is a potentially useful but impractical approach, and difficult to maintain for a prolonged period, and there is no new relevant evidence.
A new indication is to eliminate or reduce the hypotensive treatment of patients with vasodepressor syncope. This recommendation has clear clinical usefulness because it is highly feasible and there is no deleterious effect on blood pressure control in the studies cited.
The use of the alpha-adrenergic agonist midodrine in patients with vasovagal syncope resistant to educational measures is maintained as a IIb B recommendation, and the class III A recommendation is maintained for the contraindication to beta-blockers.
A new feature is the introduction of fludrocortisone, although it is only useful at high doses and is contraindicated for elderly and hypertensive patients, which is why its usefulness in real-world clinical practice is limited.
Cardiac pacing. Since the last guidelines, substantial evidence has been generated on the efficacy of PMs for the treatment of reflex syncope. In patients older than 40 years, when the mechanism is predominantly cardioinhibitory, dual-chamber PMs (in DDD pacing mode) significantly reduce recurrences. Hence, bradyarrhythmia documentation is fundamental.
Four possible indications are defined, the first 3 for patients older than 40 years: a) documentation of spontaneous bradyarrhythmia (IIa B); b) carotid sinus syndrome with cardioinhibitory mechanism (IIa B); c) asystole induced in the TT test (IIb B); and d) adenosine-sensitive syncope (IIb B).
One controversial aspect, as acknowledged by the authors themselves, is that, for asystole induced in the TT test, the indication for PM implantation is reduced to class IIb and documentation of spontaneous bradyarrhythmia is prioritized. This is despite 2 studies showing that PM implantation significantly reduces recurrences in these patients.10,11
Treatment of Orthostatic Hypotension and Orthostatic Intolerance SyndromesYears have passed but the treatment remains the same and as weakly effective as ever. Only water and salt intake has a class I C indication. There is little evidence of its effectiveness: in the American guidelines, the recommendation is IIb.12 The other usual physical measures have IIa recommendations. Of the drugs, only midodrine and fludrocortisone have a IIa indication. Droxidopa, the only drug besides midodrine to be approved by the FDA, is not recommended, and neither are beta-blockers, in contrast to the American guidelines, which assigns them class IIa and IIb indications, respectively. Appropriately, the guidelines stress that hypertensive elderly people with syncope can be more tolerant of hypotensive treatment.
Treatment of Syncope Due to ArrhythmiasSyncope due to intrinsic sinoatrial or atrioventricular conduction system disease. The indications for PM implantation have not been substantially modified. Two aspects are detailed: a) in patients with sinus node disease without documentation of symptomatic pauses, the recommendation is to rule out other diagnostic alternatives (particularly reflex syncope) before PM implantation in order to reduce the high rate of syncopal recurrences, which is as high as 28% in some series; and b) in patients with syncopes and bifascicular block on ECG, in order to establish the PM indication, the recommendation is to document the pathological findings in an electrophysiological study or via a significant pause on an implantable loop recorder.
Syncope due to tachyarrhythmias. Catheter ablation is the treatment of choice to prevent syncope in patients with supraventricular and ventricular arrhythmias (specifically in susceptible substrates, fundamentally monomorphic ventricular tachycardia).
Two notes are made: a) to individualize the therapeutic option (ablation or drugs) for atrial fibrillation and left atrial flutter (medical therapy was prioritized in previous guidelines); b) to consider implantable cardioverter-defibrillator (ICD) placement after documentation of ventricular arrhythmias in order to reduce mortality in individuals with a left ventricular ejection fraction (LVEF) ≤ 35% (I A) or with previous infarction and induction of tachycardia ventricular (I C). A cutoff point for LVEF is a more specific criterion than the previous, looser, concept of “structural heart disease”.
Syncope due to intrinsic sinoatrial or atrioventricular conduction system disease. To prevent recurrences, the guidelines stress that the focus for these patients should be on treatment of the underlying disease (to improve the prognosis) and not only on the etiological study of the syncope (not always arrhythmic).
Treatment of unexplained syncope in patients at high risk of sudden cardiac death. This section deals with patients with syncope presumably due to ventricular arrhythmias that have not been documented. Therefore, they are “syncopes of unknown origin” that, when occurring in individuals at high risk of ventricular arrhythmias, suggest an arrhythmic origin (“suspected arrhythmic syncope”).
There are 2 options: a) ICD therapy, given that, in this environment, syncope significantly increases the risk of sudden cardiac death; and b) completion of the etiological study (with the intention of documenting the clinical arrhythmia) via placement of an implantable loop recorder in low-risk individuals without an indication for ICD.
The final decision should integrate all of the available information, even though, except for hypertrophic cardiomyopathy, there are no validated risk scales. Thus, the level of evidence for most of the indications is C.
Regarding left ventricular dysfunction, the ICD indications are respected to prevent the occurrence of sudden cardiac death in patients with depressed function, according to the recognized indications. The indication is introduced for patients without an indication in the previous section–which may include individuals with reduced LVEF that exceeds 35%–with a IIa C level. For these patients, an implantable loop recorder can be considered, with a IIB C level.
Surprisingly, the electrophysiological study is not mentioned as a diagnostic tool, despite its proven usefulness in patients with syncope and myocardial infarction. Paradoxically, this recommendation is included in the section dedicated to the electrophysiological study as a I B indication.
SPECIAL ISSUESNo reference is made to elderly patients, but to patients with comorbidities and frailty. This approach is confusing because fundamental aspects of the elderly population are analyzed. Because there is consensus among the authors about the complexity of syncope treatment in the elderly, a multidisciplinary approach is recommended. A novel recommendation is to assess the role of medication (particularly hypotensive and psychotropic drugs). The evaluation must include patients’ general and cognitive physical status, and the diagnostic managements of unexplained falls and of syncope are equated.13
No modification is made to the strategy for pediatric patients. In this setting, syncope is frequent and generally benign. The treatment of pediatric patients with neurally mediated syncope should be based on education and reassurance. No pharmacological treatment is advocated, although some randomized studies have shown a possible beneficial effect of midodrine.14 Neither are other options recommended such as fludrocortisone and PM implantation, which have shown efficacy in small observational studies.
PSYCHOGENIC SYNCOPEThis group of patients was not taken into account in the previous guidelines. This entity is probably underdiagnosed and becoming more relevant.15 Diagnostic keys are proposed and reference is made to video documentation of the episode. As part of the treatment, the somatic specialist must be the physician who explains the nature of the condition to the patient.
NEUROLOGICAL CAUSES AND “PSEUDOSYNCOPES”Neurological ExplorationsNeurological evaluation has a class I C indication if there is autonomic failure or suspected epilepsy. Epilepsy is probably the most difficult differential diagnosis of syncope and is thus widely discussed in the guidelines. Of particular importance for cardiologists is “ictal asystole” in the context of partial seizures because their final treatment, in addition to antiepileptic drugs, may include PM implantation. Fortunately, it is a very rare condition and should not be confused with sudden death in epileptic patients (typically occurring in patients after nocturnal generalized tonic-clonic seizures). There is a brief mention of other diseases such as stroke, migraine, cataplexy, and drop attacks.
The authors stress that electroencephalography, Doppler imaging of the supraaortic trunks, and brain computed tomography or magnetic resonance imaging (MRI) are not indicated for syncope (class III B recommendation). However, importantly, in contrast to the previous guidelines, brain MRI (I C) is recommended in patients with signs of parkinsonism, ataxia, or cognitive impairment. Electroencephalography is only useful in doubtful cases or to establish the diagnosis of psychogenic syncope if an induced episode is recorded. A novelty is the recommendation (I B) for paraneoplastic antibody screening (and active searching for occult neoplasia if positive) and antiganglionic acetylcholine receptor antibodies in patients with acute or subacute onset of autonomic dysfunction. A diagram is proposed for the explorations to be performed on patients with autonomic dysfunction that indicates imaging tests, skin biopsy, and even genetic tests depending on the clinical presentation. Additional information on the interpretation of these examinations is provided on the web.
ORGANIZATIONAL ASPECTSOrganizational factors focus on the concept of the SU, taking as reference the consensus document published by the ESC in 2015,16 which proposed the model.
For the first time, a clear definition of the SU is established and the concept of a “syncope specialist” is defined. Previous guidelines emphasized the need for a collaborative multidisciplinary model. Now, the focus is on the presence of at least 1 physician “specialized” in syncope who leads the process.
The SU may be either a physical or virtual entity but must have dedicated staff and their own diagnostic and therapeutic resources. The need for quality assurance of the units through the measurement and control of specific indicators is established for the first time.
It is worth remembering that the proposed SU is based on the consensus of the authors. The standardized care of patients with syncope reduces unnecessary testing and hospitalization. Although this unit is based on objective data, the evidence that a SU improves health care is weak. Because it has not been clearly shown that one model is better than the other, the units must adjust to the characteristics and resources of each specific environment. The only SU model supported by a randomized study is that of the SEEDS study by the Mayo Clinic17 for the treatment of patients with syncope of unknown cause and of intermediate risk in the emergency department. This unit is the only one accepted by other scientific societies and, although mentioned in the section on syncope care in the emergency room, it is not discussed by the authors in the context of the SU.
CONFLICTS OF INTERESTNone declared.
SEC Working Group for the 2018 ESC Guidelines for the Diagnosis and Management of Syncope: Fernando Arribas, Gonzalo Barón-Esquivias, Blanca Coll Vinent, Felipe Rodríguez Entem, Jesús Martínez Alday, Ángel Martínez Brotons, Núria Rivas Gándara, and Javier Jiménez Candil.
Expert Reviewers for the ESC Guidelines for the Diagnosis and Management of Syncope: Ricardo Ruiz Granell, José Miguel Ormaetxe, José Luis Merino, Rafael Peinado, Ángel Moya, Pablo Díez Villanueva, Clara Bonanad, Héctor García Pardo, Jorge Toquero, Felipe Atienza, and Xulio Beiras.
SEC Guidelines Committee: Fernando Alfonso, Borja Ibáñez, Fernando Arribas, Gemma Berga Congost, Héctor Bueno, Arturo Evangelista, Ignacio Ferreira-González, Manuel Jiménez Navarro, Francisco Marín, Leopoldo Pérez de Isla, Antonia Sambola, Rafael Vázquez García, and Ana Viana Tejedor.
.