Keywords
INTRODUCTION
In recent years, there is growing interest in the problems caused by oxidative stress in numerous medical procedures.1-4 One such case, for example, is cardiac surgery,5 in which cardiopulmonary bypass can affect nearly all the organ systems, provoking lesions of varying degrees of severity. This injury is due, at least in part, to the phenomenon of "ischemia-reperfusion"; that is, both the interruption and the subsequent restoration of the blood flow that can have deleterious effects.6-11
Surgically induced myocardial ischemia, although transient, provokes the release of potentially toxic oxygen free radicals as part of a complex inflammatory cascade that progresses toward the site of the tissue injury,5,12-17 triggering complications as it develops.11,12 To combat the oxidizing or toxic effect of these free radicals, the organism launches a series of defensive (antioxidant) mechanisms that may or may not be effective or sufficient. Thus, the phenomena of oxidative stress are determined by the imbalance between oxidants and antioxidants, due either to an increase in the production of the former or to an inadequate neutralization on the part of the latter.1,2,5,18,19
On the other hand, improvements in anesthetic and surgical techniques are continually being introduced in the attempt to prevent or reduce the deleterious effects of the pump employed in cardiopulmonary bypass (CPB). In this context, cardiac surgery without CPB is becoming increasingly widespread, with very promising results in terms of morbidity and mortality,20-22 probably because it is associated with lower levels of oxidative stress.23 However, there are few studies comparing the two surgical techniques and providing a basis for this assumption.15,16,22,24-28
To estimate the damage associated with each type of cardiac surgery, the direct measurement of markers of oxidative stress (lipid peroxidation)5,16,18,19,29 and the analysis of antioxidant defense30-35 are equally valid approaches. This report deals with the comparative analysis of the phenomena involved in oxidative stress during cardiac surgery with and without CPB. For this purpose, we assessed an antioxidant system, the glutathione complex, which acts as an "interceptor," that is, it reacts directly with the free radicals to impede their action. The determination of glutathione concentrations provides information on its deposition in cells (erythrocytes) and plasma, as well as on the functional status of said system.
PATIENTS AND METHOD
Patients and Anesthetic Technique
In this study, we analyzed 19 cardiac operations performed in our hospital between October 2001 and September 2002. Cardiopulmonary bypass was employed in nine cases (47.4%) and all of the procedures were elective. Since the choice of the technique to be used was always made by the surgeon responsible for carrying it out, it was not possible to randomize the 2 groups; however, inclusion in the study was random (it is to be supposed that the number of operations during that period of time was much larger). The clinical characteristics of the patients are summarized in Table 1. All of them presented a contractility of more than 45% (mean ± standard deviation [SD], 61.5±8.6%) and stenosis of at least 2 coronary arteries. The antianginal therapy was the maximum tolerated by each patient and none of them presented comorbidity of interest.
The anesthetic technique always consisted of:
- Premedication with scopolamine and morphine in the hospital ward.
- Induction with etomidate, midazolam, and fentanyl.
- Maintenance on controlled mechanical ventilation with fentanyl, anesthetic gases (sevoflurane for off-pump procedures and isoflurane for on-pump surgery), and nondepolarizing muscle relaxants like atracurium or cisatracurium. Aprotinin, at a dose of 2 000 000 units, was utilized in all the procedures involving CPB.
- Immediate postoperative period: all the patients were unconscious and on mechanical ventilation upon arrival in the recovery room and were maintained in that state until the anesthetic drugs had been metabolized, after which they were extubated if their hemodynamic and respiratory statuses were satisfactory.
Seven blood samples were obtained at different time points during the operation and the immediate postoperative period (Table 2).
Sample Processing
Determination of Glutathione Concentrations
Total glutathione (TG) and oxidized glutathione (GSSG) were determined by spectrofluorometry (Hissin and Hill technique, 1976). Via mathematical fitting of the data (for a 1:5 dilution), we obtained:
and the results were expressed in µmol/erythrocyte hemoglobin.
Reduced glutathione (GSH) was calculated as TG minus GSSG, and the percentage of GSSG was determined using the equation:
(% GSSG=[GSSGx100]/[GSH+GSSG])
Determination of Glutathione-Related Enzymatic Activity
This determination provides information on the capacity of the system to react to a possible injury. Kinetic spectrophotometry was employed to analyze the 3 major enzymes involved in glutathione balance (Table 3).
Statistical Analysis
The statistical analysis was done using the SPSS (Social Program for Statistical Sciences) software package for Windows 98, version 9.0 (SPSS Inc., 1999). The results reported in the text, tables, and figures are expressed as the mean ± standard deviation (SD).
Once the homoscedasticity (equality of variance) of the groups was established, one-way ANOVA was used for the comparison of the means obtained in the different samples, followed by intergroup comparison to detect significant differences. P<.05 was considered to indicate a statistically significant difference. The corresponding association coefficients were also calculated to enable the determination of the potential influence of clinical, epidemiological or surgery-related factors.
RESULTS
Patients
All the procedures involved conventional complete revascularization and included the left anterior descending coronary artery. We obtained as many grafts as possible from the 2 mammary arteries, occasionally using the radial artery as well. The results are summarized in Table 1. The partial ischemia times for the shunting of each artery were not recorded in the group that did not undergo CPB. In one of these patients, carbon dioxide laser was also employed during the procedure and, in 6 of those who underwent CPB, concomitant valve replacement was performed.
The incidence of major complications was similar in the 2 groups and was easily resolved in most cases. One patient died 13 days after undergoing surgery without CPB; he had small native coronary arteries and basal left ventricular dysfunction (with an ejection fraction of 46%), and presented perioperative acute myocardial infarction owing to the poor quality of the grafts. The overall mean length of stay in the recovery room was longer in the group without CPB (5.0±3.1 days vs 3.7±1.1 days), although if we exclude the patient who died, the difference between the 2 values is less marked (4.1±1.4 days vs 3.7±1.1 days).
Sample Analysis
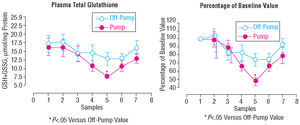
The 2 groups differed with respect to the plasma TG concentration (Figure 1). Although the initial levels were similar (16.2±2.6 µmol/min in the CPB group vs 17.2±2.4 µmol/min in the group without CPB), that of the CPB patients decreased progressively until the moment of reperfusion, when the maximal inhibition was reached (sample 5). This trend was noted in the off-pump patients, but was less marked. The reduction in TG may indicate an impairment of the antioxidant defenses of the CPB patients, or could be attributed to the depletion of glutathione in the attempt to offeset the peroxide overproduction provoked by the surgical procedure.
Figure 1. Changes in plasma total glutathione. Both the absolute values (left) and percentages of the baseline value (right), expressed as mean ± standard deviation, exhibit a differential behavior, with a more marked depletion in the CPB group until the initiation of reperfusion (sample 5), and recovery in both groups by the next day, although this recovery is incomplete in the CPB group. CPB indicates cardiopulmonary bypass.
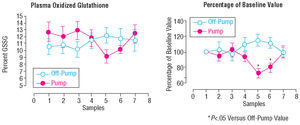
To clarify this issue, we determined the percentage of TG that corresponded to GSSG and the percent change with respect to the baseline value (Figure 2). The plasma GSSG increased in the off-pump patients, whereas it decreased in the on-pump patients.
Figure 2. Changes in plasma oxidized glutathione expressed as mean ± standard deviation of the absolute values (left) and percentages of the baseline value (right). The trend is similar to that of total glutathione: increasing in patients without CPB, reflecting an effective antioxidant defense, and decreasing in patients with CPB due to the inability to withstand the surgical injury. CPB indicates cardiopulmonary bypass; GSSG, oxidized glutathione.
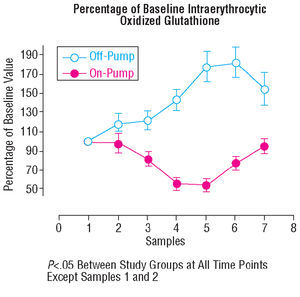
The same analyses were performed to assess the intraerythrocytic glutathione (Figures 3 and 4) with results similar to those obtained in plasma. Both determinations revealed a trend toward decreased levels in the CPB group. On the other hand, in the off-pump group, there was an increase in glutathione oxidation that did not result in the depletion of the total content.
Figure 3. Percentage of intraerythrocytic total glutathione, expressed as the mean (± standard deviation) of the absolute values (left) and the percentages (right). Both values increase during ischemia in patients without CPB, exhibiting the opposite behavior in patients with CPB (see text). CPB indicates cardiopulmonary bypass; GSH, reduced glutathione; GSSG, oxidized glutathione.
Figure 4. Percentage of intraerythrocytic oxidized glutathione, expressed as the mean ± standard deviation. This value increases in the group without CPB, and shows a marked decrease during ischemia in patients with CPB. CPB indicates cardiopulmonary bypass.
The behavior of the enzymes related to this system was analyzed (Table 4). There were no significant changes in the glutathione peroxidase (GSHpx) or glutathione transferase (GSHtf) activity during surgery; in contrast, a reduction was observed in the glutathione reductase (GSSGrd) activity, a circumstance that may be interpreted as an attempt to maintain glutathione in the oxidized form (for better defense). There were no significant differences between the 2 groups, although the trend toward a decrease in GSSGrd was slightly more marked in the on-pump patients.
Finally, the association coefficients calculated for a history of infarction and for combined surgery and the correlation coefficient for the ejection fraction were not significant.
DISCUSSION
Surgery involving the myocardium almost unavaoidably provokes an increase in the general markers of inflammation and in other specific parameters, such as the MB (muscle/brain) isoenzyme of creatine kinase (CK-MB) or troponin.5,16,17,23,25-28,36 These findings are common to all cardiac surgical procedures, even in uncomplicated cases and in the absence of evidence of myocardial infarction.17,37 In a generic sense, the intensity and characteristics of this response can depend on the type of surgery (with or without CPB) and, theoretically, it is more intense in those cases in which CPB is employed14,16,25-27,36; in fact, in the earliest publications, a greater expression of plasma markers of myocardial injury was reported in patients undergoing on-pump surgery.17,36 However, in later studies,23,25 the inconsistent results obtained invalidated them as dependable indicators of myocardial injury and made it necessary to search for other more reliable ones. This gave rise to the interest in measuring oxidative stress and antioxidant defense, since their status affects patient outcome and the development of potential complications.11,15,19,21,38
To date, the largest body of published information on the phenomena associated with oxidative stress in cardiac surgery19,22,38 and, particularly, that concerning antioxidant defense, deals with procedures involving CPB, and not only because of the long history of this approach. The explanation for these changes appears to be quite straightforward since the CPB circuit involves aortic clamping (and, consequently, cardiac ischemia), mechanical injury to the blood elements, hypothermia with cardioplegic arrest and the substitution of pulsatile blood flow by unphysiological, low-pressure continuous flow. Under these circumstances, oxygen free radicals are released,5,6,8,10,13,17 while other parameters of inflammation increase. Moreover, elevated plasma and intraerythrocytic concentrations of oxidation products are observed,18,29 as is an increase in the enzymatic activity involved.19,34,35 Another finding is that the oxidative changes take place according to a clear time sequence throughout the ischemia time,18,29,35 reaching a critical point precisely at the start of reperfusion.8 Moreover, while lipid peroxidation returns to normal the morning after the operation,17,19,29 antioxidant defense remains suppressed29,39 or, at least, presents lower values than the oxidation parameters, a circumstance that leads to manife st damage that exhausts the defense systems.
With regard to the enzymatic activity involved, the information in the literature is widely discrepant,34-36 making it impossible to define patterns of more or less deleterious behavior. The behavior of GSHpx is usually stressed.19,28,30,31 In any case, in our series, none of the enzymes analyzed underwent important modifications, a circumstance that we attribute to the small sample size.
On the other hand, in off-pump operations, the mechanism of ischemic injury is not as clear. Theoretically, when the pump is obviated, all its effects are avoided40; aortic clamping, cardioplegic arrest and continuous flow are not employed and, thus, the ischemia-reperfusion phenomenon could be confined to each artery, which is "stabilized" when it is about to be revascularized, meaning that, a priori, there should be less damage. In contrast, the manipulation and rotation of the heart to gain access to and implant shunts in the coronary arteries situated on the posterior and lateral aspects of the heart may lead to torsion of the vascular pedicle, causing considerable ischemia which counteracts the benefits. Moreover, there is too little scientific evidence supporting the superiority of one option or the other. What does appear to be clear is that the damage is less severe24,25,41 and the antioxidant defense is not as impaired or, at least, is not overwhelmed by the oxidative agents. Consequently, the morbidity and mortality associated with this procedure is reduced.26,27,41
Our results agree with this analysis of the situation and outline differences in favor of off-pump surgery in that the bypass induces the formation of vast numbers of free radicals that ultimately overwhelm the antioxidant systems and result in a situation of oxidative stress, whereas off-pump procedures permit a more active and effective antioxidant defense (Figures 1-4). Although our data on lipid peroxidation have yet to be published, they correlate with the findings of the present report (more intense peroxidation in the CPB group). On the one hand, the plasma TG and GSSG levels demonstrate that the patients with CPB did not have an effective antioxidant defense (defined as the transformation of the reduced form into the oxidized form). On the other hand, glutathione depletion was less marked in off-pump surgery than in interventions involving CPB; moreover, the glutathione consumed was used in an active antioxidant defense. Thus, the patients who undergo off-pump surgery present a better plasma antioxidant profile than those subjected to CPB. Likewise, the reduction of the eythrocyte antioxidant concentration in patients with CPB reflects the inefficiency of this antioxidant system, whereas its enhancement in patients without CPB clearly indicates an active antioxidant defense against the production of free radicals.
Meanwhile, the attempt has been made to attribute the differences observed in the oxidative status in the 2 types of surgery to different external conditions.3 A number of authors have attempted, with varying degrees of success, to relate the severest inflammatory responses and the development of complications with factors like smoking, alcohol consumption, age,3,4,42,43 left ventricular systolic dysfunction,43,44 poorly controlled diabetes,3,45,46 the extension of ischemic heart disease,47 or hemodynamic instability at the start of surgery.48 It is generally accepted that a thorough preoperative risk assessment enables the correct estimation of the morbidity and mortality.49-51 In any case, the more markedly reduced contractility in patients without CPB would lead us to expect worse results in terms of antioxidant defense,43,44 but this assumption contrasts with our findings, a circumstance that suggests that we should seek an explanation directly associated with the operation.
With respect to surgical factors, in our case, we rule out the potential influence of the anesthetic management, as it was the same in all the patients. In almost all certainty, the duration of ischemia and of CPB are the most evident differentiating factors and probably the only ones that can be easily justified. There is evidence of positive correlations between CPB time and the release of oxygen free radicals and the postoperative CK-MB concentration,5 and between longer CPB times and higher complication rates.43 All in all, the differences observed are best explained by the characteristics of each of the 2 procedures, the mechanisms of injury, which have been discussed here. Although it is certain that we have not recorded the partial ischemic times, it seems logical that the sum of the partial times in the group without CPB will be less than the time required for operations with CPB. On the other hand, there are contradictory reports in the literature with regard to valve surgery although, in our case, in contrast to what we had expected, combined surgery per se was not associated with a less effective antioxidant defense, nor did these patients have a comparatively poorer outcome.
Finally, we point out 2 essential limitations of this study. The first is the small sample size. A larger number of patients would probably enable us to accentuate the differences observed (although in some aspects, they are significant as is) and would dilute data such as the mortality in which, while there was only one case, it elevated the incidence to 10% of the group to which the patient belonged. For this reason, we do not consider the morbidity and mortality rates recorded to be discouraging, since many of the adverse events were rapidly resolved. This circumstance is reflected in the length of stay in the recovery room, which was shorter than the average of four to 5 days registered in Spain in recent years.43
The second limitation is the paucity of information on the course following discharge from the recovery room. We consider that this matter should be addressed in another study, and prefer to limit this analysis to the surgical procedure and the immediate postoperative period.
CONCLUSIONS
In our series, we observed differences involving the behavior of the glutathione system in that the patients who did not undergo CPB presented a better antioxidant profile. This may indicate that off-pump cardiac surgery is less damaging to the myocardium.
Correspondence: Dra. A.M. Montijano.
Avda. Dr. Fleming, 4, 2.°. 14004 Córdoba. España.
E-mail: amontijano@medynet.com