To the Editor:
Spontaneous coronary artery dissection (SCAD) is a rare, probably underdiagnosed cause of acute coronary syndrome and sudden death that mainly affects young, previously healthy patients. The etiology of this condition is still uncertain, and the limited evidence regarding treatment is based on clinical case descriptions and retrospective analyses.
We describe the case of a 36-year-old woman with no cardiovascular risk factors or other relevant history who consulted for chest pain of 1 h duration. An electrocardiogram done by an out-of-hospital emergency service showed ST elevation in I and aVL, a reciprocal decrease in the inferior leads, and hyperacute T-waves at V4 through V6. After antiplatelet, anticoagulant, and nitrate therapy, the elevated ST normalized and the patient arrived at the hospital asymptomatic. The left ventricular ejection fraction (LVEF) was severely depressed (30%) due to extensive anterolateral akinesia. Scheduled coronary angiography 48 h later showed coronary arteries with no atherosclerosis, and a slight loss of diameter in the proximal and middle segments of the left anterior descending artery (LAD). Intravascular ultrasound (IVUS) revealed an intramural dissection and hematoma affecting the LAD (minimum lumen area, 3.78 mm2) and the left main coronary artery (LMCA) (minimum lumen area, 7.5 mm2) (Figure 1). There was no evidence of intimal rupture. Based on the patient's stable status and TIMI III flow, observation was decided, with continuation of medical therapy and hospital monitoring and angiographic follow-up a few days later. Coronary angiography and IVUS at 18 days showed reabsorption of the intramural hematoma and sealing of the LAD and LMCA dissection (Figure 2). Echocardiography done before discharge showed normalization of the LVEF and contractility in the previously affected regions, except for mild apical hypokinesia. The hormone, autoimmune, and pregnancy studies were negative.
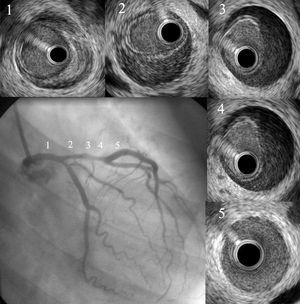
Figure 1. Coronary angiography and intravascular ultrasound 48 h after admission. Intramural dissection and hematoma are seen between the middle segment of the left anterior descending artery and the proximal left main coronary artery.
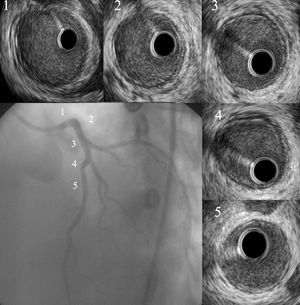
Figure 2. Coronary angiography and intravascular ultrasound at 18 days postadmission revealed spontaneous closure of the dissection and reabsorption of the intramural hematoma.
More than 250 cases of SCAD have been described, particularly in young pregnant women (80%) around the time of delivery or in relation to the use of contraceptives. It is unquestionable that the prevalence is underestimated, due to false negative results of the coronary angiography, spontaneous closure of the dissection, and presentation as sudden death. Sudden death is a common manifestation, in which the condition is diagnosed during the autopsy. Survivors may present angina or myocardial infarction, which usually affects the LAD, although it has been simultaneously described in multiple vessels and in the LMCA in 20% of cases.1-3
The etiology and pathogenesis of this condition are uncertain. In the absence of intimal rupture, vasa vasorum bleeding and subsequent hemorrhaging in the tunica media have been proposed as a possible underlying mechanism. Expansion of the hematoma and false lumen compresses the true lumen and leads to myocardial ischemia. Periadventitial inflammatory infiltrates with eosinophils and cystic necrosis of the tunica media have been described in some cases.4 Propagation of the dissection may occlude major branches and form pseudoaneurysms.
No optimal treatment has been established for SCAD, and the limited number of patients precludes definitive conclusions. Stable patients with limited dissections tend to have spontaneous closure and favorable long-term results with conservative treatment. The use of thrombolytics as first-line therapy has been avoided because of the possibility of extending the dissection. Although surgery has been recommended for dissections affecting the LMCA, its limitations are difficulty finding the true lumen and nonnegligible mortality.5 Spontaneous LMCA dissections successfully treated by stents have also been reported.6 However, this procedure is associated with complications, such as difficulties when advancing the guidewire through the true lumen, proximal and distal progression of the dissection, and acute closure of the vessel.
In our case, intravascular ultrasound was essential for both the diagnosis and follow-up. The option of conservative management was taken because of the patient's stable status over the previous 48 h, adequate TIMI flow, and absence of intimal rupture or severe stenosis in the main coronary artery.
Although new dissections are common in the same or a different coronary artery in the months after the initial event, patients who survive hospitalization have a good long-term prognosis.7 Our patient has remained asymptomatic for the 6 months since admission.