To the Editor:
Percutaneous coronary intervention has displaced revascularization surgery in increasingly complex cases. At times, this requires longer procedures and the use of larger doses of contrast. The principal problem arising from these situations is the nephrotoxic effect of the contrast material, whether ionic or non-ionic,1,2 and neurological complications as striking as the one we present here have also been recorded.
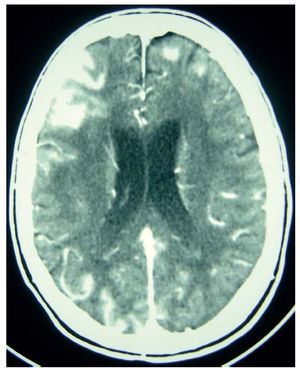
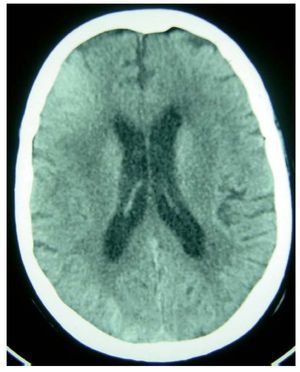
We present the case of a 70-year-old woman, with a personal history of arterial hypertension and degenerative aortic valve disease with mild stenosis and normal ventricular function, who was admitted electively to undergo cardiac catheterization because of recent onset effort angina. Renal function was normal (creatinine base value, 1.1 mg/dL; clearance, 46.21 mL/min/1.73m2). The cardiac catheterization showed diffused coronary artery disease with poor distal beads that had undergone partial percutaneous revascularization; a second intervention was pending. Due to technical difficulties, the procedure was lengthy. A conventional ionic contrast material was used, given the absence of signs of renal insufficiency at the time of catheterization. It was necessary to use 1500 mL of contrast material, for which reason, following the intervention, intravenous N-acetylcysteine and abundant hydration with physiological saline (100 mL/h) were administered to prevent nephropathy due to the contrast. The patient was admitted to the cardiac ward for observation. Upon arrival, she experienced a convulsive episode, which subsided spontaneously after 3 minutes. Following the episode she was conscious and aware, with no evidence of neurological focality or stiff neck. Likewise, there was no headache. Analysis showed no ionic alterations and the glycaemia level was normal. An urgent cranial computed tomography (CT) was performed (Figure 1), which showed hyperdensity of cerebral sulci, fundamentally in the right frontal area, indicative of a diffuse subarachnoid haemorrhage, without an apparent source of bleeding. No dilation, intraventricular haemorrhages, or focal parenchymal lesions were observed. The patient experienced myoclonus which subsided with diazepam, and the cranial CT was repeated 24 hours later (Figure 2), with practically normal results. The rapid resolution of the CT findings and the absence of neurological antecedents and after-effects point to the neurotoxicity of the contrast material as the most probable cause.2
Figure 1. Cranial CT without contrast: axial view of lateral ventricles showing hyperdensity of the cerebral sulci that are most noticeable in the right frontal area, compatible with a subarachnoid space haemorrhage.
Figure 2. Control cranial CT: discrete hyperdensity in the right frontal area.
Given a patient with a neurological episode following cardiac catheterization, the most frequent aetiology is ischemia3; however, as this case indicates, neurological complications caused by the contrast have been described. Although they are infrequent, it should be known that they include convulsions,4 cortical blindness,5,6 and transitory general amnesia.7,8 The aetiology remains unclear, but it has been theorised that the most likely mechanism is the osmotic rupture of the blood-brain barrier,2,5,7 which would permit contrast material to reach the subarachnoid space, where it would directly affect neuronal stimulation and excitation.1
Before carrying out the angiography, it is necessary to identify those patients with the highest risk of suffering toxic effects, the most frequent of which is nephropathy. In addition, any recent history of convulsions, asthma, or known allergies should be analysed. Elderly patients, with a previous history of renal insufficiency or diabetic nephropathy, or those in unstable condition, are at greater risk for toxicity.9 In this way, hydration is recommended for all patients before receiving the contrast injection, as is the use of non-ionic or low-osmolar contrast, which reduces the risk of an adverse reaction.10
This case teaches us that, having ruled out ischemia, some neurological symptoms following cardiac catheterisation may be due to contrast-induced toxicity. This diagnosis can be confirmed in the case of rapid resolution of the neurological symptoms and CT hyperdensity findings.