Patients with type 2 diabetes and revascularized coronary disease are a group with very high cardiovascular risk that has been rarely studied. This ICP-Bypass substudy analyzes the clinical characteristics and risk factor control of these patients.
MethodsThe analysis selected patients with type 2 diabetes who had participated in an earlier multicenter, observational, cross-sectional study (ICP-Bypass) conducted in 2293 patients > 18 years of age who had undergone coronary surgery or percutaneous coronary intervention. Demographic and therapeutic variables, as well as clinical and analytical parameters, were collected and comparatively analyzed.
ResultsThe mean age (standard deviation) of the 771 diabetic patients included in the analysis was 67.7 (9.6) years (71.4% men; mean time since revascularization, 3.5 years). Most (57.8%) were receiving treatment with oral hypoglycemics alone, whereas 30.4% were receiving insulin alone or in combination. The mean glycohemoglobin figure was 7.1% (in 70%,<7.5%); 74.8% had been diagnosed with dyslipidemia. Mean low-density lipoprotein cholesterol was 93.5mg/dL (in 73%, > 70mg/dL). Among these patients, 93.6% were receiving statins and 18.7% a statin combined with ezetimib. A total of 78.1% had been diagnosed with hypertension; systolic/diastolic blood pressure was < 130/80mmHg in 52% and < 140/90mmHg in 93%.
ConclusionsCardiovascular risk and prevention may be improved in revascularized diabetic patients in Spain through further control of risk factors, particularly dyslipidemia. Patients with glycohemoglobin > 7.5% should be individually assessed in terms of glycemic targets.
Keywords
Patients with ischemic heart disease who have diabetes mellitus (DM) are a group at increased cardiovascular risk.1,2 According to the latest guidelines on cardiovascular prevention and DM, prediabetes, and cardiovascular disease published by the European Society of Cardiology, patients with type 2 DM (DM2) are considered to be at high to very high cardiovascular risk—similar to patients with acute coronary syndrome or disease—if they also have a history of cardiovascular disease or other associated risk factors.3–5 Therefore, patients with DM and ischemic heart disease are at very high risk and have a high prevalence of dyslipidemia and hypertension.6 Additionally, DM is associated with a more atherogenic lipid profile, due to the smaller, denser low-density lipoproteins than those found in nondiabetic patients and lower high-density lipoprotein cholesterol (HDL-C) concentrations, which may contribute to increased cardiovascular risk in these patients.7
The various clinical guidelines and consensuses recommend a multifactorial approach toward the diabetic patient that considers both glycemia and all other related risk factors, in order to minimize macrovascular and microvascular mortality and morbidity, as observed in the Steno-2 study.8,9 However, the target for each risk factor should be individualized in some cases. Intensive pharmacological interventions aimed at lipid management and control have been shown to help lower cardiovascular risk in high-risk patients, regardless of the degree of control achieved.10 In particular, a sharp drop in low-density lipoprotein cholesterol (LDL-C) has been shown to lower the rate of cardiovascular events in diabetic patients by 21%.11 Unlike lipid intervention studies, however, the concept of “the lower, the better” is ruled out in hypertension control due to the presence of the J-curve. In the case of glycemic control, the strictness of the target depends on patient age, functional status, and comorbidities.12,13
The ICP-Bypass study investigated the characteristics and residual risk in a population of patients with ischemic heart disease (for the purposes of the study, patients with a history of coronary revascularization).14 Because these DM patients are at very high risk according to the European Society of Cardiology Guidelines3,4,15 and there are few data on risk factors in the diabetic population with a history of coronary disease who have undergone surgery revascularization or percutaneous coronary intervention, the aim of this study was to investigate and describe the characteristics of patients with DM2 in the ICP-Bypass study, including the impact of chronic renal failure and the presence and degree of control of other associated risk factors.
METHODSThe ICP-Bypass study has already been described in detail.14 The study was conducted in the second quarter of 2009, and each of the 199 participating investigators included the first 14 patients who underwent revascularization (bypass or percutaneous coronary intervention>3 months earlier) and came for follow-up at cardiology outpatient clinics in hospitals or health care centers in Spain. At the inclusion visit, patients signed their informed consent, completed a study-specific questionnaire to collect age, weight, height, waist circumference, and blood pressure (BP) at the time of the visit, as well as the presence of cardiovascular risk factors and laboratory parameters: HDL-C, LDL-C, triglycerides, glycohemoglobin (HbA1c), and creatinine in the previous 3 months. Current medical treatments related to risk factor management and control were also collected.
For the present analysis, the variables were retrieved from the main study database and patients were selected if they had been diagnosed with DM2 according to the medical history, were receiving at ≥1 oral antidiabetic (OAD) agent, or had HbA1c>6.5%. Patients were considered to have hypertension or dyslipidemia if the diagnosis had been previously recorded in the medical history. For LDL-C, these post-hoc analyses assumed a therapeutic goal < 70mg/dL, in accordance with the latest guidelines published after the initial analysis.3,15 Controlled BP was established as < 140/90mmHg. The MDRD-4 (Modification of Diet in Renal Disease-4) formula16 was used to calculate the eGFR (estimated glomerular filtration rate) from the recorded variables and to define the presence or absence of chronic renal failure as a possible risk-modifying factor. Chronic renal failure was considered to exist if eGFR < 60mL/min/1.73 m2, which corresponds to chronic kidney disease stages 3 to 5.
Statistical AnalysisThe qualitative variables were evaluated by the ¿2 test and the quantitative variables by Student t test and analysis of variance; only valid data were included, and missing data were not allocated. P values < .05 were considered statistically significant. No adjustments were made for multiplicity, and no interim analyses were performed. No inferential analyses were performed with variables that had qualitative or binary answers. The analysis was performed using SPSS version 18.
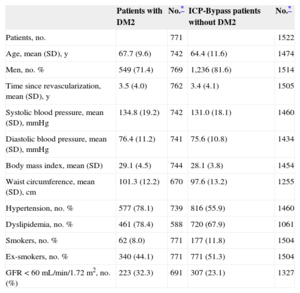
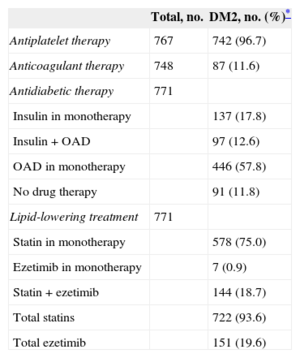
RESULTSThe ICP-Bypass study population that met the inclusion criteria consisted of 2292 patients, of whom 771 (34%) had DM2. Among these 771 already revascularized diabetic patients (mean time since revascularization, 3.5 years; median, 1.90 [3.96]; Q=0.55; Q3=5.08 years), a total of 32.3% had renal failure (eGFR < 60mL/min/1.73 m2), and the mean eGFR was 71.5mL/min/1.73 m2. The patient characteristics are summarized in Table 1. The main differences compared with the total population for the main study were a lower percentage of active smokers (8.0% vs 51.3% of the total population) and a higher prevalence of hypertension (78.1% vs 55.9%) and renal failure (32.3% vs 23.1%). A total of 96.7% patients were receiving antiplatelet agents, 93.6%, a lipid-lowering agent, and 88.2%, drug therapy for DM (Table 2).
Characteristics of Patients with Type 2 Diabetes Mellitus Included in the Analysis and of the Nondiabetic Population
| Patients with DM2 | No.* | ICP-Bypass patients without DM2 | No.* | |
|---|---|---|---|---|
| Patients, no. | 771 | 1522 | ||
| Age, mean (SD), y | 67.7 (9.6) | 742 | 64.4 (11.6) | 1474 |
| Men, no. % | 549 (71.4) | 769 | 1,236 (81.6) | 1514 |
| Time since revascularization, mean (SD), y | 3.5 (4.0) | 762 | 3.4 (4.1) | 1505 |
| Systolic blood pressure, mean (SD), mmHg | 134.8 (19.2) | 742 | 131.0 (18.1) | 1460 |
| Diastolic blood pressure, mean (SD), mmHg | 76.4 (11.2) | 741 | 75.6 (10.8) | 1434 |
| Body mass index, mean (SD) | 29.1 (4.5) | 744 | 28.1 (3.8) | 1454 |
| Waist circumference, mean (SD), cm | 101.3 (12.2) | 670 | 97.6 (13.2) | 1255 |
| Hypertension, no. % | 577 (78.1) | 739 | 816 (55.9) | 1460 |
| Dyslipidemia, no. % | 461 (78.4) | 588 | 720 (67.9) | 1061 |
| Smokers, no. % | 62 (8.0) | 771 | 177 (11.8) | 1504 |
| Ex-smokers, no. % | 340 (44.1) | 771 | 771 (51.3) | 1504 |
| GFR<60 mL/min/1.72m2, no. (%) | 223 (32.3) | 691 | 307 (23.1) | 1327 |
DM, diabetes mellitus; GFR, glomerular filtration rate; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
Summary of Pharmacological Treatments in Population With Type 2 Diabetes Mellitus
| Total, no. | DM2, no. (%)* | |
|---|---|---|
| Antiplatelet therapy | 767 | 742 (96.7) |
| Anticoagulant therapy | 748 | 87 (11.6) |
| Antidiabetic therapy | 771 | |
| Insulin in monotherapy | 137 (17.8) | |
| Insulin+OAD | 97 (12.6) | |
| OAD in monotherapy | 446 (57.8) | |
| No drug therapy | 91 (11.8) | |
| Lipid-lowering treatment | 771 | |
| Statin in monotherapy | 578 (75.0) | |
| Ezetimib in monotherapy | 7 (0.9) | |
| Statin + ezetimib | 144 (18.7) | |
| Total statins | 722 (93.6) | |
| Total ezetimib | 151 (19.6) |
DM2, type 2 diabetes mellitus; OAD, oral antidiabetic.
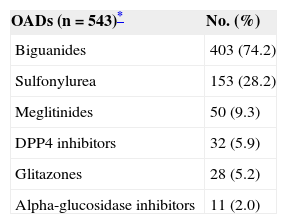
Approximately 2/3 of patients (n=523) had HbA1c data. The mean HbA1c was 7.13%. Approximately half the patients (48.2%) had HbA1c < 7.0%, 69.4% had < 7.5%, and 80.3% had < 8%. Table 2 shows the distribution of the type of hypoglycemic treatment. Most patients (57.8%) were receiving treatment with OADs only, whereas 30.4% used insulin in monotherapy or together with OADs. Among patients who were receiving OAD therapy, metformin (74.2%) and sulfonylureas (28.2%) were used most commonly (Table 3). Among patients taking ≥1 OAD, most (412/543 [76%]) were receiving monotherapy, whereas 22% were taking combined therapy with 2 OADs.
Oral Antidiabetics
| OADs (n=543)* | No. (%) |
|---|---|
| Biguanides | 403 (74.2) |
| Sulfonylurea | 153 (28.2) |
| Meglitinides | 50 (9.3) |
| DPP4 inhibitors | 32 (5.9) |
| Glitazones | 28 (5.2) |
| Alpha-glucosidase inhibitors | 11 (2.0) |
DPP4, dipeptidyl peptidase-4; OAD, oral antidiabetic.
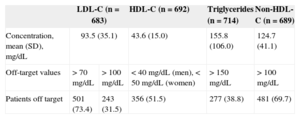
According to the baseline characteristics, 78.4% of diabetic patients who had already undergone revascularization had been diagnosed with dyslipidemia. The mean values were LDL-C, 93.5mg/dL; HDL-C, 43.6mg/dL; triglycerides, 155.8mg/dL; and non-HDL cholesterol, 124.7mg/dL. Additionally, 73% had LDL-C ≥ 70mg/dL and 51.5% had HDL-C<40mg/dL (men) or < 50mg/dL (women); 38.8% had elevated triglycerides (> 150mg/dL), and 18% had abnormal levels in all 3 parameters. Only 63 (10%) patients were within the targets or goals recommended by the lipid therapy guidelines (Table 4).
Summary of Lipid Targets
| LDL-C (n=683) | HDL-C (n=692) | Triglycerides (n=714) | Non-HDL-C (n=689) | ||
|---|---|---|---|---|---|
| Concentration, mean (SD), mg/dL | 93.5 (35.1) | 43.6 (15.0) | 155.8 (106.0) | 124.7 (41.1) | |
| Off-target values | > 70 mg/dL | > 100 mg/dL | < 40 mg/dL (men), < 50 mg/dL (women) | > 150 mg/dL | > 100 mg/dL |
| Patients off target | 501 (73.4) | 243 (31.5) | 356 (51.5) | 277 (38.8) | 481 (69.7) |
HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SD, standard deviation.
Unless otherwise indicated, data are expressed as No. (%) or mean (standard deviation).
Regarding pharmacological treatments for dyslipidemia, three quarters of the population were receiving a statin as monotherapy, whereas 18.7% were taking a statin-ezetimib combination (Table 2). In 93.6% of the population taking statins, atorvastatin was most common (60% of the population), followed by simvastatin (approximately 20%), pravastatin (7%), and fluvastatin (6%).
A total of 78.1% of patients had been diagnosed with hypertension (Table 1). In the hypertensive population, mean systolic BP was 137.5mmHg and mean diastolic BP was 77.3mmHg. A total of 93% and 52% of hypertensive patients achieved systolic/diastolic BP values < 140/90mmHg and < 130/80mmHg, respectively.
According to eGFR, 32.3% of patients had chronic renal failure. In general, no differences were observed in the control of glycemic levels (HbA1c, 7.14% ([1.32%]) in MDRD<60 vs 7.11% ([1.36%]) in MDRD>60; difference, 0.034%; P=.794). This was also true for BP (systolic BP, 135.7 [19.83] mmHg vs 133.93 [17.83mmHg]; difference, 1.77mmHg; P=.248; diastolic BP, 76.77 [12.54] mmHg vs 75.99 [10.02] mmHg; difference, 0.78mmHg; P=.394) and for lipid profile (LDL-C, 93.0 [35.53] mg/dL vs 93.78 [35.03] mg/dL; difference, –0.774mg/dL; P=.797; HDL-C, 43.8 [15.52] mg/dL vs 43.6 [14.74] mg/dL; difference, 0.16 mg/dL; P=.898; triglycerides, 154.90 [81.67] mg/dL vs 156.6 [118.62] mg/dL; difference, −1.7mg/dL; P=.850; non-HDL-C, 126.09 [40.47] mg/dL vs 123.76 [41.17] mg/dL; difference, 2.33mg/dL; P=.502) among patients with and without chronic renal failure.
DISCUSSIONThis substudy of diabetic patients in the ICP-Bypass study provided an opportunity to investigate and describe the extent of control of risk factors, such as glycemic level and lipid and blood pressure profile, as well as the treatment of this very high-risk population that receives follow-up in cardiology outpatient clinics.
The characteristics of the population included in this substudy were generally similar to those of the nondiabetic population in the ICP-Bypass study.14 However, several differences often seen among diabetic populations can be observed, for instance, a higher incidence of hypertension or chronic renal failure, a known complication of DM.16 Likewise, the lower incidence of active smokers (8% vs 51.3% of the nondiabetic study population) but much higher incidence of ex-smokers (44.1% vs 10.5%) may reflect greater adherence to recommended lifestyle modifications.3–5
Approximately half the patients had achieved HbA1c values < 7.0%, which is the target generally recommended by the various clinical guidelines and consensuses,17 including the multidisciplinary consensus sponsored by the Spanish Diabetes Society.18 This percentage is also in line with the results of local epidemiologic studies conducted in the general diabetic population in Spain.19
Most clinical guidelines currently recommend individualization of treatment and establish less strict glycemic targets according to advanced cardiovascular disease, comorbidities, functional status, and/or life expectancy.17 Although more aggressive goals may be appropriate in view of the high cardiovascular risk of the patients in our study, the ACCORD study20 included > 10000 patients with with DM2 and a history of cardiovascular events or additional cardiovascular risk factors and observed an increased mortality in the intensive (target<6%) vs standard (< 7.0%) treatment group. In addition to increased hypoglycemia in the intensive arm observed in the ACCORD study20, subsequent analyses showed that hypoglycemia is associated with an increased risk of mortality regardless of the type of treatment (standard or intensive). Although hypoglycemia has not been shown to be directly responsible for the increased mortality observed in the intensive arm of the ACCORD study, it is known that hypoglycemia-induced hemodynamic, hematologic, and/or electrocardiographic changes can lead to an increase in cardiovascular events, particularly in patients with a history of coronary disease. A study carried out in diabetic coronary patients using continuous glucose and Holter electrocardiographic monitoring observed the presence of electrocardiographic abnormalities and/or ischemic symptoms in the context of hypoglycemia events, some of them asymptomatic.21 Therefore, avoiding low glycemic levels in the context of ischemic heart disease appears to be clearly recommendable.
In the context of this individualization, the Spanish Diabetes Society recommends a target of HbA1c < 7.5% for patients with advanced atherosclerotic disease, prioritizing treatment safety at all times. If this more flexible goal is used, 70% of patients in our study were on target.
Regarding the drugs used for glycemic control, the higher use of metformin observed in our study was in accordance with the recommendations that establish it as the first-line therapy of choice. Insulin use was higher (30.4%) than that reported in studies conducted among the general diabetic population in our setting (16%-23%),22,23 although this may be explained by a possibly longer history of DM in these patients (data not recorded in our study) and the resulting deterioration in beta-cell function, as well as by a higher prevalence of chronic renal failure. The combination of OADs and the use of secretagogues (eg, sulfonylureas) widely used as adjuvant therapy, were relatively low. The higher prevalence of chronic renal failure and the limitations of sulfonylureas in this condition may have had some influence on the therapeutic decision.
In addition to the increased risk of hypoglycemia described with these drugs,24 observational clinical studies and meta-analyses have observed a higher risk of cardiovascular events and/or mortality with sulfonylureas, compared with metformin or combinations with metformin.25-27 Concern about both hypoglycemia and deleterious effects may also have led to the lower use of sulfonylureas in revascularized patients. The low use of glitazones is not surprising, due to concerns about cardiovascular effects in patients with a history of coronary disease,28,29 which ceased when rosiglitazone was withdrawn from the European market in 2010. More recently, incretin-based drugs have been shown to have a low risk of hypoglycemia and a neutral or beneficial effect on weight and, therefore, have been included as an alternative for these patients.30 The presence of these drugs in our study is low, as the drugs were first marketed in Spain in 2007.
It is worth noting that three quarters of patients in our study had LDL-C>70mg/dL. In a study by Pérez de Isla et al,31 the percentage of patients with LDL-C>70mg/dL, a history of coronary disease, and DM2 was slightly higher (81%) than in our population of revascularized diabetic patients. The general impression gained from these data is that the situation could be improved. Statin therapy has become a key part of the strategy to control dyslipidemia in patients with DM. In our study, only 6.4% of the population were not receiving any statins. In addition to statins, other options to lower LDL-C levels among these patients are presented.
The treatment guidelines for patients with documented cardiovascular disease state that the highest statin dose tolerated should be used to reach the LDL-C targets.3,15 Despite this, the use of statins of medium potency (or the equivalent dose for statins of higher potency) has not been extensively analyzed in clinical trials, which have usually focused on comparing intensive vs low-dose or low-potency treatments.10 The use of medium doses, in combination with other lipid-lowering agents (eg, a cholesterol-absorption inhibitor), would provide an option to the possible complications of long-term treatments, such as muscle disease, and would maintain control of LDL-C levels,32 particularly important in the diabetic population which, at LDL-C values that are not very high, have a higher number of smaller and denser particles, which are particularly atherogenic.7
In our study, half the hypertensive patients had controlled BP<130/80mmHg and >90%, < 140/90mmHg. These percentages are significantly higher than those described in various national studies for patients with diabetes or cardiovascular diseases.23,33 The BP values are in line with the targets recommended by the latest clinical practice guidelines.34,35
LimitationsBecause there was no monitoring in the study, we cannot rule out a selection bias or the inclusion of better-controlled patients, which would be a limitation for this study.
Other study limitations include the inherent limitations of observational cross-sectional studies, for example, the retrospective nature of the collection of some parameters and the unavailability of some variables. Approximately a third of patients had no HbA1c data, and although there may be questions about the possibility of extrapolating the results to all study patients, a comparative analysis of the population with and without HbA1c measurements (data not shown) did not reveal any significant differences in the demographic or clinical characteristics. Because the study involved only cardiologists, included patients with stable heart disease, and had a potential selection bias, as mentioned earlier, the results may not be extrapolable to all diabetic patients with revascularized ischemic heart disease. Despite these limitations, this study describes the clinical and therapeutic characteristics of a broad sample of patients with DM2 and prior revascularization, thus providing information on a group at very high cardiovascular risk. This information can be used to identify where these patients can be managed better in order to lower their cardiovascular risk. In fact, a recent analysis of secondary prevention in diabetic patients with coronary disease advocates the exploration of new preventive strategies.36
CONCLUSIONSOur study found that patients with diabetes and revascularized coronary disease should be controlled more closely in terms of certain risk factors, particularly lipid levels. Conversely, control of blood pressure and glycemic levels was rather good, although patients with HbA1c>7.5% (30%) and>8.0% (20%) should be individually checked and assessed with regard to control targets. Other factors, such as age, functional status, life expectancy, and other comorbidities, should also be considered.
FUNDINGThe ICP-Bypass study was funded by MSD (Merck Sharp & Dohme) Spain.
CONFLICTS OF INTERESTSG. Vitale and S. Fernández-Anaya are employed by MSD España.