To the Editor:
An 87-year-old male with symptomatic aortic stenosis was referred for percutaneous aortic valve implant. The preoperative echocardiogram demonstrated severe aortic valve stenosis (calculated area, 0.6 cm2), normal left ventricular ejection fraction and cardiac anatomy suitable for the percutaneous implant (absence of calcified nodes in the aortic valves, thoracic aorta without severe calcification—porcelain aorta—, atheromas >5 mm thick, and no aneurysm, absence of excessive angulation in the aortic arch or horizontalised aortic arch). The previous coronary catheterisation showed no significant lesions. The patient was rejected for surgery due to his elevated comorbidity (EuroSCORE, 23%).
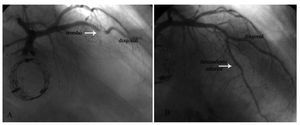
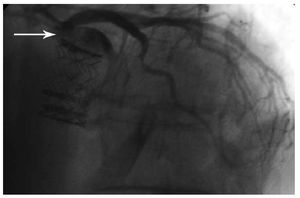
The procedure was performed under general anaesthesia and mechanical ventilation, with transoesophageal echocardiogram monitoring. A 23 mm Edwards-Sapiens prosthesis was implanted via retrograde approach, with right artery femoral access and vascular suturing. Six hours after the procedure ST elevation was observed in anterior leads and akinesia in apical segments in the echocardiogram. Suspecting an anterior myocardial infarction in evolution, an emergency coronary catheterisation was performed (Figure 1), demonstrating occlusion in the anterior descending artery, together with the presence of radiolucent material with a friable appearance in the left sinus of Valsalva (between the implanted prosthesis, the displaced aortic leaflet and the aortic wall) (Figure 2). A coronary intervention procedure was performed, with thrombectomy (Pronto®; Boston Scientific) which opened the anterior descending artery, with no remnant of thrombus in the main vessel but with migration of the thrombus to the diagonal branch. A stent was implanted (Chronos 2.25×16 mm; Sorin Group) and the vessel was opened and distal flow restored.
Figure 1.A: coronary catheterisation; occlusion of the anterior descending artery is observed, at the bifurcation with the second diagonal, compatible with intracoronary thrombus. B: final result after the thrombectomy and the stent implant in the diagonal artery.
Figure 2.Paravalvular recess formed between the implanted aortic valve, the left aortic leaflet and the left sinus of Valsalva, with a radiotranslucent image in its interior and blood stasis.
The patient evolved favourably with no complications. The control echocardiogram demonstrated anterior hypokinesia, moderate ventricular dysfunction and normal functioning of the implanted prosthesis.
The implantation of percutaneous aortic prostheses is an alternative therapy for the treatment of patients with symptomatic aortic stenosis not susceptible to cardiac surgery, with good initial results,1 but not free from complications, with a mortality rate at 30 days of 12%-16%.2,3 Among the complications, the most prevalent are vascular access problems,2 valve migration problems,2,4 paravalvular aortic regurgitation,2,3 mitral insufficiency,5 cerebrovascular accident,2 and even death due to occluded left main artery.2 Infarctions have been described in the follow-up, but not in the immediate postoperative stage.2
Infarction in the immediate postoperative period may be due to several causes. First, the migration of atheroma fragments from the native aortic valve or ascending aorta towards the coronary circulation. Although the phenomenon has been widely documented in aortic vascular surgery procedures as a cause of cerebrovascular accident,6 coronary embolism is very infrequent. A second possibility is the appearance of a thrombus on the prosthesis. Anticoagulation in biological valve prostheses is not recommended, apart from implantation procedure to maintain an ACT >250.1 After implantation, dual antiplatelet therapy is maintained with acetylsalicylic acid (ASA) and clopidogrel for 3 months and subsequently ASA indefinitely.2 However, implantation of metallic prosthetic material can trigger the activation of coagulation and favour the appearance of thrombus on the valve surface, especially in cases of poor co adaptation of the valve in areas of blood stasis, such as those that form in the insertion area between the valve and the native aortic leaflets.
In our case, it was not possible to extract and analyse the embolic material. Nevertheless, given its friability, a thrombotic origin was suspected. Correct antiplatelet therapy prior to the procedure, together with careful anticoagulation for the first 24 hours after the procedure could avoid thromboembolic complications. Similarly, a 300-600 mg dose of clopidogrel immediately afterwards could be appropriate.