Drug challenge tests used to elicit a Brugada electrocardiographic pattern (B-ECG) are fundamental in the diagnosis of this syndrome. Sodium channel blockers used in the treatment of cardiac arrhythmias, mainly ajmaline and flecainide, are the agents most widely employed because of their demonstrated efficacy and safety in unmasking the B-ECG. The results of the test are considered positive if, during infusion of the drug, a nondiagnostic B-ECG (type 2 or 3) becomes a diagnostic B-ECG (type 1 or coved type), which is characterized by ST segment elevation ≥ 2mm followed by a negative T wave in more than 1 precordial lead (V1-V3). These tests are usually performed in an outpatient setting and, once the electrocardiogram has become normalized, the patient is discharged after a short monitoring period. There is no information in the literature concerning the incidence and implications of late positive responses following an initially negative flecainide test (FT).
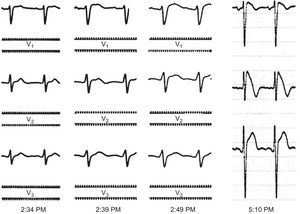
We report the case of a 32-year-old man who was asymptomatic and had no family history of sudden cardiac death. He was referred to our hospital to undergo a FT when he was found to have a type 3 B-ECG in a routine electrocardiogram. The results of a physical examination and a battery of analyses were normal. The existence of structural heart disease was ruled out by echocardiography. A baseline electrocardiogram performed prior to the FT revealed no abnormalities. Following flecainide infusion (2mg/kg body weight for 10minutes), the patient had a significantly prolonged QRS interval, but met none of the diagnostic criteria for B-ECG (with precordial leads V1 and V2 placed both in the fourth and in the third intercostal space). Although the widening of the QRS complex did not meet the criteria for interrupting the test (QRS>130% of baseline value), he was admitted to the hospital for electrocardiographic monitoring until the intraventricular conduction disturbance had been corrected. Two hours after completing the administration of flecainide, we detected coved ST-segment elevation in the right precordial leads, a finding that met the criteria for type 1 B-ECG (Figure). Twenty-four hours later, the electrocardiogram had returned to normal and the patient was discharged home.
Right precordial leads (V1-V3) at 25mm/s and 10mV/mm. The tracings in the first 3 panels were obtained in the electrophysiology laboratory with an EP-WorkMate polygraph (St. Jude Medical). The fourth panel is a standard digital electrocardiogram obtained in the cardiology department.
This report describes a case of a late positive response to FT after an initial negative result. It was discovered incidentally because the patient underwent a longer than usual period of electrocardiographic monitoring.
Among the antiarrhythmic sodium channel blockers currently available, ajmaline has been found to exhibit the greatest efficacy in unmasking B-ECG. Hong et al1 evaluated ajmaline in a cohort of 147 carriers of mutations in the SCN5A gene. They reported a diagnostic sensitivity and specificity of 80% and 94%, respectively, as well as a positive predictive value of 93% and negative predictive value of 83% for he syndrome. Meregalli et al2 analyzed the effect of flecainide in 110 carriers of the same gene; they obtained a sensitivity of 77%, specificity of 80%, positive predictive value of 96%, and negative predictive value of 36%. The 2 drugs were compared in a studyby Wolpert et al3 involving 22 probands with a genetic diagnosis of Brugada syndrome; ajmaline had a higher detection capacity (22 of 22) than flecainide (15 of 22) and a more marked ST-segment elevation. The reproducibility of FT has also been controversial. Gasparini et al4 found a reproducibility of 100%. However, there are reports of cases in which the test was negative, although the initial response had been positive.5
Despite the superiority of ajmaline, the fact that in many countries it is not available has made flecainide the drug of choice in most electrophysiology laboratories. The differences between the 2 drugs have been related to flecainide's greater inhibition of the transient outward potassium current3 (Ito). This reduces the ionic imbalance between the positive inward and outward currents at the end of phase 1 of the action potential that enables the unmasking of the B-ECG.
The case of a delayed positive response to flecainide reported here might indicate that results considered to be negative at the time of the challenge test may be false negatives, since the electrocardiographic monitoring time is usually 30minutes or less.
Studies involving a larger number of patients should be carried out to examine whether the systematic prolongation of the monitoring period following a FT could contribute to reducing the number of false negatives.