A large mass of heart muscle is dependent on lesions in the left main coronary artery (LMCA), making revascularization of this structure perhaps more important than in other locations. In general, the decision to revascularize is based on angiography findings.
The quantitative flow ratio (QFR) is a new index that has shown good agreement with the fractional flow reserve (FFR), a value obtained invasively in several clinical situations. The QFR uses 2 coronary angiography views to estimate the FFR based on computational fluid dynamics and 3-dimensional reconstruction without the need for a pressure wire. There is very little evidence on QFR use in the LMCA, and the manufacturers themselves advise against using it in lesions affecting the ostium or bifurcation
This retrospective, observational study in daily clinical practice was designed to assess the diagnostic performance of the QFR to estimate the FFR obtained with an invasive technique and to compare it with angiographic evaluation in inconclusive LMCA lesions
Angiograms of all patients with LMCA stenosis between 30% and 70% by visual estimation and 1 FFR study were analyzed in a single center between January 1, 2018 and May 15, 2019. Studies not including 2 views separated by at least 25° angulation and those of insufficient quality for QFR assessment were excluded.
The visual assessment was carried out by 2 operators whose experience included more than 1000 procedures for functional assessment of coronary lesions. Operators were blinded to the FFR results.
The QFR was measured with the Medis Suite XA QAngio XA 3D QFR software, version 3.2.28.0 (Medis, The Netherlands),1 taking the angiographic location of the pressure wire sensor as the distal point and without knowledge of the FFR value.
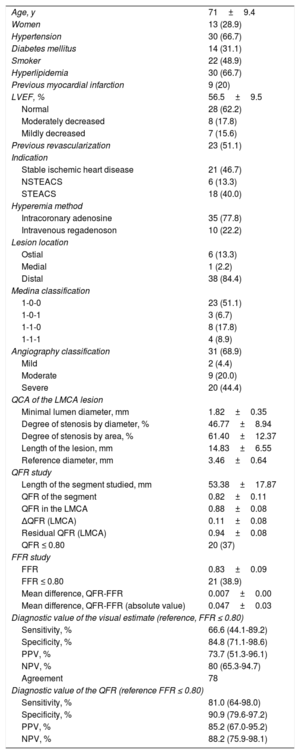
In total, 66 studies from 57 patients were analyzed. Fifty-four studies (81.8%) from 45 patients were suitable for determining the QFR. Eight studies were excluded because they lacked 2 views separated by 25° in which the bifurcation of the trunk was visible without overlapping branches, and 4 because they showed severely calcified lesions impeding proper delineation of the vessel borders (table 1).
Baseline characteristics of the patients and procedures
| Age, y | 71±9.4 |
| Women | 13 (28.9) |
| Hypertension | 30 (66.7) |
| Diabetes mellitus | 14 (31.1) |
| Smoker | 22 (48.9) |
| Hyperlipidemia | 30 (66.7) |
| Previous myocardial infarction | 9 (20) |
| LVEF, % | 56.5±9.5 |
| Normal | 28 (62.2) |
| Moderately decreased | 8 (17.8) |
| Mildly decreased | 7 (15.6) |
| Previous revascularization | 23 (51.1) |
| Indication | |
| Stable ischemic heart disease | 21 (46.7) |
| NSTEACS | 6 (13.3) |
| STEACS | 18 (40.0) |
| Hyperemia method | |
| Intracoronary adenosine | 35 (77.8) |
| Intravenous regadenoson | 10 (22.2) |
| Lesion location | |
| Ostial | 6 (13.3) |
| Medial | 1 (2.2) |
| Distal | 38 (84.4) |
| Medina classification | |
| 1-0-0 | 23 (51.1) |
| 1-0-1 | 3 (6.7) |
| 1-1-0 | 8 (17.8) |
| 1-1-1 | 4 (8.9) |
| Angiography classification | 31 (68.9) |
| Mild | 2 (4.4) |
| Moderate | 9 (20.0) |
| Severe | 20 (44.4) |
| QCA of the LMCA lesion | |
| Minimal lumen diameter, mm | 1.82±0.35 |
| Degree of stenosis by diameter, % | 46.77±8.94 |
| Degree of stenosis by area, % | 61.40±12.37 |
| Length of the lesion, mm | 14.83±6.55 |
| Reference diameter, mm | 3.46±0.64 |
| QFR study | |
| Length of the segment studied, mm | 53.38±17.87 |
| QFR of the segment | 0.82±0.11 |
| QFR in the LMCA | 0.88±0.08 |
| ΔQFR (LMCA) | 0.11±0.08 |
| Residual QFR (LMCA) | 0.94±0.08 |
| QFR ≤ 0.80 | 20 (37) |
| FFR study | |
| FFR | 0.83±0.09 |
| FFR ≤ 0.80 | 21 (38.9) |
| Mean difference, QFR-FFR | 0.007±0.00 |
| Mean difference, QFR-FFR (absolute value) | 0.047±0.03 |
| Diagnostic value of the visual estimate (reference, FFR ≤ 0.80) | |
| Sensitivity, % | 66.6 (44.1-89.2) |
| Specificity, % | 84.8 (71.1-98.6) |
| PPV, % | 73.7 (51.3-96.1) |
| NPV, % | 80 (65.3-94.7) |
| Agreement | 78 |
| Diagnostic value of the QFR (reference FFR ≤ 0.80) | |
| Sensitivity, % | 81.0 (64-98.0) |
| Specificity, % | 90.9 (79.6-97.2) |
| PPV, % | 85.2 (67.0-95.2) |
| NPV, % | 88.2 (75.9-98.1) |
FFR, fractional flow reserve; LMCA, left main coronary artery; LVEF, left ventricular ejection fraction; NSTEACS, non-ST-segment elevation acute coronary syndrome; STEACS, ST-segment elevation acute coronary syndrome; NPV, negative predictive value; PPV, positive predictive value; QCA, quantitative coronary analysis; QFR, quantitative flow ratio
Values are expressed as the number (%), mean±standard deviation, or mean (range).
An FFR value ≤ 0.80 was obtained in 21 studies (39%). The visual estimate concurred with FFR ≤ 0.80 in 78%. Concordance between the QFR and FFR values obtained (with a cutoff ≤ 0.80) was 87% (correlation coefficient, R=0.79) (figure 1A,B).
A, Scatter plot with regression line between the fractional flow reserve (FFR) and quantitative flow ratio (QFR) values. Continuity equation and R and R2 values. B, Bland-Altman plot for the FFR and QFR values. C: ROC curves of the QFR values, stenosis by diameter, and minimum lumen diameter (MLD).
Areas under the receiver operating characteristic (ROC) curve were 0.88, 0.67, and 0.81 for QFR, stenosis by diameter, and minimum lumen diameter, respectively (figure 1C).
The agreement and area under the ROC curve values obtained in our study are similar to or somewhat lower than those found in other locations. In a meta-analysis including 9 studies involving 1111 vessels and comparing the FFR and QFR, the area under the ROC curve was 92%.2 In another meta-analysis,3 the length of the lesion, higher degree of stenosis, and diabetes were factors associated with greater discrepancy between the FFR and QFR. As bifurcation and ostial lesions have been excluded from the studies to date, it cannot be determined whether these locations may be a cause of disagreement between the 2 indices. LMCA lesions mainly affect the bifurcation, which makes QFR calculation more complex.
Angiography-derived indices are attributed the advantages of greater applicability with lower costs, procedure times, and complications. It is controversial whether these indices represent a closer approximation to physiological lesion assessment or a reversal with a return to morphological assessment.4 The FFR incorporates microvascular involvement when determining the indication to revascularize an epicardial lesion. In a recent study,5 microvascular involvement was associated with lower diagnostic yield of the QFR in predicting the FFR value. An index that is not specific to the lesion could lead to inappropriate decisions based on cutoffs similar to those used in intracoronary ultrasound and optical coherence tomography.
A limitation of this study is the small number of procedures included, among which 20% were unsuitable for measurement. Thus, it should be considered a pilot study. Measurements were not performed in a central laboratory, but they were done by operators certified in QFR determination, and intracoronary adenosine was used in most of the studies, without involvement of the ostium.
In conclusion, this study, the first to compare QFR and FFR findings in the LMCA, shows that retrospective QFR determination can be performed in more than 80% of LMCA lesions with> 85% agreement, which is higher than that obtained by angiography. In consideration of the clinical importance of LMCA lesions, we believe that the functional repercussions should be one of the factors to take into account in the decision to revascularize vessels with moderate stenosis.