Keywords
INTRODUCTION
Over half of all deaths in Spain occur in hospitals.1 Do-not-resuscitate (DNR) orders are used with increasing frequency and most non-sudden deaths in Europe are preceded by such orders.2 However, DNR orders and discussion of resuscitation are less frequent in patients with cardiovascular disease than in patients with diseases such as cancer.3-5 Our goal was to evaluate the use of DNR orders and palliative care in cardiac patients. We hypothesized that there would be considerable room for improvement in implementing these orders.
METHODS
Data was obtained retrospectively from a registry of all deaths in the cardiology department of a tertiary hospital from January 2007 to February 2009. Data collected included:
- Demographic variables, cardiovascular risk factors (diabetes mellitus, hyperlipidemia, smoking, hypertension, obesity defined as a body mass index [BMI] >30), and antecedents included in medical records.
- Patient location and test results.
- Variables relating to the DNR order, including existence or absence of the order, whether included in the medical or nursing notes, and whether discussed or not with the patient or the patient's family. Date of order. Measures to limit therapeutic effort. Prior use of aggressive care.
- Use of palliative treatment: morphine chloride, spiritual care from the hospital chaplain or other means, disconnection of implantable cardioverter defibrillator.
- Autopsy: request to the family and performance.
In all cases, the decision not to resuscitate was taken individually by the attending physician. The study was approved by the hospital ethics committee.
Between-group comparisons were carried out using c2 or Fisher's exact test for categorical variables and Student t test for continuous variables. Analyses were performed in version 12 of SPSS (SPSS Inc., Chicago, Illinois, USA).
RESULTS
During the study period, 9587 patients were admitted to the unit and 198 (2%) died. Among those who died, resuscitation was ruled out in 113 (57%); these patients tended to be older, with more co-morbidities, a higher percentage of admissions due to heart failure, and longer duration of stay in the unit. They were also less frequently admitted to the coronary care unit (Table 1).
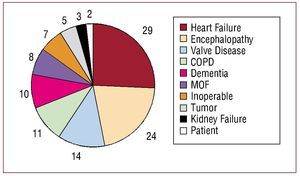
The following data refer to the 113 patients in which the decision not to resuscitate was recorded in writing. In 3 patients, the DNR order was given within 24 hours of admission. The median number of days from admission until the order was 7 (interquartile range, 3-21.3 days). In most cases, the decision not to resuscitate was based on several factors, though these frequently included older age, co-morbidity, and the presence of heart disease. The principal factors involved in the decision are shown in Figure 1.
Figure 1. Main reason patient considered not revivable in 113 consecutive cases. COPD, chronic obstructive pulmonary disease; Dementia, cognitive deterioration; Encephalopathy, severe encephalopathy or electroencephalogram with poor prognosis; Heart failure, severe heart failure or cardiogenic shock; Inoperable, non-valvular surgical conditions inoperable due to high risk; MOF, multiple organ failure; Patient, patient's wishes; Tumor, advanced tumor; Valve disease, inoperable severe valve disease.
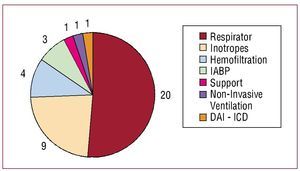
The DNR order was recorded in the patient's medical record in 102 (90.3%) cases and in the nursing notes in 74 (65.5%) cases. A note was made to inform patients of the DNR order in 5 (4.4%) cases and to inform the family in 95 (84.1%) cases. As well as the DNR order, therapeutic efforts were explicitly limited in the 24 h preceding death in 39 (34.5%) patients, as shown in Figure 2. Palliative treatment was used infrequently in DNR patients and many had received aggressive and expensive treatments prior to the DNR order (Table 2). An advance directives document was not included in any of the patients' medical records.
Figure 2. Measures withdrawn to limit therapeutic efforts during the 24 hours prior to death in 39 patients. Hemofiltration, withdrawal of continuous venous hemofiltration; IABP, withdrawal of intra-aortic balloon pump; ICD, disconnection of implantable cardioverter defibrillator; Inotropes, withdrawal of inotropic perfusion; Non-invasive ventilation, withdrawal of non-invasive ventilation; Respirator, extubation and withdrawal of mechanical ventilation (2 with withdrawal of inotropes and 1 with withdrawal of IABP; Support, stopping previously implanted ventricular support.
DISCUSSION
Almost 3 out of 5 patients who died in our unit over the study period had a DNR order. In many cases the decision to apply a DNR order was taken only after a prolonged stay in the unit and the application of aggressive therapeutic measures. Only half of the patients assigned a DNR order received morphine chloride as a palliative measure, spiritual care was rare, and implantable cardioverter defribrillators were not disconnected in 3 of the 4 patients wearing the device, suggesting room for improvement in that area.
Most non-sudden deaths in Spain are preceded by DNR orders.2 We observed that DNR patients had more co-morbidity and were older. In previous studies, the variable most frequently associated with these orders was age.6
In our series, few attempts were made to ascertain patient preferences and only 4% were informed of the decision not to resuscitate. It has been reported that the decision is made without taking into account patient wishes in over two thirds of cases,6 despite the fact that in many cases patients should not be deprived of the possibility of resuscitation without prior discussion.6 In a study of cardiac arrest in 2505 octogenarians, Goodlin et al7 found clear discrepancies between the desire to receive resuscitation and attitudes towards resuscitation. In a quarter of patients with heart failure, physicians were found to have a misguided view of the patient's desire to be resuscitated.3 On the other hand, the decision-making capacity of patients with terminal heart disease can be affected by the advanced condition of the illness. Patients likewise sometimes do not want to be informed, do not want to have to decide, or may be very ambivalent.3 The decision to apply a DNR order was not previously agreed with the family in 16% of our series. Most patients and family members consider it essential to talk to the clinician regarding the patient's death and DNR orders,3 but this type of dialogue is difficult for physicians.6 The decision should also be disclosed in all clinical documents. In our series, it is striking that the decision to apply the DNR order did not appear in the nursing notes in 34% of cases. The final decision to resuscitate or not can frequently be taken in a question of seconds by a doctor on call, so it is imperative that DNR orders are reflected in the most easily accessible documentation, which would usually be the nursing notes.
With regard to the deficits we observed in palliative care, specialists in this type of care have been found to have little training in heart disease, and vice-versa.8 This lack of training contrasts with the widespread use of aggressive measures in patients later considered DNR during the same period of hospitalization. The fact that implantable cardioverter defibrillators were not disconnected in 3 of the 4 patients using the device is particularly noteworthy. After interviewing 100 relatives of patients who died with a defibrillator, Goldstein et al9 showed that the possibility of disconnection was only raised with 27, 21 of whom accepted disconnection.
In our study, therapeutic efforts were explicitly limited in 35% of patients. From an ethical point of view, there is no great difference between not initiating life support treatment or withdrawing such measures once they have been implemented. However, for the clinician it is a more difficult decision to withdraw such measures than not to implement them.10 The problem is relevant, as the percentage of deaths preceded by limitation of therapeutic effort seems to be increasing.11 This suggests a need for tools which will permit early detection of patients who will not benefit from aggressive management.
Finally, the very low rate of requests for and performance of autopsies observed here is a reflection of the decline in the number of autopsies performed in Spanish hospitals, a decline which has previously been described as alarming.12
Our study suffers from limitations inherent in retrospective data collection. Using previous diagnoses probably meant that dementia was under-diagnosed. Moreover, the number of patients analyzed limited our ability to draw definitive conclusions. Finally, as this was a single-center study it reflects management in only one hospital so we should be cautious about extrapolating the results to other centers.
In conclusion, resuscitation was not considered appropriate in 3 of every 5 patients who died in the cardiology unit studied. The decision to issue a DNR order was frequently taken after administering aggressive treatment and little palliative care was provided afterward.
This study was financed in part by the Spanish Cooperative Cardiovascular Disease Research Network (RECAVA).
Correspondence:
Dr. M. Martínez-Sellés.
Servicio de Cardiología. Hospital General Universitario Gregorio Marañón. Dr. Esquerdo, 46. 28007 Madrid. Spain.
E-mail: mmselles@secardiologia.es
Received April 29, 2009.
Accepted for publication June 3, 2009.