To the Editor,
The modified Blalock-Taussig shunt (MBT) is the preferred treatment in neonates with duct-dependent heart disease and decreased pulmonary blood flow, in patients in whon complete correction is not possible. Thrombosis is the most serious complication and has been treated via the surgical removal of obstructions, fibrinolysis, mechanical recanalization with angioplasty, and/or stenting. Using another shunt should always be avoided. In recent years, coronary stents have been used to ensure the ductus remains permeable and to guarantee pulmonary flow.1 We report on 2 neonates who received ductal stent implantation after acute thrombosis of a shunt.
Neonate diagnosed in utero with pulmonary atresia with intact ventricular septum. Cardiac catheterization was performed on the sixth day of life. Right ventricular pressure was suprasystemic. There was no passage of contrast into the pulmonary artery. A 0.014 guide wire was inserted and balloon valvuloplasty was performed with sequential 3 / 20, 5 / 20, and 7 / 2 balloons. Echocardiography showed a moderate tricuspid regurgitation, atrial septal defect with right-to-left shunt, and a gradient of 36 mmHg in the pulmonary valve. Repeated attempts to discontinue prostaglandin led to saturation <70%. A right MBT performed on day 22 thrombosed and prostaglandins had to be restarted. On day 24, a SprinterRX Driver 3.5 / 15 stent (Medtronic ®) was implanted in the ductus via the femoral artery (FA) using a right coronary guiding catheter; saturation increased to 90%. The child was discharged with clopidogrel (0.2 mg/kg/day) and aspirin (5 mg/ kg/day).2 When the child was 6 months old, a transannular patch was placed and stent flow was interrupted with a clip.
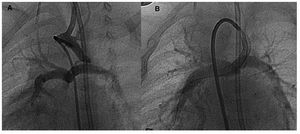
A 1500-g neonate diagnosed with pulmonary atresia with ventricular septal defect, right aortic arch, ductus left and left superior vena cava, was administered prostaglandin to 2 months and underwent a right MBT shunt. Prostaglandin perfusion was restarted at 24 h as saturation was <65%. Echocardiography detected no flow in the BTM and confirmed the permeability of the ductus. The FA catheterization showed thrombosis of the shunt, a right aortic arch and left ductus originating from the left subclavian artery, with a long and tortuous route to the left pulmonary artery (Figure 1). The attempt to cross the ductus caused a severe spasm (Figure 2A). A right coronary guiding catheter was used to implant a SprinterRX Driver 3.5/15 (Medtronic ®) stent together with a Pro-Kinetic Energy 3.5/20 (Biotronic AG ®) stent which overlapped the first, in order to fully cover the ductus (Figure 2B). Saturations increased from 60% to 90%. The child is being treated with clopidogrel and aspirin pending a Rastelli intervention.
Figure 1. Right aortic arch with tortuous left ductus originating in the left subclavian artery.
Figure 2. A: severe constriction in the pulmonary end of ductus. B: ductus after stent implantation.
The use of ductal coronary stents has improved outcomes and reduced complications. Several technical aspects are important, and complications increase if the morphology of the ductus is tortuous. It is essential to cover the entire ductal tissue to prevent stenosis of the ductus and to decrease pulmonary blood flow. Case 2 is an example of a variant of ductus rarely described in the literature.3 Normally, the ductus is located on the same side as the aortic arch. In this patient, the first stent did not cover the ductus and an overlapping stent had to be used to ensure coverage of the remaining stenotic area.
Prostaglandin perfusion is always stopped 6 h before. The ductus then becomes moderately restrictive, thereby facilitating stent implantation. Both patients have shown excellent progress and the need for a new shunt has been avoided. Recent studies have indicated that pulmonary arteries show similar growth in patients treated with stents and those treated with a shunt.4 Stents do not complicate later surgery and can be removed or closed with a clip. In view of these results, we believe ductal stenting offers a viable alternative in cases of MBT thrombosis.