The coronavirus disease 2019 (COVID-19) pandemic has required changes in the workflow of medical procedures, including those related to cardiology and electrophysiology. In 2020, guidance was published to maximize the safety of health care personnel and patients during cardiac electrophysiology procedures during the pandemic.1 The article emphasizes the use of the outpatient setting for some procedures. Since the beginning of 2022, there has been an increase in hospital workload, which has reduced the availability of hospital beds for patients undergoing outpatient interventions. In this context, many hospitals have adapted to this new reality and have found that earlier discharge is feasible and safe. Previously, Marijon et al.2 demonstrated that early discharge protocols (4-6hours) for patients undergoing uncomplicated radiofrequency ablation were safe and applicable in routine clinical practice. The document also highlights higher patient satisfaction (in relation to shorter hospital stay), as well as cost savings.
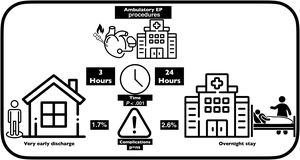
In 2022, Rashedi et al.3 published a systematic review and meta-analysis of the safety and efficacy of early discharge after atrial fibrillation ablation, supporting the adoption of these protocols. The support of a day hospital has allowed many arrhythmia units to implement early discharge protocols (6-8hours) for cardiac device implantation, reducing costs and increasing patient satisfaction.4,5 In addition, for these patients, the widespread use of remote monitoring has enhanced the safety of these procedures even further.6 In summary, outpatient interventional cardiac procedures have become increasingly common, increasing satisfaction rates and reducing costs, without affecting procedural safety. For all these reasons, in April 2022, we started a very early discharge protocol (VEDP) for a series of electrophysiology procedures and first implantation of devices despite not having a day hospital for postprocedure monitoring.
We conducted a comparative analysis with a historical cohort of outpatients with a standard protocol (SP) from September 2018 to April 2019. In accordance with ethics guidelines, all participating patients provided informed consent, and the study received approval from the appropriate ethics committee. Informed consent forms were duly obtained and archived.
We analyzed acute complications (prior to discharge) and those requiring some type of medical intervention within the first 30 days, particularly those causing prolongation of hospital stay. The VEDP included 185 patients and the SP included 189. All procedures were performed in a cardiac electrophysiology laboratory.
In the VEDP, after the procedure, patients remained in a room adjacent to the electrophysiology laboratory, with standard monitoring until discharge, which involved the monitoring by a part-time nurse (who carries out the presurgical preparation of the single electrophysiology laboratory and the 2 catheterization laboratories in the same area). Additionally, an electrocardiogram and chest X-ray were performed, if an implant was performed, in addition to checking the surgical wound or puncture site. The SP involved an elective admission until the morning after the procedure in the cardiology inpatient ward, without continuous monitoring and with standard nursing care. Both groups maintained the same antithrombotic treatment management protocol, and a remote monitoring system was provided to all patients undergoing device implantation prior to discharge.
Table 1 and figure 1 show a summary of all the procedures performed and the characteristics analyzed regarding their safety. The average length of stay was significantly lower (3.25 vs 25hours) in the VEDP group, both for device implantations (P<.001) and for electrophysiology procedures (P <.001). There were no statistically significant differences in the total number of complications (4 vs 6), even when we distinguished between acute complications and those occurring within the first 30 days after discharge. Four patients in the VEDP underwent pacemaker implantation and atrioventricular node ablation in the same procedure. More ablations were performed in the SP (100 vs 70, P=.046). One VEDP patient required admission due to tamponade in the context of ablation of right ventricular outflow tract extrasystole, and another required repositioning of an atrial lead, which was performed at the end of the day; the patient was discharged on the same afternoon as the procedure. Among patients undergoing de novo implantation, those in the VEDP group were slightly younger (72 vs 75 years, P=.003), and there were more women in the SP group (22.4% vs 37.3%, P <.001).
Characteristics of the patients and results
| 2022 | 2018-2019 | ||
|---|---|---|---|
| Total number ambulatory procedures | 230 | 221 | |
| VEDP | SP | P | |
| Number | 185 (80.4) | 189 (85.5) | ns |
| Age, y | 63 [50.5-76] | 64 [52-75] | ns |
| Women | 62 (33.5) | 81 (42.8) | <.001 |
| Hours after discharge | 3.5 [2.5-4.13] | 24 [22.8-25.5] | <.001 |
| Puncture number | 2 [1-2] | 2 [2-3] | ns |
| Electrophysiology | |||
| Number | 89 | 106 | |
| Age, y | 56 [44-68] | 54 [43-65.5] | ns |
| Female sex | 40 (44.9) | 50 (47.1) | ns |
| Hours after discharge | 3.75 [3-4.25] | 23.5 [22.3-25] | <.001 |
| Puncture number | 2 [2-3] | 2 [2-3] | ns |
| Diagnostic only | 19 (21.3) | 6 (5.6) | .046 |
| Therapeutic | 70 (78.7) | 100 (94.4) | .046 |
| IRT ablation | 27 (30.3) | 36 (34) | ns |
| Accesory pathway ablation | 9 (10.1) | 16 (15.1) | |
| AT ablation | 1 (1.1) | 2 (1.9) | |
| AV node ablation | 4 (4.5) | 2 (1.9) | |
| AF RF ablation | 3 (3.4) | 0 (0) | .001 |
| CVT isthmus ablation | 19 (21.4) | 36 (34) | .002 |
| VT/VE ablation | 7 (7.9) | 6 (5.7) | ns |
| Devices | |||
| Number | 98 | 83 | |
| Age, y | 72 [58.3-78.8] | 75 [66.5-80] | .03 |
| Female sex | 22 (22.4) | 31 (37.3) | <.001 |
| Hours after discharge | 3.25 [2.38-4] | 25 [23.3-26] | <.001 |
| Puncture number | 2 [1-2] | 2 [1-2] | ns |
| PM single | 15 (15.3) | 28 (33.7) | <.01 |
| PM single physiologic pacing | 3 (3) | 0 (0) | |
| PM dual | 36 (36.7) | 35 (42.2) | |
| PM dual physiologic pacing | 5 (5.1) | 1 (1.2) | |
| CRT-P | 2 (2) | 2 (2,4) | |
| ICD single | 22 (22.4) | 11 (13.2) | |
| ICD dual | 7 (7.1) | 1 (1.2) | |
| CRT-D | 10 (10.2) | 5 (6) | |
| Antithrombotic treatment | |||
| OAC | 58 (31.4) | 66 (34.9) | ns |
| APT | 39 (21.1) | 31 (16.4) | |
| Dual APT | 7 (3.8) | 5 (2.6) | |
| OAC+APT | 4 (2.2) | 6 (3.2) | |
| Complications | |||
| Total | 4 (1.7) | 6 (2.6) | ns |
| Devices | 2 (1.01) | 2 (1) | |
| EP | 1 (0.5) | 4 (2.1) | |
| Acute (predischarge) | |||
| Atrial lead dislogement | 1 (0.5) | ns | |
| Neumothorax | 1 (0.5) | ||
| Tamponade | 1 (0.5) | ||
| APE during VT ablation | 1 (0.5) | ||
| After discharge until day 30 | |||
| ICD infection | 1 (0.5) | ns | |
| Pocket bleeding | 1 (0.5) | ||
| Pericarditis | 2 (1) | ||
| AVB postablation | 1 (0.5) | ||
APE, acute pulmonary edema; AF, atrial fibrillation; APT, antiplatelet therapy; AT, atrial tachycardia; AVB, atrioventricular block; AVN, atrioventricular node; CRT, cardiac resynchronization therapy; CRT-D, CRT-Defibrillator; CRT-P, CRT-pacemaker; CVT, cavotricuspid isthmus; Dual, dual-chamber; ICD, implantable cardioverter-defibrillator; IRT, intranodal reentrant tachycardia; OAC, oral anticoagulation; PM, pacemaker; PVC, premature ventricular contraction; RF, radiofrequency; Single, single-chamber; SP, standard protocol; VE, ventricular extrasystole; VEDP, very early discharge protocol; VT, ventricular tachycardia.
The protocol avoided 184 days of hospital stay (20.4 days per month) and could be applied to 80.4% of all patients referred to our unit for invasive procedures. Very few patients undergoing redo cryoablation for atrial fibrillation were included in the first group and therefore we were unable to assess the safety of the protocol in that context.
In conclusion, these results suggest that the VEDP for outpatients undergoing de novo implantation of cardiac stimulation devices or electrophysiology studies in an electrophysiology laboratory is safe and efficient in selected patients, without the support of a day hospital.
FUNDINGNo funding has been received for this work.
AUTHORS’ CONTRIBUTIONSL. Álvarez-Acosta and J. Hernández-Afonso conceived the study. All authors verified the analytical methods. J. Hernández-Afonso and P. Ruiz-Hernández encouraged L. Álvarez-Acosta to make the comparison with a prior cohort and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
CONFLICTS OF INTERESTNone of the authors have any conflicts of interest related to this article.