The concept of interatrial block (IAB), established by consensus in 2012, is defined as prolonged P wave duration (≥120ms) due to delayed transmission of the sinus impulse through the region of the Bachmann bundle.1 IAB is classified as partial (P wave≥120ms) or advanced (P wave≥120ms with biphasic morphology in the II-III-aVF leads). Atypical patterns of advanced IAB have been described, but their frequency and clinical significance are unknown.2 The aims of this study were to determine the prevalence of the various IAB patterns (partial, typical advanced, and atypical advanced) in the general population,3 in centenarians,4 in patients with heart failure,5 and in patients undergoing cavotricuspid isthmus ablation for atrial flutter,6 and to evaluate associations between these patterns and atrial fibrillation (AF) or stroke.
Data from 4 studies3–6 were evaluated. These included 240 individuals from the general population who participated in a case-control study (n=80 and n=160, respectively) to analyze the relationship between IAB and AF,3 60 centenarians,4 464 patients with heart failure,5 and 110 patients undergoing cavotricuspid isthmus ablation to treat atrial flutter.6 All 4 studies had been approved by their respective local ethics committees and the participants signed an informed consent form.
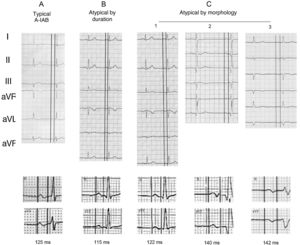
In each study, researchers performed a standardized analysis of the patients’ electrocardiograms. The following IAB patterns were defined2 (figure 1):
- 1.
Normal P wave: duration <120ms and normal morphology.
- 2.
Partial IAB: duration≥120ms and absence of the final negative component of the P wave in the inferior leads.
- 3.
Advanced IAB:
- •
Typical: duration≥120ms and P wave with biphasic morphology in II-III-aVF.
- •
Atypical by morphology:2
- -
Type 1: duration≥120ms and P +/– in III-aVF with an isodiphasic component in lead II in the terminal portion (+/0). This occurs because the final part of atrial activation in the P loop is around –30°, at the limit of the positive or negative hemifield of lead II.
- -
Type 2: duration ≥ 120ms and P +/– in III-aVF with P +/–/+ in II. Similar to type 1. It occurs because the final part of atrial activation in the P loop is around –30°, but at the end it rotates clockwise and passes from the negative to the positive hemifield of II.
- -
Type 3: duration ≥ 120ms and P +/– in II and P negative in III and aVF, but with an isodiphasic component in III-aVF in the first part (0/–). This occurs because the onset of atrial activation has an axis between 0 and –30°.
- •
Atypical by duration:2 duration <120ms but P +/– in II-III-aVF.
The mean age of the participants was 74 years in the general population group, 101 years in the centenarian group, and 65 to 67 years in the heart failure and atrial flutter ablation groups. Men accounted for 70% to 78% of participants in all groups except the centenarian group, in which 70% were women.
In the series studied, 40% to 50% of participants had a normal P wave, except the centenarians (32%). Atypical advanced IAB occurred in 5.6% (95% confidence interval [95%CI], 3.0%-10.4%) of the general population controls, 25.0% (95%CI, 15.8%-37.2%) of the centenarians, 16.8% (95%CI, 13.7%-20.5%) of heart failure patients, and 6.4% (95%CI, 3.1%-12.6%) of patients with atrial flutter (table 1). These prevalence values were similar to those of typical advanced IAB in all the groups. The most common form of atypical advanced IAB was type 1 morphology.
Prevalence of the various types of interatrial block in the studies analyzed
| Study | Participants | NormalP wave | Partial IAB | Advanced typical IAB | Advanced atypical IAB | |||
|---|---|---|---|---|---|---|---|---|
| By morphology | By duration | |||||||
| Atypical 1 | Atypical 2 | Atypical 3 | ||||||
| General population (REGICOR)Age: 74 yMen: 70.0% | n=80Atrial fibrillation | 26.3% (17.9-36.8)(n=21) | 62.5% (51.6-73.3)(n=50) | 7.5% (3.5-15.4)(n=6) | 2.5% (0.7-8.7)(n=2) | 1.25% (0.2-6.8)(n=1) | 0% (0-4.6)(n=0) | 0% (0-4.6)(n=0) |
| n=160Controls | 44.4% (36.9-52.1)(n=71) | 46.9% (39.3-54.6)(n=75) | 3.1% (1.4-7.1)(n=5) | 5.0% (2.6-9.6)(n=8) | 0.6% (0.1-3.5)(n=1) | 0% (0-2.3)(n=0) | 0% (0-2.3)(n=0) | |
| General population (centenarians)Age: 101 yMen: 30.0% | n=60 | 31.7% (21.3-44.2)(n=19) | 26.7% (17.1-39.0)(n=16) | 16.7% (9.3-28.0)(n=10) | 15.0% (8.1-26.1)(n=9) | 1.7% (0.3-8.9)(n=1) | 1.7% (0.3-8.9)(n=1) | 6.7% (2.6-15.9)(n=4) |
| Heart failureAge: 65 yMen: 70.9% | n=464 | 50.6% (46.1-55.2)(n=235) | 20.5% (17.1-24.4)(n=95) | 12.1% (9.4-15.4)(n=56) | 10.1% (7.7-13.2)(n=47) | 0.9% (0.3-2.2)(n=4) | 0.4% (0.1-1.6)(n=2) | 5.4% (3.7-7.8)(n=25) |
| Atrial flutter ablationAge: 67 yMen: 78.1% | n=110 | 38.2% (29.7-47.5)(n=42) | 50.0% (40.8-59.2)(n=55) | 5.5% (2.5-11.4)(n=6) | 3.6% (1.4-9.0)(n=4) | 0.9% (0.2-5.0)(n=1) | 0.9% (0.2-5.0)(n=1) | 0.9% (0.2-5.0)(n=1) |
IAB, interatrial block
The relationship between these IAB patterns and the risk of AF or stroke was analyzed in patients with heart failure. The various types of atypical block by morphology were grouped into a single category because of the small number of cases. In heart failure patients, the presence of typical advanced IAB or atypical advanced IAB by morphology was associated with a similarly increased risk of AF (respectively, hazard ratio [HR], 2.06; 95%CI, 0.96-4.43, and HR, 1.96; 95%CI, 0.96-3.92) and stroke (HR, 2.96; 95%CI, 0.67-13.01, and HR, 2.82; 95%CI, 0.74-10.79). These results indicate that atypical advanced IAB is a risk factor for AF or stroke in these patients in the same manner as typical advanced IAB.
Among the limitations of this analysis (in addition to those of each study), we mention the heterogeneity of the study designs, the interobserver variability in determining atypical IAB patterns, and the differences in the follow-up times and methods used in the studies.
In conclusion, atypical advanced IAB is as frequent as typical advanced IAB, and it occurs most often as type 1 by morphology. Our results indicate that the prevalence of this condition increases with age and the presence of heart failure. In heart failure patients, atypical advanced IAB by morphology is associated with an increased risk of AF and stroke, similar to that of typical advanced IAB.
FUNDINGThe studies included received funding from Instituto de Salud Carlos III (PI071218, PI081327, CIBERCV CB16/11/00246, CB16/11/00292, CB16/11/00403], and funding support for research groups from the Generalitat de Catalunya [SGR 2014-1195], the Ministry of Education and Science (SAF2014-59892), TV3 Fundació La MARATÓ (201502, 201516), and AdvanceCat 2014-2020, Clinical Registry Project of the Clinical Cardiology Section of 01/2013, Spanish Society of Cardiology.
AUTHORS’ CONTRIBUTIONSDefinition of the objectives and study design (R. Elosua, M. Martínez-Sellés, A. Baranchuk, A. Bayés-de-Luna), data collection (LA Escobar-Robledo, A. Massó-van Roessel), data analysis (R. Elosua), interpretation of the results (R. Elosua, L.A. Escobar-Robledo, A. Massó-van Roessel, M. Martínez-Sellés, A. Baranchuk, A. Bayés-de-Luna), writing of the first draft (R. Elosua, A. Bayés-de-Luna), critical review of the manuscript and approval of the final version, as well as availability to answer questions related to the validity and integrity of the data and the study (R. Elosua, L.A. Escobar-Robledo, A. Massó-van Roessel, M. Martínez-Sellés, A. Baranchuk, A. Bayés-de-Luna).
CONFLICTS OF INTERESTThe authors declare that they have no conflicts of interest.