Hyponatremia (plasma sodium =135 mEq/L) is one of the most common electrolyte abnormalities in patients with acute heart failure (HF) and is considered a marker of poor prognosis.1
The latest European Society of Cardiology, Guidelines for HF included tolvaptan, a vasopressin V2-receptor blocker that inhibits free water reabsorption,2 as a valid treatment for patients with refractory hyponatremia.3
We present our experience with tolvaptan for the treatment of refractory hyponatremia in patients admitted by HF.
A retrospective study was conducted in patients treated with tolvaptan who were admitted for HF between February 2011 and August 2012 with refractory hyponatremia (sodium <135mEq/L despite “classic” treatment, mainly fluid intake restrictions and/or administration of hypertonic saline solution) and persistent symptoms of HF.
Plasma sodium, potassium, and creatinine concentrations, glomerular filtration rate (calculated by the Modification of Diet in Renal Disease equation), weight, and excretion rhythm at the start of tolvaptan therapy were assessed 24h and 48h after tolvaptan was given.
The ESTATA/SE 11.1 software package was used for the statistical analysis.
A total of 30 patients (57% women; mean age, 72±14 years) were included. The most common cause of HF (33% of all patients) was ischemic heart disease; 54% of patients presented ventricular dysfunction (mean ejection fraction, 48%±16%). All were following optimal treatment for HF and all were receiving diuretic therapy at home.
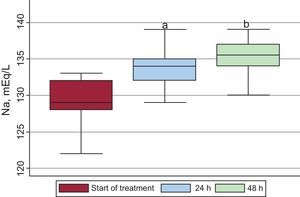
Treatment was started at a daily dose of 15mg of tolvaptan in 90% of patients and 30mg in all others. At the start of treatment, sodium was 129±3mEq/L. Natremia was significantly increased at 24h, an effect that persisted at 48h (129±3mEq/L at baseline; 134±3mEq/L at 24h; 135±3mEq/L at 48h; P<.001) (Fig. 1). No significant changes were observed in potassium concentrations after the drug was administered (4±0.5mEq/L at baseline; 4±0.4mEq/L at 24h; 4.2±0.4mEq/L at 48h; P>.05).
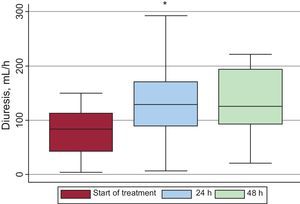
After treatment, diuresis was significantly increased at 24h, and the effect was maintained at 48h (80±45mL/h, 138±60mL/h, and 136±64mL/h, respectively; P<.001) (Fig. 2). Likewise, a significant decrease in patient weight was observed at 48h (67.1±17.8kg vs 64.1±15.1kg; P=.01).
No statistically significant differences were observed in creatinine (1.3±0.5mg/dL at baseline; 1.4±0.4mg/dL at 24h; 1.6±1.1mg/dL at 48h; P>.05) or Modification of Diet in Renal Disease (54±20, 50±16, and 50±18mL/min/1.73m2, respectively; P>.05).
Patients who presented moderate-to-severe hyponatremia (sodium <130 mEq/L) showed a larger post-treatment increase in natremia and excretion rhythm than those who presented mild hyponatremia. These results were similar in patients with ventricular dysfunction or HF with preserved systolic function.
The only adverse event occurred in a patient with no known renal impairment who experienced acute renal failure while receiving treatment and it resolved without dialysis.
In patients with HF, a significant relationship between natremia and in-hospital mortality was observed, along with an increase in readmissions and long-term morbidity and mortality.1,2
Various mechanisms promote this hyponatremia: increased vasopressin due to low cardiac output and decreased renal blood flow, increased perception of thirst, and the use of diuretics.
In patients admitted to our hospital for HF and refractory hyponatremia, we observed a significant increase in the natremia after tolvaptan therapy. Additionally, patients with lower sodium were those who most benefited from treatment, as shown in other studies.4–6 Our study also observed a significant increase in the excretion rhythm and a decrease in weight without significant decline in kidney function or potassium levels, suggesting, that tolvaptan may be a therapeutic option that can be added to loop diuretics, which already have a hyponatremic effect of their own.
Furthermore, our results show similar effects in patients with or without ventricular dysfunction, an important fact taking into account that the prevalence of hyponatremia is similar in both groups.
Therefore, tolvaptan administration in unselected patients with decompensated HF and symptomatic refractory hyponatremia significantly increases sodium concentrations and excretion rhythm without significantly affecting kidney function.
.