Keywords
INTRODUCTION
Brugada syndrome is characterized by right bundle branch block and ST segment elevation in the right precordial leads on electrocardiography in patients with no structural heart disease, and episodes of syncope or sudden death.1 The electrocardiographic pattern is transient in up to 40% of the cases, and can be unmasked by sodium channel blockers2 such as flecainide. We present the case of a young man with type 1 Brugada ECG pattern that manifested after the intake of a large amount of cocaine.
CASE STUDY
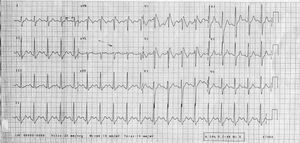
A 22-year-old man with no medical history of interest came to the emergency room for palpitations and perioral paresthesia. In the previous 6 hours, he had consumed about 600 mg of cocaine. Blood pressure was 130/80 mm Hg and Sat O2, 98%. The physical examination was unremarkable. The electrocardiogram (ECG) showed sinus rhythm at 115 bpm, complete right bundle branch block, and ST segment elevation of more than 2 mm in V1-V3 (Figure 1). The chest x-ray was normal. The general analyses, including ion assay, showed no alterations, with the urinalysis positive for cocaine.
Figure 1. 12-lead electrocardiogram after cocaine consumption. Type 1 Brugada ECG pattern.
Lorazepam was administered and the patient was kept under observation until the clinical symptoms had abated, after which time he was referred to the arrhythmia section for further study.
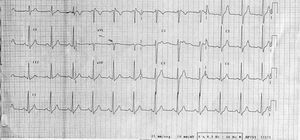
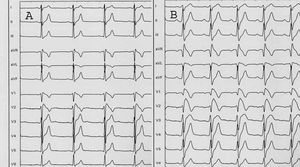
Follow-up ECG showed sinus rhythm and right bundle-branch block, but the findings did not meet the criteria for Brugada syndrome (Figure 2). On the basis of suspected Brugada syndrome, a flecainide test (2 mg/kg intravenous) was performed with positive results (Figure 3). Since the patient had no personal or family history of syncope, documented arrhythmia, or sudden death, an electrophysiological study (EEF) was done; however, ventricular arrhythmia could not be induced and therefore there was no indication for an automatic defibrillator or other specific treatment, except for discontinuation of cocaine consumption. The patient required outpatient follow-up.
Figure 2. 12-lead electrocardiogram at baseline.
Figure 3. Electrocardiogram before administration of flecainide (A). Electrocardiogram after administration of flecainide. Positive pharmacological test (B).
In a subsequent study of near relatives, the father's ECG showed right bundle branch block, but without the criteria defining a Brugada pattern. A flecainide test and EEF were also done, both with negative results.
DISCUSSION
Brugada syndrome is a genetically determined disease caused by mutations in the sodium channels (SCN5A) coded in chromosome 3.2 A decrease in these channels determines a voltage gradient between the epicardium and the ventricular endocardium, with prolongation of the action potential and repolarization dispersion in the epicardium, leading to a high vulnerability for the development of reentry ventricular arrhythmia.3
Two potential electrocardiographic patterns were initially included: coved or type 1 pattern and saddle-back or type 2 pattern. The diagnosis can be difficult in up to 40% of cases because the electrocardiographic pattern often shows transient normalization.2 Furthermore, a negative pharmacological challenge test using conventional leads does not rule out the possibility of Brugada syndrome, making it necessary to routinely include precordial leads in the second and third intercostal spaces.4 In our patient, the onset of a type 1 Brugada ECG pattern coincided with the effects of cocaine, and the pattern repeated during the flecainide test. At baseline the patient presented a type 2 pattern. This variable morphology can be explained by the fact that cocaine,5 as occurs with flecainide, produces sodium channel blocking. The action of sodium channel blockers on already abnormal channels can enhance the changes and unmask the electrocardiographic pattern.2
It is interesting to highlight the dynamic nature of the electrocardiogram changes, in which the patterns of the syndrome may not be evident and can hinder the diagnosis.
Literature references to cases in which the Brugada pattern is manifested by cocaine use are scanty6,7 and in all cases, subsequent pharmacological challenge tests were negative and Brugada syndrome could not be diagnosed; hence, the electrocardiogram changes were attributed solely to the action of cocaine. This case is of interest due to the lack, as far as we are aware, of previous reports in the literature describing unmasking by cocaine of Brugada syndrome later demonstrated by a positive flecainide test. Careful ECG assessment is necessary in patients who come to the Emergency Room for cocaine use, since this will allow adequate cardiological assessment among patients diagnosed as having a Brugada pattern.
Received October 13, 2004.
Accepted for publication March 18, 2005.
Correspondence: Dra. B. Daga.
Servicio de Cardiología. Hospital Clínico Universitario Lozano Blesa.
Avda. San Juan Bosco, s/n. 50009 Zaragoza. España.
E-mail: berthadagha@yahoo.es