We describe a 57-year-old man with Child-Pugh class B chronic cirrhosis of the liver disease due to alcoholism and portal hypertension as well as ascites, hypersplenism, and grade III esophageal varices. The liver transplant evaluation revealed severe, symptomatic aortic stenosis with preserved systolic function; hence, transplantation was contraindicated. Because the patient was at high surgical risk due to his severe liver disease and comorbidities, surgical replacement of the aortic valve was ruled out. A CoreValve No. 31 aortic valve was implanted percutaneously; persistent third-degree atrioventricular block subsequently appeared and the patient required a dual-chamber pacemaker.
Three months later, the patient was hospitalized for bacteremia and pancytopenia secondary to hypersplenism. While admitted, he underwent colonoscopy with polypectomy, but experienced lower gastrointestinal bleeding that required blood transfusion.
During follow-up, the patient experienced several episodes of paroxysmal atrial fibrillation that were treated with amiodarone. The risks and benefits of anticoagulation therapy were assessed (CHA2DS2-VASc=1; HAS-BLED=3), antiplatelet therapy with clopidogrel was prescribed, and percutaneous closure of the left atrial appendage (LAA) was scheduled.
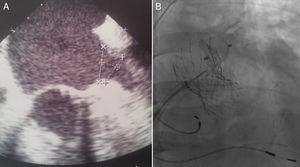
The patient's history of esophageal varices was a relative contraindication for procedural guidance using transesophageal echocardiography (TEE).1 Consequently, a decision was made to use endoscopic ultrasound guidance. A Pentax EG-3870UTK endoscope coupled to a Hitachi HI Vision Avius console with a frequency of 7.5 MHz was used. Under mild sedation in the interventional cardiology room, an Amplatzer Cardiac Plug No. 22 LAA closure device was implanted with no complications. Endoscopic ultrasound allowed direct visualization of the esophagus and esophageal varices and confirmed that there was no bleeding or other adverse events (Figure 1). The technique also allowed optimal visualization of the atrial appendage during the device implantation (Figure 2A) and, together with angiography (Figure 2B), confirmed the successful final outcome by Doppler ultrasound.
The patient was discharged with clopidogrel, as it is less likely to affect the gastrointestinal tract. The successful outcome was confirmed at 1 month by endoscopic ultrasound. Twelve months later, the patient was stable and had experienced no thromboembolic or hemorrhagic events.
Atrial fibrillation affects 3.8 million patients in Europe and causes 15% to 20% of all ischemic strokes.2 More than 90% of cardiac embolisms originate in the LAA. Accordingly, the European Society of Cardiology Clinical Practice Guidelines3 state that percutaneous LAA closure is an option for patients at thromboembolic risk who cannot be treated with long-term oral anticoagulant therapy.
To guide the LAA closure procedure, some groups use intracardiac echocardiography or angiographic control, but most hospitals use TEE.4
Intracardiac echocardiography is extremely useful for guidance in interventional procedures involving cardiac structures and has been evaluated for LAA examinations, in particular to rule out intracavitary thrombi.5 However, the standard views (right atrium, coronary sinus, distal right ventricular outflow tract) do not always allow full visualization of the LAA. For this reason and because TEE was contraindicated in our patient, we decided to use endoscopic ultrasound as an alternative imaging technique. Furthermore, unlike other ultrasound systems, such as TEE, 3D-TEE, and endoscopic ultrasound, intracardiac echocardiography uses consumable items, which may raise the costs associated with the technique.
Endoscopic ultrasound is a diagnostic and therapeutic method used in digestive procedures, such as cholangiopancreatography, gastrointestinal tumor staging, and the treatment of pancreatic cystic lesions, subepithelial lesions, and gastric varices. It has a distal ultrasound transducer that runs at frequencies of 5 to 20 MHz, with penetration-depth and resolution variables that allow highly precise real-time imaging of the digestive tract wall, surrounding organs, and blood vessels. The endoscopic ultrasound probe is equipped with color Doppler ultrasound, pulsed Doppler, and elastography (software used to assess fibrotic tissues), but has the drawback that it is a monoplanar device. In patients at high risk of esophageal bleeding, in whom TEE is contraindicated, endoscopic ultrasound may be a safer option for LAA closure procedural guidance because any of the rare complications that may occur are immediately identified during the procedure.6 Clinical trials support its use in gastrointestinal hemorrhage situations in patients with esophageal varices, although the use of the technique has not been previously described for the specific evaluation of cardiac structures or as a technique to guide interventional cardiovascular procedures.