We read with great interest the article by Zamora et al.,1 in which they estimated the number of patients eligible for proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors. We thought it particularly interesting that, although they found a relatively low percentage of patients with cardiovascular disease to be eligible for these drugs, this patient group had the highest absolute number of eligible patients. We consider these results to be highly relevant to clinical practice, as they show that 19.8% of patients with cardiovascular disease met the criteria to receive PCSK9 inhibitors based on a low-density-lipoprotein cholesterol (LDL-C) level > 100mg/dL despite maximal lipid-lowering therapy.
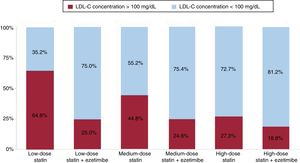
We estimated the percentage of patients that would be eligible for PCSK9 inhibitors based on LDL-C levels > 100mg/dL despite maximal lipid-lowering therapy in the 1281 patients with cardiovascular disease in the REPAR Study (Registro Paciente de Alto Rieso Cardiovascular; in English, the High-Cardiovascular-Risk Patient Registry). This registry previously demonstrated that treatment with high-dose statins was associated with improved LDL-C control,2 although this was only achieved in less than 40% of patients. In the group of patients with established cardiovascular disease (91% of whom had ischemic heart disease), 33.6% of patients were receiving high-dose statins and 5.4% were receiving high-dose statins plus ezetimibe. As can be seen in Figure 1, the percentage of patients with LDL-C > 100mg/dL despite taking high-dose statins with or without ezetimibe was 27.3% and 18.8%, respectively; this percentage was 44.8% and 24.6% in patients who were receiving medium-dose statins with or without ezetimibe, respectively.
Dyslipidemia remains one of the most poorly-controlled factors in patients with established cardiovascular disease.3,4 Treatment with high-dose statins has been demonstrated to be effective in controlling LDL-C and reducing the incidence of cardiovascular complications5; combined treatment with ezetimibe also improves LDL-C control and prognosis.5 However, a large percentage of patients do not meet LDL-C treatment target levels despite maximum-dose treatment.2–4 Poor control may also be attributed to additional factors such as low treatment adherence, an effect that cannot be excluded in our analysis. PCSK9 inhibitors are a new treatment option that has been demonstrated to be safe and effective for LDL-C control and that reduces the incidence of cardiovascular complications.6 The data from both the study by Zamora et al.1 and the REPAR Study provide evidence that there is a high percentage of patients with established cardiovascular disease who are eligible for PCSK9 inhibitors after optimization of lipid- lowering therapy and lifestyle factors.
The REPAR Study received an unconditional grant from Ferrer laboratories, Spain.