We report the case of a 50-year-old woman who presented to the emergency department with dyspnea and no known history except for a recent microdiscectomy for a herniated right L4-L5 lumbar disc. A week after surgery, she developed progressive dyspnea, even on minimal exertion. There were also signs of peripheral congestion and orthopnea.
On physical examination, the patient was hemodynamically stable. Notable findings were jugular venous distension, the Kussmaul sign, a pronounced carotid pulse, and a systolic murmur in the aortic pulmonary area with a split S2 and bibasilar crackles. Palpation revealed a soft abdomen and an abdominal murmur with no pain or palpable masses. Pitting edema was visible up to the pretibial region on the lower extremities.
Laboratory tests showed elevated D-dimer (4183ng/mL) and N-terminal fragment of brain natriuretic peptide (NT-proBNP) (995pg/mL) levels. There was blunting of both costophrenic sinuses on chest radiography. The electrocardiogram showed sinus tachycardia (110bpm), while bedside cardiac ultrasound showed slightly dilated right cavities with normal functioning, although we could not rule out an ostium secundum-type atrial septal defect. There were no signs of heart valve disease or pericardial effusion. Given the elevated D-dimer levels, computed tomography of the pulmonary arteries was performed to rule out pulmonary thromboembolism.
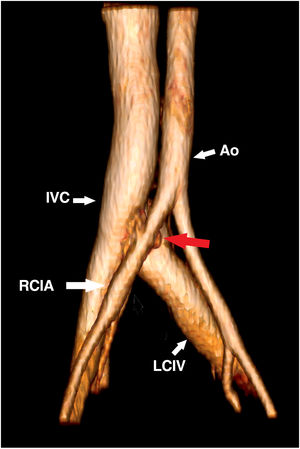
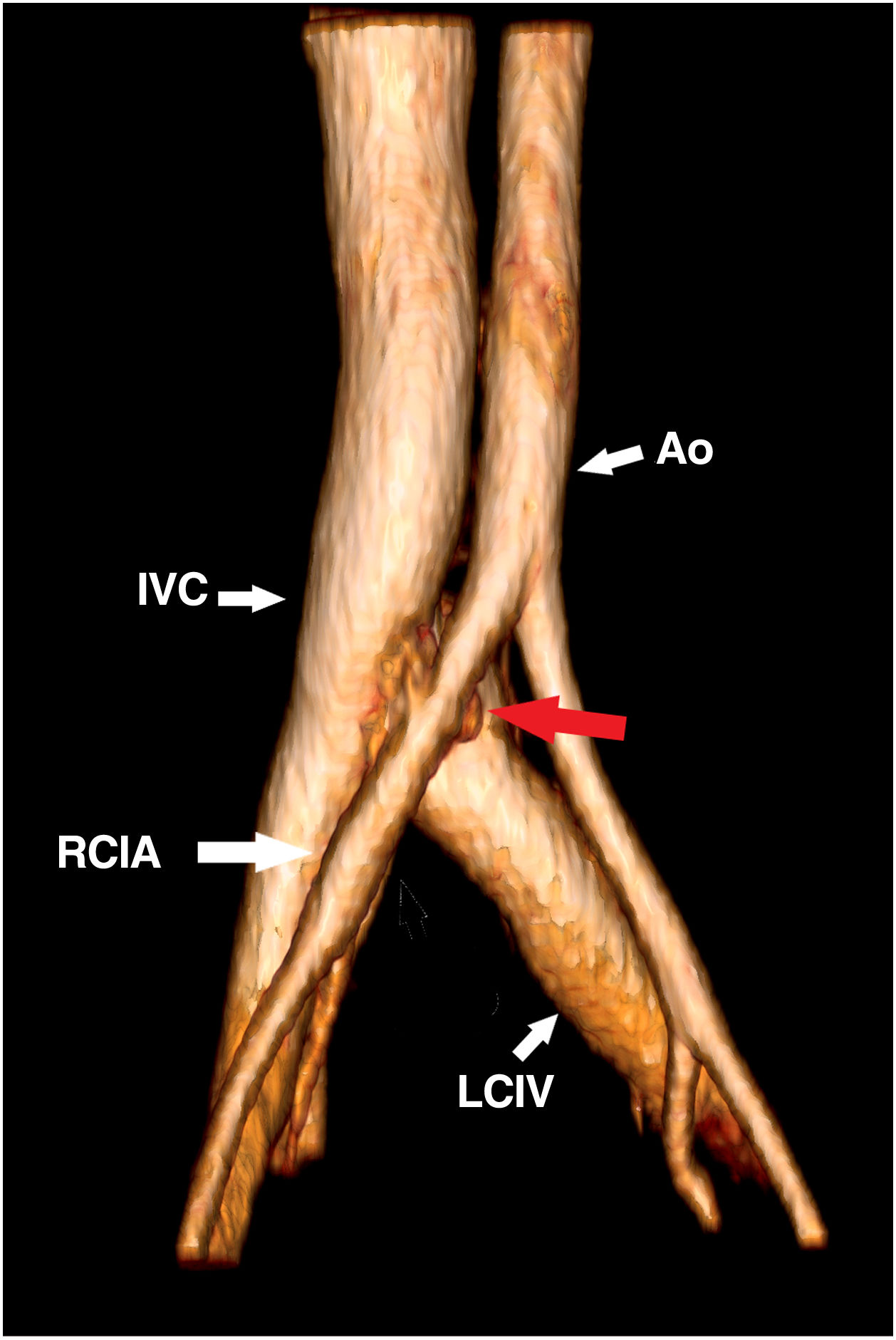
The initial clinical diagnosis was a decompensated atrial septal defect following lumbar surgery. The patient underwent a complete transthoracic and transesophageal echocardiographic examination, which ruled out this defect and showed normal cavities. The only other significant finding was high estimated cardiac output (8.9L/min). Considering the above, a tentative diagnosis of high-output heart failure was considered. Right heart catheterization showed a mean pulmonary artery pressure of 29mmHg, a right atrial pressure of 10mmHg, a right ventricular pressure of 4mmHg, and a pulmonary capillary pressure of 18mmHg. Multilevel venous blood gas sampling revealed an inferior vena cava oxygen saturation of 88%, indicating a possible arteriovenous shunt in the lower body. Computed tomography angiography of the aorta (figure 1) showed a right ilio-iliac arteriovenous fistula (AVF) caused by perforation of the anterior part of the annulus fibrosus and the common vertebral ligament during curettage of the disc space, which extended as far as the retroperitoneal vascular structures. The injury probably did not affect the entire vascular wall, but would have led to the formation of the AVF. There were 2 treatment options: endovascular surgery or classic open surgery. We chose endovascular surgery, as it is a less invasive procedure that is widely used at our hospital.
The patient progressed favorably. She remained asymptomatic, was discharged, and is currently in New York Heart Association functional class I. Informed consent was obtained for the publication of this case report.
Dyspnea is a common symptom and the differential diagnosis is therefore broad. High-output HF is a rare condition with uncertain prevalence.1,2 It is characterized by high cardiac output, low systemic vascular resistance (due to peripheral vasodilation or, as in this case, an AVF), and a low arteriovenous oxygen difference. Its most common causes are listed in table 1.
Most common causes of high-output heart failure2
| Cause | Frequency, % | Symptoms | Signs | Specific treatment |
|---|---|---|---|---|
| Obesity | 31 | Dyspnea, tachycardia | Body mass index >30 | Lifestyle and pharmacological measures, bariatric surgery |
| Liver cirrhosis | 23 | Asthenia, increased waist circumference, dyspnea | Alcohol abuse, viral hepatitis, obesity, autoimmune diseases, abdominal distention, mucocutaneous jaundice, gastrointestinal bleeding | Liver transplant, dual treatment with antiminerals or corticosteroids and loop diuretics |
| Arteriovenous shunts | 23 | Dyspnea, orthopnea, edema, palpable thrills, murmur over AVF | Hereditary hemorrhagic telangiectasia with mucocutaneous or gastrointestinal bleeding episodes. History of surgery in the case of iatrogenic AVF | In the case of congenital AVF, treatment of underlying cause (medical treatment, invasive or surgical embolization) In the case of acquired AVF, surgical or percutaneous closure or reduction |
| Pulmonary diseases | 16 | Dyspnea, wheezing | COPD, bronchiolitis, bronchiectasis, interstitial diseases | Aerosol therapy, noninvasive ventilation, mucolytics |
| Myeloproliferative disease | 8 | Tiredness, dyspnea | Fever, increased periods of bleeding, splenomegaly, peripheral blood smear abnormalities | Chemotherapy, hematopoietic stem cell transplant |
| Hyperthyroidism | Variable, not recorded in studies | Tachycardia, palpitations, dyspnea | Fever, tremor, hyperreflexia, hyperactivity, goiter | Antithyroid hormones, radiotherapy, surgery |
| Sepsis | Variable, not recorded in studies | Tachycardia, tachypnea, warm well-perfused extremities | Fever, chills, fatigue, loss of appetite, palpitations, altered mental status | Life support, targeted antibiotic therapy |
| Anemia | Not recorded in studies | Tachycardia, asthenia | Mucocutaneous pallor, external bleeding, pain due to expanding hematoma, brain fog | Specific treatment of cause, iron replacement |
| Beriberi | Not recorded in studies | Dyspnea, orthopnea, palpitations, peripheral edema with burning pain | Malnutrition, alcoholism | Thiamine replacement for at least 2 weeks |
| Paget disease | Not recorded in studies | Osteoarthritic pain, neuropathy | Bone deformation, sensory and motor deficit in cases of spinal cord involvement | Bisphosphonates |
AVF can be congenital or acquired. Acquired AVF secondary to lumbar disc surgery is uncommon, with some series reporting a prevalence <0.04%.3,4
The most common clinical manifestations are abdominal murmur, dyspnea, tachycardia, edema of the lower extremities, and jugular venous distention. If the fistula causes a notable shunt, the Water-Hammer pulse is normal and similar to that seen in aortic insufficiency. In addition, the extremities are often well perfused and warm due to peripheral vasodilation.
A detailed history and thorough physical examination are essential for diagnosis. Analytical data such as NT-proBNP and high-sensitivity troponin I levels and echocardiographic findings are useful. Right heart catheterization with invasive measurement of cardiac hemodynamics has been recommended for patients with clinical heart failure and echocardiographic findings consistent with indirectly assessed high cardiac output.1 High-output heart failure has traditionally been defined as symptoms in the context of a cardiac index >4L/min/m2 or a cardiac output >8L/min.1
Finally, it is important to treat the heart failure symptoms and the underlying cause. Surgical or endovascular repair is the definitive treatment for acquired AVF, as when performed early it reverses cardiac remodeling.1
Heart failure with preserved ejection fraction was included in the differential diagnosis, as it can be caused by high cardiac output. It is rare and usually has a reversible trigger (eg, anemia, high cell turnover, previous treatment). A high index of clinical suspicion and appropriate use of multimodal imaging combined with invasive diagnostic and therapeutic techniques are important.
FundingNone
Authors’ ContributionsA.B. Rojas Brito is the lead author of this article. S.C. Huerta edited and oversaw the article and was involved in diagnosing the patient. E.D. Pérez Nogales and B. Saiz Udaeta were involved in diagnosis and treatment. J.M. Rubio García prepared the 3-dimensional volume reconstruction.
Conflicts of InterestNone.