Although the prognosis of chronic thromboembolic pulmonary hypertension (CTEPH) is poor, its survival has been improved by thromboendarterectomy surgery and balloon pulmonary angioplasty (BPA). Clinical practice guidelines1 and consensus documents2 state that BPA should be performed in high-volume expert centers to guarantee good outcomes and a low rate of complications. In Spain, these criteria are met by just 2 expert centers, services, and units (RCSUs), designated in 2015 by the Spanish Ministry of Health for this disease.3 The objective of this designation is to guarantee equitable access and high-quality, safe, and efficient care for patients with diseases requiring a high level of specialized care and to therefore concentrate patients in a small number of centers. However, this situation needs to be reconsidered due to the growing demand for this procedure and long waiting times in the RCSUs, the increasing interest of non-RCSU centers in performing BPA, and the long distances travelled by patients from other autonomous communities to the RCSUs. In this regard, the consensus document of the European Respiratory Society proposes that BPA procedures be permitted in nonexpert centers, under the guidance of an expert center.4 Here, we present the results of a pioneering experience that includes the performance of BPA in nonexpert centers through a network protocol coordinated with a referral RCSU.
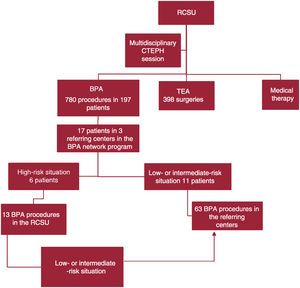
The multidisciplinary CTEPH unit in our RCSU has been a pioneer in Spain in the teaching of the BPA procedure via theoretical and practical courses and training stays in the unit. In addition, a collaborative network program was developed with centers that refer patients to our RCSU and would like to begin conducting BPA in order to enable the referring centers to autonomously perform BPA after a training period overseen by our RCSU. The ultimate aim of this collaboration is to secure uniform therapeutic opportunities for patients with CTEPH, whether they are managed in referring centers or in the RCSU, and to guarantee high-quality and safe treatments. Accordingly, we developed a protocol-based collaborative network program (table 1). The main prerequisite of this program is that all patients be presented in a multidisciplinary session in the RCSU to determine each patient's optimal therapy. If BPA is chosen, any low- or intermediate-risk procedures can be performed in the referring centers after a period of guided training (figure 1). A second precondition of the program is that the “nonexpert” center be equipped with a pulmonary hypertension unit experienced in the diagnosis and pharmacological management of pulmonary hypertension, including the use of drugs with complex administration protocols, as well as experience with the intensive care management of possible BPA-associated complications.
Protocol and results of the pulmonary angioplasty network program
| Protocol for a CTEPH network conducted in collaboration with an RCSU for the development and implementation of a pulmonary angioplasty program in referring centers | |
|---|---|
| Patients indicated for BPA in an RCSU | High-risk patients according to European Society of Cardiology guidelines1Patients requiring intravenous dobutamine or epoprostenol before BPAPatients with high-risk hemodynamic parameters: severely reduced cardiac index ≤ 1.8 L/min/m2 or severely elevated mean pulmonary pressure or pulmonary vascular resistances (≥ 45 mmHg or ≥ 10 WU)Patients with elevated technical complexity (severely dilated and tortuous pulmonary arteries, patients with residual post-TEA pulmonary hypertension) |
| Patients indicated for BPA in a referring center | Patients who, in the initial assessment, do not meet treatment criteria in the RCSUPatients who, after 2 or 3 BPA procedures, transition to low or intermediate risk |
| Prerequisites of the referring center for BPA initiation | Availability of a working unit/group for pulmonary hypertensionPossible implementation of extracorporeal membrane oxygenationAvailability of at least 1 interventional cardiologist with knowledge of the BPA technique and its complications |
| Initiation of BPA instruction in the referring center | Performance of the first 10 BPA procedures under guidance in the referring center |
| Characteristics, complications, and results of the BPA program in the referring centers | ||||||||
|---|---|---|---|---|---|---|---|---|
| BPA performed in an RCSU/BPA in referring center | Patients in the BPA program | Completed/in process/interrupted | Starting year | Complications | Peri-BPA deaths | Other major complications | Reason for BPA | |
| Referring center 1 | 2/30 | 7 patients85% womenMean age, 71 (46-86) y | 6/1/0 | 2017 | 32% of procedures:1 catheter dissection6 hemoptysis episodes (3 in 1 patient)2 mild reperfusion edemas1 femoral hematoma | No | No | • Distal involvement, 3 patients• Distal involvement+comorbidity in 4 patients (> 80 y) |
| Referring center 2 | 6/21 | 6 patients50% womenMean age, 69 (58-78) y | 4/1/1 | 2021 | 27% of procedures: 6 hemoptysis episodes in 2 patients2 catheter/guidewire/balloon dissections1 mild reperfusion edema1 contrast allergy | No | No | • Post-TEA (n=1)• Distal involvement (n=2)• Distal involvement and high surgical risk (n=3) |
| Referring center 3 | 5/12 | 4 patients50% womenMean age, 79 (77-86) y | 3/1/0 | 2021 | 8% of procedures: 1 hemoptysis due to distal perforation, self-limiting | No | No | • Distal involvement in all 4 patients (2 patients > 85 y) |
| Program results | ||||
|---|---|---|---|---|
| Baseline | End | % improvement, mean (95%CI) | P | |
| Mean pulmonary arterial pressure, mmHg | 46.8±15.1 | 30.2±6.0 | 35.7 (19.2-52.1) | < .001 |
| Pulmonary vascular resistance, WU | 9.6±5.3 | 3.8±1.7 | 60.4 (28.1-92.7) | < .01 |
| Cardiac index, L/min/m2 | 2.1 (1.9-2.4) | 2.6 (2.2-2.8) | 23.8 | .03 |
| NT-proBNP, pg/mL | 1197 (606-3096) | 202 (124-363) | 83.1 | .02 |
| 6-min walk test, m | 308.8±87.2 | 400.0±107 | 29.8 (–0.12 to 69.8) | .10 |
| World Health Organization functional class, % I/% II/% III/% IV | I: 0.0II: 17.7III: 58.8IV: 23.5 | I: 35.3II: 47.0III: 17.7IV: 0.0 | Not applicable | < .01 |
95%CI, 95% confidence interval; BPA, balloon pulmonary angioplasty; NT-proBNP, N-terminal pro-B-type natriuretic peptide; RCSUs, expert centers, services, and units; TEA, thromboendarterectomy.
Currently, this BPA program in referring centers and coordinated with the RCSU is in operation in 3 centers in autonomous communities distinct from that of our RCSU. Interventional cardiologists in these centers underwent a theoretical/practical course on BPA in our RCSU, conducted the first 10 BPA procedures in their centers under the guidance of an interventional cardiologist from the RCSU, and now independently perform low- and intermediate-risk procedures in their centers. The present work has been conducted in accordance with international recommendations on clinical research and has been approved by the ethics committee of our center. Informed consent was obtained from all patients and stored.
All patients included in this BPA network program were presented in a multidisciplinary CTEPH session in our RCSU in which the appropriate therapeutic option was selected for each patient in conjunction with the referring physicians. The first procedures were performed in our RCSU for high-risk patients or those with elevated technical complexity, so that 13 of the 63 procedures were performed in the RCSU while the remainder were performed in the referring centers (figure 1). The results of this program are shown in table 1. The data show similar clinical, hemodynamic, and biomarker improvements to those published for the first 46 patients who underwent BPA in our RCSU.5 The periprocedural complication rate in the referring centers was also similar to or lower than that described for our RCSU series.5 All complications were mild (table 1), with no periprocedural deaths, confirming that the network BPA program is safe for patients.
In conclusion, the preliminary results indicate the feasibility of this novel network protocol for CTEPH, which includes the performance of pulmonary angioplasty in nonexpert centers and conducted in a network coordinated with the referral RCSU for low- and intermediate-risk patients. The preliminary results demonstrate that this approach could be safe and effective. This type of tutored pulmonary angioplasty program in referring centers would additionally reduce procedural delays and improve the efficient management of this disease.
FUNDINGThe present work has not been funded by any organization.
ETHICAL CONSIDERATIONSThe present work has been conducted in accordance with international recommendations on clinical research and has been approved by the ethics committee of our center. Informed consent was obtained from all patients and stored. The sex distribution of the population is balanced. Possible sex and gender biases have not been analyzed due to the small sample size.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCEArtificial intelligence has not been used to draft this article.
AUTHORS’ CONTRIBUTIONSM. Velázquez Martín contributed to the conception and drafting of the manuscript. N. Maneiro Melón managed the data analysis and interpretation. A. Gómez Menchero, R. González Ferreiro, and A. Andrés Morist contributed to the data acquisition. P. Escribano Subias contributed to the conception of the work. All authors have performed a critical review of the intellectual content and have approved the final version of the manuscript. Similarly, all authors agree to be accountable for all aspects of the work and to investigate and resolve any questions related to the accuracy or veracity of any part of the work.
CONFLICTS OF INTERESTNone.