Prompt coronary reperfusion is crucial in patients with ST-segment elevation acute coronary syndrome. The aim of this study was to determine factors associated with a delay in seeking medical attention after the onset of symptoms in patients with this condition.
MethodsProspective cohort study in consecutive patients with ST segment elevation infarction. Multiple logistic regression analysis was used to identify factors independently associated with a longer delay in requesting medical help.
ResultsIn total, 444 consecutive patients were included (mean age, 63 years; 76% men, 20% with diabetes). Median total ischemia time was 225 (160-317) minutes; median delay in seeking medical attention was 110 (51-190) minutes. Older patients (age > 75 years; odds ratio = 11.6), women (odds ratio = 3.4), individuals with diabetes (odds ratio = 2.3), and those requesting medical care from home (odds ratio = 2.2) showed the longest delays in seeking medical attention. Lengthy delay was associated with higher in-hospital mortality (9.8% vs 2.7%; P<.005) and 1-year mortality (7.3% vs 2.9%; P<.05) than when attention was promptly solicited.
ConclusionsElderly patients, women, and diabetic individuals with ST-segment elevation myocardial infarction show longer delays in seeking medical attention for their condition. Delays in seeking medical attention are associated with greater in-hospital and 1-year mortality.
Keywords
Despite important healthcare advances and the considerable resources dedicated to improving the clinical outcome of patients with ST-segment elevation acute coronary syndrome (STEACS), this condition remains a major cause of mortality and morbidity in Western countries, including Spain.1–3 There is a clear link between delays in reperfusion treatment and the extent of myocardial necrosis and short- and long-term clinical repercussions of the condition. Thus, patients who benefit most from this treatment strategy are those with a shorter time interval to reperfusion.4,5 Most resources for these patients in coordinated regional care programs are focused on achieving a faster diagnosis, improvements in between- and within-hospital patient transferals, and more generalized use of primary percutaneous coronary interventions (PPCI).6,7 Nonetheless, in Spain, as in other countries, there is little information on factors that lead to delays in the initial medical attention after symptom onset, or the contribution of this time lag to the overall delay before reperfusion.8,9 Previous studies have described several demographic, clinical, and socioeconomic factors associated with delays in prehospital medical attention in STEACS patients.10–14 However, adequate data are lacking on the reasons that determine a delay in seeking medical help. Knowledge of factors associated with a delayed request for medical care may be a key element in the design of strategies to enable faster access to revascularization in high-risk groups, thereby improving their prognosis. The aim of this study was to determine factors associated with a delay in seeking medical attention (DSMA) after the onset of symptoms in patients with STEACS.
METHODSThis is a cohort study with prospective data collection in consecutive patients with a diagnosis of STEACS and an indication for PPCI attended in our hospital over a 3-year period (May 2010-May 2013). Our institution is the referral center for performing PPCI in a catchment population of 608 989 individuals in the Community of Madrid. The entire urban population resides in municipalities of more than 10 000 inhabitants, and the maximum distance to our center is 33 km. Within our publically-funded health care system, initial medical care for these patients can be carried out directly in the patient's home after activation of outpatient emergency services, or by the patient attending a primary care center, a community hospital without PPCI capability, or by going directly to our referral hospital. No specific emergency response network (eg, Infarct Code program) was operating in our area during the study period.
Data Collection and DefinitionsThe timeline data were prospectively obtained from the patients and from registries kept by the emergency services and medical centers where they were attended. Clinical and demographic information was prospectively collected from the clinical reports. The DSMA was defined as the time interval between the onset of symptoms consistent with ischemic heart disease and the first request for medical attention. Data were prospectively collected on the time lapse that occurred to the first medical contact, the diagnosis of STEACS, arrival at our center, and the door-to-guidewire time. Ischemia time (IT) was defined as the period between symptom onset and passage of the angioplasty guidewire through the culprit lesion. All clinical data were recorded at discharge. The 12-month follow-up data were collected at a medical visit or by telephone contact, using a structured questionnaire.
All patients with a diagnosis of STEACS, whatever the stage of development, and an indication for PPCI according to the criteria of the European Society of Cardiology15 were included in the study. All participants underwent coronary angiography and PPCI following current recommendations.16 Patients gave informed consent for participation, and the study was approved by the local ethics committee for clinical research.
Statistical AnalysisQualitative variables are presented as number and percent, and quantitative variables as the mean±standard deviation (confidence interval) or as the median [interquartile range] for those with a nonnormal distribution. Associations between qualitative variables were evaluated with the chi-square test or with the Fisher exact test when more than 25% of the expected values were < 5. Odds ratios (OR) were estimated with 95% confidence intervals (95%CI). Multiple logistic regression was used to determine which factors studied were associated with a longer DSMA in STEACS patients; the models included variables showing a P value < .15 on univariate analysis. The following variables were entered in the models: age, sex, hypertension, dyslipidemia, smoking, diabetes mellitus, previous infarction, obesity, anatomic location of the infarct, place where medical care was requested, and Killip class at admittance. A crude analysis was carried out of variables related to the management and clinical course of patients showing a longer DSMA. The null hypothesis with a type I error or alpha <.05 was rejected in all the hypothesis tests. Statistical analyses were done with SPSS software, version 15.0. The STROBE guidelines for presenting the results of observational studies were applied to the findings.17
RESULTSDemographic and Clinical CharacteristicsOver the study period, 464 patients with a definite or probable diagnosis of STEACS were referred. Twenty patients in this cohort were excluded, 14 because they did not fulfill the diagnostic criteria of STEACS and 6 because the timeline data were considered unreliable. The main characteristics of the study population are summarized in Table 1. Of the 444 consecutive patients finally included, 338 (76%) were men with a mean age of 63±14 years (23% older than 75 years), 20% had diabetes, 53% had an infarction in an anterior location, and 83% were in Killip class I on admittance to our center. All patients underwent PPCI. Glycoprotein IIb/IIIa platelet inhibitors were used in 37%, mechanical thrombus aspiration in 78%, and stent implantation (54% drug-eluting) in 99% of patients.
Sociodemographic, Clinical and Angiographic Characteristics of the Study Patients at Baseline, During Hospitalization, and at 12 Months
| Variables | Total (n=444) | Time to request medical care | P | |
|---|---|---|---|---|
| > 110 min (n=222) | ≤ 110min (n=222) | |||
| Baseline clinical/ sociodemographic characteristics | ||||
| Women | 106 (24) | 81 (76) | 25 (24) | < .0001 |
| Age, y | 63.0±14.0 | 67.8±15.0 | 58.7±11.6 | < .0001 |
| Age > 75 y | 100 (23) | 89 (20) | 11 (2) | < .0001 |
| Diabetes mellitus | 89 (20) | 56 (63) | 33 (37) | < .001 |
| Hypertension | 240 (54) | 132 (55) | 108 (45) | .02 |
| Dyslipidemia | 205 (46) | 105 (51) | 100 (48) | .60 |
| Smoking | 218 (49) | 93 (43) | 125 (57) | < .01 |
| Previous infarction | 60 (14) | 29 (48) | 31 (52) | .79 |
| BMI > 30 | 89 (20) | 39 (8) | 50 (11) | .28 |
| Anterior location | 237 (53) | 125 (53) | 112 (47) | .17 |
| Place where medical care was requested | ||||
| Hospital | 239 (54) | 101 (42) | 138 (58) | — |
| Home | 111 (25) | 67 (60) | 44 (40) | < .01 |
| Medical center | 87 (20) | 48 (55) | 39 (45) | .46 |
| Others* | 7 (1) | 4 (57) | 3 (43) | .76 |
| Angiographic and clinical characteristics during hospitalization | ||||
| Killip class I | 372 (83) | 179 (82) | 193 (87) | .31 |
| Multivessel disease | 212 (48) | 107 (49) | 105 (47) | .74 |
| Drug-eluting stent | 242 (54) | 109 (55) | 133 (69) | .04 |
| Thrombus aspiration | 244 (55) | 121 (55) | 123 (56) | .11 |
| ST resolution | 288 (65) | 133 (64) | 155 (73) | .04 |
| Q-wave on ECG | 263 (59) | 137 (66) | 126 (55) | .16 |
| Major hemorrhage | 19 (4) | 12 (6) | 7 (3) | .12 |
| Mechanical complication | 30 (7) | 18 (8) | 12 (6) | .24 |
| LVEF < 35% | 38 (9) | 27 (13) | 11 (5) | < .01 |
| In-hospital mortality | 27 (6) | 21 (10) | 6 (3) | < .01 |
| Clinical characteristics at 12 months | ||||
| Reinfarction | 1 (0) | 1 (0) | 0 (0) | .48 |
| Rehospitalization | 32 (7) | 18 (10) | 14 (3) | .33 |
| Heart failure | 12 (3) | 9 (5) | 3 (2) | .06 |
| New revascularization | 15 (3) | 6 (3) | 9 (4) | .52 |
| Any-cause mortality | 20 (5) | 14 (7) | 6 (3) | .05 |
BMI, body mass index; ECG, electrocardiogram; LVEF, left ventricular ejection fraction.
Values are expressed as no (%) or mean±standard deviation.
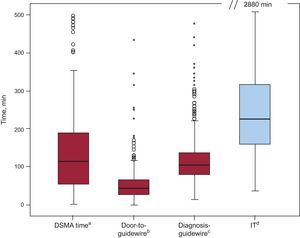
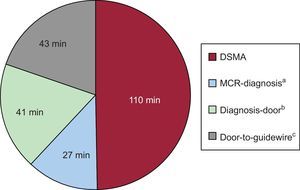
The place where medical care was initially requested was most often the PPCI-capable hospital (54%), followed by telephone requests from the patient's home (25%), and less often from primary care centers or non-PPCI hospitals (21%). Median IT was 225 [160-317] minutes; median DSMA time was 110 [51-190] minutes; median time between the medical care request and first contact with a physician was 39 [15-50] minutes and the door-to-guidewire time was 55 [29-65] minutes. The DSMA time contributed most to the IT (Figure 1). The DSMA was the only value that had a statistically significant influence on the total IT in patients with longer or shorter delay times. There were no significant differences in the time between the first medical contact and guidewire passage (110 vs 98 min; P=.08), door-to-guidewire time (46 vs 40 minutes; P=.22), or patient transfer time (45 vs 40 minutes; P=.17) (Figure 2).
Graph showing various time intervals from ischemia onset to reperfusion. DSMA: delay in seeking medical attention; IT: ischemia time. aTime from symptom onset to request for medical assistance. bTime from arrival at a hospital equipped for primary percutaneous coronary interventions to passage of the angioplasty guidewire through the culprit coronary lesion. cTime from first medical contact to passage of the angioplasty guidewire through the culprit coronary lesion. dIschemia time (from onset of symptoms to passage of angioplasty guidewire).
Contribution of the various time intervals (median) involved in the medical care process to the total ischemia time in the sample. DSMA, delay in seeking medical attention; MCR, medical care request. aTime from the medical care request to establishment of the diagnosis of ST-segment elevation infarction. bTime from the diagnosis of ST-segment elevation infarction to arrival at the hospital for a primary percutaneous coronary intervention. cTime from arrival at the hospital to passage of the angioplasty guidewire through the culprit lesion.
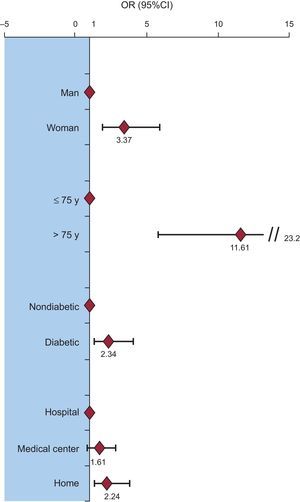
Univariate analysis was carried out on the demographic and clinical characteristics of patients having a longer DSMA time, defined by the median value for this variable (> 110minutes vs ≤ 110 minutes) (Table 2). Patients with a longer DSMA were older (age > 75 years; OR=13.1; 95%CI, 6.7-25.0), more often women (OR=4.6; 95%CI, 2.8-7.6), more often had diabetes (OR=2.0; 95%CI, 1.2-3.2), and requested medical help from their home (OR=2.1; 95%CI, 1.3-3.3) rather than going directly to a medical center or hospital. Following multivariate analysis to correct for potential confounding factors, these 4 variables remained independently associated with longer DSMA. There were no interactions between age, sex, diabetes, or the place where medical care was solicited (Figure 3).
Univariate Analysis of Factors Associated With More Than 110 Minutes’ Delay in Seeking Medical Care
| Variables | Total (n=444) | > 110min, No. (%) | P | OR (95%CI) |
|---|---|---|---|---|
| Sex | < .0001 | 4.6 (2.8-7.6) | ||
| Men | 334 | 138 (41.3) | ||
| Women | 110 | 81 (76.4) | ||
| Age | < .0001 | 13.1 (6.7-25.0) | ||
| > 75 y | 104 | 89 (89.0) | ||
| ≤ 75 y | 340 | 130 (38.2) | ||
| Diabetes mellitus | < .001 | 2.0 (1.2-3.2) | ||
| Yes | 89 | 56 (62.9) | ||
| No | 351 | 163 (46.4) | ||
| Hypertension | .02 | 1.5 (1.0-2.3) | ||
| Yes | 242 | 132 (55.0) | ||
| No | 202 | 87 (43.5) | ||
| Dyslipidemia | .60 | 1.1 (0.7-1.6) | ||
| Yes | 205 | 105 (51.2) | ||
| No | 232 | 113 (48.7) | ||
| Smoking | < .01 | 0.6 (0.4-0.8) | ||
| Yes | 218 | 93 (42.7) | ||
| No | 213 | 119 (55.9) | ||
| Previous infarction | .79 | 0.9 (0.5-1.6) | ||
| Yes | 60 | 29 (48.3) | ||
| No | 377 | 189 (50.1) | ||
| Obesity | .28 | 0.8 (0.5-1.2) | ||
| Yes | 89 | 39 (43.8) | ||
| No | 290 | 146 (50.3) | ||
| Infarct location | .17 | 1.3 (0.9-1.9) | ||
| Anterior | 237 | 125 (52.7) | ||
| Others | 203 | 94 (46.3) | ||
| Place where medical care was requested | ||||
| Hospital | 239 | 101 (42.3) | — | — |
| Home | 111 | 67 (60.4) | < .01 | 2.1 (1.3-3.3) |
| Medical center | 87 | 48 (55.2) | .46 | 1.2 (0.7-2.2) |
95%CI, 95% confidence interval; OR, odds ratio.
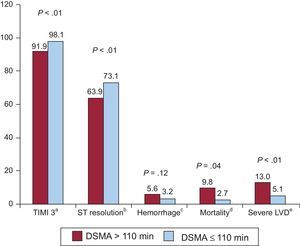
At the initial evaluation, TIMI 3 (Thrombolysis In Myocardial Infarction grade 3) flow was more frequent in patients more promptly seeking medical attention than in those with a longer delay (47% vs 39%; P<.005). Following PPCI, TIMI 3 flow was reached in fewer patients taking longer to request medical care (>110minutes) than in those promptly seeking care (92% vs 98%; P<.005) and ST segment resolution was also less frequent in the group with a longer delay (64% vs 73%; P<.005). Furthermore, drug-eluting stents were used less often in patients with a longer delay time (55% vs 69%; P=.04).
There were no differences between the groups regarding the percentage receiving dual antiplatelet therapy before PPCI. However, glycoprotein IIb/IIIa platelet inhibitor use was lower (53% vs 72%; P<.001) and bivalirudin use was higher (27% vs 8%; P<.001) in patients showing a longer delay.
No differences between the groups were found for the development of heart failure or major bleeding complications during hospital admittance. Nonetheless, in the group with a longer delay, a higher percentage had a poor left ventricular ejection fraction (LVEF) (< 35%) (13% vs 5%; P<.005) and significantly higher in-hospital mortality due to any cause than those seeking help sooner (9.8% vs 2.7%; P<.005) (Figure 4). Lastly, at 12 months’ follow-up, any-cause mortality was also significantly higher in the group with a longer DSMA (7.3% vs 2.9%; P<.05).
Differences in prognostic markers and clinical events during hospitalization between patients with a longer and shorter delay. in seeking medical attention. DSMA, delay in seeking medical attention; LVD, left ventricular dysfunction; TIMI 3, Thrombolysis In Myocardial Infarction grade 3. aAchievement of TIMI 3 flow following primary angioplasty. bAt 90 min following angioplasty, ST segment decrease of at least 50% in leads previously showing an increase. cBleeding requiring transfusion or surgery, or hemoglobin decrease ≥ 3 g/dL. dAny-cause mortality during hospital admittance. eLeft ventricular ejection fraction < 35%.
Mortality in STEACS is clearly related to the time that passes from the development of the acute coronary occlusion to the moment reperfusion is achieved.5 In many studies, the prehospital time has been found to contribute most to the reperfusion time.18 However, there is little information on the time interval from symptom onset to the moment when medical care is requested, the impact of this delay on total IT, and the factors contributing to the delay. Most available data on this issue are from studies performing a general analysis of “prehospital delay”,12–14,18,19 usually defined as the interval from symptom onset to hospital arrival. According to the regional organization of health care for these patients, prehospital delay would only be equivalent to the DSMA if patients were to go directly to a hospital with PPCI capability. In contrast, in organizational systems that include initial medical attention in the patient's home or primary care centers, as in Spain, the delay would have 2 components: the DSMA (dependent on the patient) and the time of initial medical attention, diagnosis, and medicalized transport to a PPCI hospital (mainly dependent on the system). This is the first study specifically and prospectively investigating DSMA and its implications. The results show that this time period, which depends exclusively on the patient, accounts for around two-thirds of the total prehospital delay and half (48%) the IT.
In the patient series studied, elderly individuals were those most clearly affected by this delay (OR=11). This factor may have contributed to the lower efficacy of mechanical reperfusion therapy reported in this patient population in previous studies.20 Our findings concur with data from studies conducted in other countries, and highlight the need for specific interventions designed for this demographic group.20–22 In a study including both STEACS patients and non—ST-segment elevation acute coronary syndrome patients, Saczynski et al12 found that the problem of delays in receiving medical attention was especially important in patients older than 75 years.
In the present study, female sex and diabetes mellitus emerged as robust independent predictors of DSMA following the onset of compatible symptoms. These findings are also consistent with those of previous studies. In a substudy of the MONICA registry, prehospital delay was specifically investigated in patients with diabetes in a cohort of more than 4000 patients with acute coronary syndrome.22 Diabetic patients showed a longer prehospital delay, with no differences between sexes.22 It is well-recognized that women and individuals with diabetes who experience STEACS have a poorer clinical course. The delay to reperfusion may play an essential role in the outcome of these subgroups, although this has not been definitely established. There is some indication that these patient subgroups may present with atypical symptoms more often, making it more difficult to recognize the severity of the condition, but the evidence supporting this notion is scant.23,24
The present study did not reveal an association between the DSMA and factors linked to reperfusion delay in other studies, such as hypertension or a previous history of myocardial infarction. Additional population studies are needed to better define elements that determine a delay in recognizing the symptoms or perceiving the severity of the disease, and to identify other factors that may lead to a delay receiving medical attention, with the consequent lengthening of the total IT.
Patients showing a longer delay before requesting medical care had higher mortality in the acute phase of the condition and at 1-year of follow-up, likely because the IT had been longer and they had epidemiologic characteristics associated with a poorer prognosis. These findings concur with those of previous studies, although it remains to be determined whether the delay time, the epidemiologic characteristics of this group (elderly individuals, women, and diabetic individuals), or a combination of both elements are responsible for the poorer prognosis.
LimitationsOne of the main limitations of this study is the relatively small sample size, which, however, sufficed to achieve the power needed to detect significant associations. In addition, the study had a clinical focus, and other relevant factors, such as the patients’ economic level and the fact of living alone or with others were not investigated. Nor did we analyze the influence of the time point of presentation or whether it was a workday or weekend, which are possible confounding variables. Finally, the potential bias inherent to observational studies should also be taken into account.
CONCLUSIONSAmong STEACS patients, those older than 75 years, women, and individuals with diabetes are more likely to experience a longer DSMA. Furthermore, patients who request medical assistance from their home show longer DSMA than those who go directly to a medical center. From the clinical standpoint, the group with a longer DSMA were found to have a more prolonged IT and higher in-hospital and 1-year mortality than patients with shorter delay times. Further studies are needed to determine whether specific programs targeting STEACS patients with a higher risk of prolonged DSMA can help to improve the prognosis of this patient population.
CONFLICTS OF INTERESTNone declared.