ST-segment elevation myocardial infarction (STEMI) network activation by a noncardiologist reduces delay times but may increase the rate of false-positive STEMI diagnoses. We aimed to determine the prevalence, predictors, and clinical impact of false-positive activations within the Catalonian STEMI network (Codi Infart).
MethodsFrom January 2010 through December 2011, all consecutive patients treated within the Codi Infart network were included. Code activations were classified as appropriate if they satisfied both electrocardiogram and clinical STEMI criteria. Appropriate activations were classified as false positives using 2 nonexclusive definitions: a) “angiographic” if a culprit coronary artery was not identified, and b) “clinical” if the discharge diagnosis was other than STEMI.
ResultsIn total, 5701 activations were included. Appropriate activation was performed in 87.8% of the episodes. The rate of angiographic false positives was 14.6%, while the rate of clinical false positives was 11.6%. Irrespective of the definition, female sex, left bundle branch block, and previous myocardial infarction were independent predictors of false-positive STEMI diagnoses. Using the clinical definition, hospitals without percutaneous coronary intervention and patients with complications during the first medical contact also had a false-positive STEMI diagnoses rate higher than the mean. In-hospital and 30-day mortality rates were similar for false-positive and true-positive STEMI patients after adjustment for possible confounders.
ConclusionsFalse-positive STEMI diagnoses were frequent. Outcomes were similar for patients with a true-positive or false-positive STEMI diagnosis treated within a STEMI network. The presence of any modifiable predictors of a false-positive STEMI diagnosis warrants careful assessment to optimize the use of STEMI networks.
Keywords
Percutaneous coronary intervention (PCI) is the treatment of choice in patients with ST-segment elevation myocardial infarction (STEMI), when performed expeditiously by properly trained personnel.1,2 A reduction of total ischemia time improves clinical outcomes in STEMI patients,3,4 and the decision on reperfusion therapy should be made promptly after the first medical contact (FMC). A key strategy to reduce FMC-to-balloon times is to allow attending health care professionals to make a diagnosis, select reperfusion strategies, and transfer patients to cardiac catheterization laboratories or administer thrombolytic treatment based on clinical and electrocardiogram (ECG) information.5–7
Reperfusion strategy selection by noncardiologists could decrease total ischemia times but could potentially increase inappropriate STEMI network activation and/or false-positive STEMI diagnoses. In addition, depending on the patient's clinical status, cardiac catheterization in patients without STEMI might be associated with deleterious consequences related to the procedure and should therefore be avoided. Identification of predictors associated with false-positive STEMI diagnoses should help health care professionals to improve diagnostic accuracy.
The objective of this study was to determine the prevalence of inappropriate STEMI network activations and false-positive STEMI diagnoses and their influence on clinical outcomes.
METHODSThis was an observational, multicenter study based on prospectively collected data from consecutive patients treated within the Catalonian STEMI network (Codi Infart) from January 2010 through December 2011.
Catalonia is an Autonomous Community in northeast Spain with a population of approximately 7 500 000 inhabitants. In June 2009, a regional STEMI network was introduced in Catalonia.8,9 To provide the most appropriate reperfusion therapy in each patient, the network was divided into referral areas for PCI-equipped hospitals. The Codi Infart network has 4 components: a) emergency medical services (EMS) ambulances staffed by physicians or nurses able to diagnose symptoms, interpret an ECG, select a reperfusion strategy, and administer fibrinolytic therapy; b) an EMS dispatch center that coordinates the logistics between the ambulances or community hospitals and the primary PCI hospitals; c) 10 primary PCI hospitals, 5 of which have 24/7 availability (at the time of the study period); d) a Codi Infart registry, with prospective inclusion of all patients treated within the network; demographic, clinical, and procedural data, delay times, and in-hospital complications are recorded. All-cause mortality was evaluated with a telephone call 30 days after the episode. Complications during the FMC were defined as cardiac arrest, ventricular tachycardia, atrioventricular block, cardiogenic shock, mechanical ventilation, and major bleeding.
The Codi Infart network is activated after a health care professional has diagnosed a patient with STEMI based on ECG and clinical criteria. Once the network is activated, the reperfusion strategy is selected according to standard guidelines. If primary PCI is selected, the patient is transferred to the nearest primary PCI center; after primary PCI and when clinically stable, the patient is transported to the referral center to avoid oversaturation of PCI centers. All patients treated with fibrinolysis are transferred to a PCI center immediately if fibrinolysis fails or for elective coronary angiography. Secondary prevention treatment is prescribed according to standard medical practice.
ST-segment elevation myocardial infarction code activation criteria were defined according to the universal definition of myocardial infarction10: a) ECG criteria with new ST-segment elevation or new or presumably new left bundle branch block (LBBB), and b) clinical criteria suggestive of possible ischemic symptoms such as various combinations of chest, upper extremity, mandibular or epigastric discomfort, or an ischemic equivalent including dyspnea or fatigue. The cardiologists who were in charge of the patient after his or her arrival at the primary PCI center (referral center) were responsible for determining if the STEMI code activation criteria were satisfied and that the decision was recorded in the Codi Infart registry database.
Inappropriate STEMI code activation was defined as any activation of the network in patients who lacked 1 or both of the STEMI activation criteria previously described.
Several “false-positive” STEMI diagnoses definitions have been proposed.11–14 For the purpose of this study, we considered 2 definitions: a) angiographic, which included patients without a culprit coronary artery (acute total or subtotal occlusion of a coronary artery or a coronary lesion with a visible thrombus), and b) clinical, which included patients with a discharge diagnosis other than STEMI, including unstable angina, non-STEMI, and nonacute coronary syndrome, irrespective of the treatment.
The study cohort was divided into 2 groups according to the appropriateness of the activation (group 1: inappropriate activation; group 2: appropriate activation). Group 2 was classified according to the 2 nonexclusive, prespecified, false-positive STEMI diagnoses definitions. For the purpose of this study, when the FMC was in a PCI center without 24/7 PCI capability in an hour without PCI availability, the place of the FMC was registered as the PCI center.
Statistical AnalysisContinuous variables were explored for normal distribution with the Kolmogorov-Smirnov test. Normally distributed variables are expressed as mean ± standard deviation and nonnormally distributed variables are expressed as median [interquartile range] and were compared using the Student t or Mann-Whitney U tests, as appropriate. Categorical variables are expressed as count (percentage) and were compared using the chi-square test. Logistic regression analysis was performed using a likelihood ratio-based backward exclusion method to evaluate the effect of explanatory variables on the presence of inappropriate activation or false-positive STEMI diagnosis. The variables included in the final adjusted regression model were selected on the basis of a combination of statistical significance (P<.10) and clinical judgement. The results are reported as odds ratios (OR), together with their 95% confidence intervals (95%CI). To evaluate the association between the type of activation and in-hospital and 30-day all-cause mortality, proportional hazard Cox regression analyses were developed. An exploratory univariate analysis was performed and covariates with a clinical justification or P value<.10 were entered in the Cox models. The result is reported as hazard ratio (HR), together with the 95%CI. All P values were 2-tailed, with statistical significance set at a level of P<.05. Statistical analyses were performed using SPSS Statistics 20.0 (SPSS Inc., Chicago, Illinois, United States).
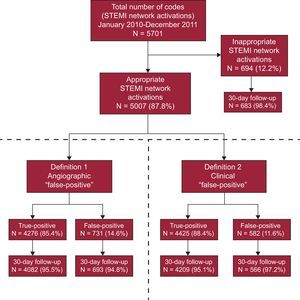
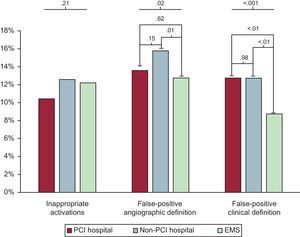
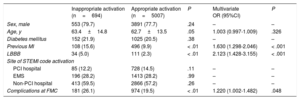
RESULTSAppropriate Versus Inappropriate ActivationsDuring the 2-year study period, 5701 STEMI codes were activated in the Codi Infart network. Of these, 5007 (87.8%) satisfied clinical and ECG criteria for an appropriate activation; 694 (12.2%) were adjudicated as inappropriate activations (Figure 1). The main characteristics according to the appropriateness of the activation are shown in Table 1. In 216 (31.1%) of the inappropriate activations, the absence of LBBB or ST-segment elevation did not satisfy ECG criteria. The remaining 478 (68.9%) episodes showed a discrepancy in the clinical criteria for STEMI according to the cardiologist at the PCI hospital. There were no statistically significant differences in these results between the STEMI network activation points (Figure 2). Patients with an inappropriate activation were older and had a higher prevalence of previous myocardial infarction (Table 1). Left bundle branch block was more frequent in patients with inappropriate activation than in those who satisfied clinical and ECG criteria (5.0% vs 2.3%; P<.01). Percutaneous coronary intervention was performed in 240 patients (34.6%) in the inappropriate activation group. Unstable angina and non-STEMI were the discharge diagnoses in 51 patients (7.3%) and in 55 (7.9%) patients, respectively. On multivariate analysis, previous myocardial infarction, LBBB, and complications during FMC were independently associated with a higher risk of inappropriate activation (Table 1). In-hospital mortality was similar between inappropriate and appropriate activations (3.9% vs 2.8%; P=.12). After 30 days of follow-up, mortality was also similar between groups (7.8% vs 6.1%; P=.10).
Univariate and Multivariate Predictors of Inappropriate STEMI Network Activations
| Inappropriate activation (n=694) | Appropriate activation (n=5007) | P | Multivariate OR (95%CI) | P | |
|---|---|---|---|---|---|
| Sex, male | 553 (79.7) | 3891 (77.7) | .24 | – | – |
| Age, y | 63.4±14.8 | 62.7±13.5 | .05 | 1.003 (0.997-1.009) | .326 |
| Diabetes mellitus | 152 (21.9) | 1025 (20.5) | .38 | – | – |
| Previous MI | 108 (15.6) | 496 (9.9) | < .01 | 1.630 (1.298-2.046) | < .001 |
| LBBB | 34 (5.0) | 111 (2.3) | < .01 | 2.123 (1.428-3.155) | < .001 |
| Site of STEMI code activation | |||||
| PCI hospital | 85 (12.2) | 728 (14.5) | .11 | – | – |
| EMS | 196 (28.2) | 1413 (28.2) | .99 | – | – |
| Non-PCI hospital | 413 (59.5) | 2866 (57.2) | .26 | – | – |
| Complications at FMC | 181 (26.1) | 974 (19.5) | < .01 | 1.220 (1.002-1.482) | .048 |
95%CI, 95% confidence interval; EMS, emergency medical service; FMC, first medical contact; LBBB, left bundle branch block; MI, myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed mean±standard deviation or No. (%).
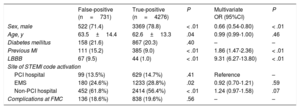
Of a total of 5007 appropriate STEMI code activations, 731 (14.6%) were classified as false-positive STEMI diagnoses according to the angiographic definition (Figure 1). When the FMC occurred in a non-PCI hospital, the false-positive rate was higher than the mean; in contrast, there was a higher rate of true-positive STEMI diagnoses when the FMC was the EMS. The false-positive rate was higher in non-PCI hospitals compared with PCI hospitals and EMS (Figure 2). ST-segment elevation myocardial infarction diagnoses classified as “false-positive” with the angiographic definition were more frequent in older patients, in women, and in patients with a higher prevalence of previous myocardial infarction (Table 2). In addition, the proportion of patients with LBBB was higher in the angiographic false-positive group than in the true-positive group. In the multivariate analysis, female sex, previous myocardial infarction, and LBBB were independently associated with a higher risk of false-positive diagnoses. Univariate and multivariate predictors of angiographic false-positive diagnoses are shown in Table 2. By definition, none of the patients in the angiographic false-positive group were treated with PCI; however, a higher proportion of patients in this group were treated with fibrinolysis compared with the true-positive group (9.2% vs 6.7%; P=.02). False-positive patients had a lower prevalence of atrioventricular block at FMC and during hospitalization (2.5% vs 4.4%; P=.01 and 1.1% vs 3.9%; P<.01), and a lower prevalence of ventricular fibrillation or ventricular tachycardia during hospitalization (2.5% vs 5.3%; P=.02). The prevalence of cardiogenic shock during FMC was numerically higher in the false-positive group, although the difference was nonsignificant (5.7% vs 4.4%; P=.10). The final diagnosis was unstable angina in 16.3% of patients classified as false-positive STEMI with the clinical definition and was non-STEMI in 0.52%; the remaining patients were classified as having nonacute coronary syndromes. As for the patients who were classified as false-positive STEMI with the angiographic definition, 9.3% had a diagnosis of unstable angina, and 9.4% had a diagnosis of non-STEMI, while the remaining patients had diagnoses other than acute coronary syndrome. Crude in-hospital and 30-day mortality was higher in patients with an angiographic false-positive diagnosis than in patients with a true-positive diagnosis (4.5% vs 2.6%; P=.01 and 7.8% vs 5.8%; P=.05 respectively) (Figure 3A). However, after adjustment for possible confounders, the risk of in-hospital and 30-day mortality was similar between groups (HR, 0.94; 95%CI, 0.61-1.47, and HR, 1.04; 95%CI, 0.76-1.42, respectively).
Univariate and Multivariate Predictors of False-positive STEMI Network Activations (Angiographic Definition)
| False-positive (n=731) | True-positive (n=4276) | P | Multivariate OR (95%CI) | P | |
|---|---|---|---|---|---|
| Sex, male | 522 (71.4) | 3369 (78.8) | < .01 | 0.66 (0.54-0.80) | < .01 |
| Age, y | 63.5±14.4 | 62.6±13.3 | .04 | 0.99 (0.99-1.00) | .46 |
| Diabetes mellitus | 158 (21.6) | 867 (20.3) | .40 | – | – |
| Previous MI | 111 (15.2) | 385 (9.0) | < .01 | 1.86 (1.47-2.36) | < .01 |
| LBBB | 67 (9.5) | 44 (1.0) | < .01 | 9.31 (6.27-13.80) | < .01 |
| Site of STEMI code activation | |||||
| PCI hospital | 99 (13.5%) | 629 (14.7%) | .41 | Reference | – |
| EMS | 180 (24.6%) | 1233 (28.8%) | .02 | 0.92 (0.70-1.21) | .59 |
| Non-PCI hospital | 452 (61.8%) | 2414 (56.4%) | < .01 | 1.24 (0.97-1.58) | .07 |
| Complications at FMC | 136 (18.6%) | 838 (19.6%) | .56 | – | – |
95%CI, 95% confidence interval; EMS, emergency medical service; FMC, first medical contact; LBBB, left bundle branch block; MI, myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed mean±standard deviation or No. (%).
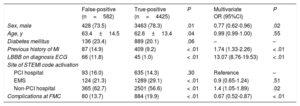
Of a total of 5007 appropriate STEMI code activations, 582 (11.6%) were classified as clinical false positives (Figure 1). Similar to the angiographic definition, when patients initially arrived at a non-PCI hospital, the prevalence of false positives was higher than the mean, but when the FMC was the EMS, significantly fewer episodes were classified as false positives (Figure 2). The proportion of patients with LBBB was higher in the clinical false-positive group than in the true-positive group. False-positive STEMI diagnoses based on the discharge diagnosis definition occurred in patients who were more frequently older, women, and had a higher prevalence of previous myocardial infarction (Table 3). In the multivariate analysis, female sex, previous myocardial infarction, LBBB, and complications during FMC were independently associated with a higher risk of false-positive diagnoses according to the clinical definition. In addition, STEMI network activation by the EMS was independently associated with a lower risk of false-positive diagnoses compared with network activation within a non-PCI community hospital. Univariate and multivariate predictors of clinical false-positive diagnoses are shown in Table 3. Patients classified as false-positive with the clinical definition were less likely to be treated with fibrinolysis, primary PCI, or rescue PCI; nonetheless, 132 (22.6%) patients in the false-positive group were treated with either primary or rescue PCI. “False-positive” patients had a lower prevalence of atrioventricular block at FMC and during hospitalization (2.6% vs 4.3%; P=.04, and 0.5% vs 3.9%; P<.01, respectively) and a lower prevalence of ventricular fibrillation or ventricular tachycardia during FMC and hospitalization (5.2% vs 7.5%; P=.03, and 1.7% vs 5.3%; P<.01, respectively). The prevalence of cardiogenic shock was similar between groups during FMC and hospitalization (4.8% vs 4.5%; P<.77, and 5.0% vs 6.1%; P=.27, respectively). Crude in-hospital and 30-day mortality was similar between patients with false-positive activation based on discharge diagnosis than in patients with true-positive activation (3.3% vs 2.8%; P=.51 and 7.1% vs 6.0%; P=.31, respectively) (Figure 3B).
Univariate and Multivariate Predictors of False-positive STEMI Network Activations (Clinical Definition)
| False-positive (n=582) | True-positive (n=4425) | P | Multivariate OR (95%CI) | P | |
|---|---|---|---|---|---|
| Sex, male | 428 (73.5) | 3463 (78.3) | .01 | 0.77 (0.62-0.96) | .02 |
| Age, y | 63.4±14.5 | 62.6±13.4 | .04 | 0.99 (0.99-1.00) | .55 |
| Diabetes mellitus | 136 (23.4) | 889 (20.1) | .06 | – | – |
| Previous history of MI | 87 (14.9) | 409 (9.2) | < .01 | 1.74 (1.33-2.26) | < .01 |
| LBBB on diagnosis ECG | 66 (11.8) | 45 (1.0) | < .01 | 13.07 (8.76-19.53) | < .01 |
| Site of STEMI code activation | |||||
| PCI hospital | 93 (16.0) | 635 (14.3) | .30 | Reference | – |
| EMS | 124 (21.3) | 1289 (29.1) | < .01 | 0.9 (0.65-1.24) | .51 |
| Non-PCI hospital | 365 (62.7) | 2501 (56.6) | < .01 | 1.4 (1.05-1.89) | .02 |
| Complications at FMC | 80 (13.7) | 884 (19.9) | < .01 | 0.67 (0.52-0.87) | < .01 |
95%CI, 95% confidence interval; ECG, electrocardiogram; EMS, emergency medical service; FMC, first medical contact; LBBB, left bundle branch block; MI, myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed mean ± standard deviation or No. (%).
Our study describes the demographic characteristics and clinical outcomes of false-positive STEMI diagnoses of a regional network in a large cohort of patients. The main findings can be summarized as follows: a) a high prevalence of false-positive STEMI diagnosis was observed; b) female sex, a previous history of myocardial infarction, and LBBB were independent predictors of “false-positive” diagnoses, irrespective of whether the clinical or angiographic definition was applied; c) the presence of clinical complications during FMC was also independently associated with a higher rate of false-positive diagnoses; d) EMS network activations were associated with a lower rate of “false positives” when the clinical definition was used; and e) no differences in 30-day mortality were observed between the false-positive and true-positive groups.
False-positive STEMI diagnoses were identified in 14.6% and 11.6% of appropriate STEMI activations when the nonexclusive angiographic and clinical definitions were used, respectively. The rate of false-positive diagnosis is similar to those reported in other series, which range from 14% to 36%.12,14
Female sex, a prior history of myocardial infarction, and LBBB on diagnostic ECG were independent predictors of false-positive activation. Female sex has been previously described as an independent predictor of delay in seeking medical attention and of false-positive STEMI network activation. Women are known to have different symptoms to men during a myocardial infarction.15 The difference in clinical presentation could explain the higher rate of false positives with the clinical definitions. Women also have a higher rate of acute myocardial infarction with no obstructive coronary atherosclerosis, which might also explain the higher rate of false positives with the angiographic definition. In the multivariate analysis, the presence of a LBBB pattern was associated with the highest risk of a false-positive diagnosis. Even with the use of the specific ECG criteria for the diagnosis of acute myocardial infarction in the presence of LBBB,16 LBBB has been consistently associated with a higher rate of false-positive diagnoses. Despite a higher rate of false-positive diagnoses in patients with LBBB and symptoms suggestive of myocardial infarction, patients with LBBB and a true acute myocardial infarction have poor clinical outcomes,17 and caution should be exercised before ruling out acute myocardial infarction and reperfusion therapies in those patients.18,19
In our study, 694 (12.2%) activations were classified as inappropriate when current guidelines were used.1 This percentage is similar to that in other registries, which ranged from 5% to 31%.20 Caution is advised when comparing the percentage of inappropriate activations, because of the different definitions used, and the improper interchange of the terms “inappropriate” and “false-positive”. Garvey et al.20 examined the percentage and outcome of inappropriate STEMI activation in a US statewide network with 14 primary PCI regional centers. To be categorized as inappropriate, activations had to have been cancelled because of ECG reinterpretation or because the patient was not a candidate for cardiac catheterization according to the Reperfusion of Acute Myocardial Infarction in the North Carolina Emergency Departments (RACE) initiative. Among the 5073 alerts, 3973 patients were included in the analysis, which found a 15% rate of inappropriate activations. In contrast to their study, our group found no differences in the percentage of inappropriate activations according to the point of activation. The similar rate of inappropriate activations by the EMS in comparison with non-PCI or primary PCI hospitals in Catalonia could be explained by the staffing of advanced life support EMS ambulances with nurses and/or physicians who might be more experienced in the diagnosis of STEMI patients than community hospital staff. Out-of-hospital STEMI activation by nonphysicians has been associated with higher rates of inappropriate activation,21 although the safety and effectiveness of out-of-hospital STEMI network activation by nonphysicians has been extensively studied and validated.17,22–26
Higher mortality was observed in the angiographic false-positive group than in the true-positive STEMI group; however, after adjustment for possible confounders, this difference was no longer significant. Our findings are similar to those observed in previous studies,14 highlighting the similar mortality rates in patients regardless of their classification as having false-positive or true-positive STEMI. Once the STEMI network is activated, access to a tertiary hospital with specialized acute and intensive cardiology care is straightforward in our network. To avoid unnecessary delays, the STEMI network protocol obviates the need for a cardiologist to diagnose STEMI. In this scenario, patients with critical conditions that do not fulfill both criteria (clinical and ECG) could be transferred to a center with specialized cardiology care, including high-risk patients who could benefit from early diagnosis, thus explaining the higher mortality observed in the inappropriate activation and false-positive STEMI diagnosis groups.
LimitationsThe present study has several limitations that should be highlighted. Our findings are the result of a retrospective analysis. Discharge diagnosis was classified as STEMI or other, and the alternative diagnosis was not obtained. Information on 30-day mortality was not obtained in all patients, although missing data accounted for less than 5% in both groups. Another limitation is the timespan between the last date of follow-up and reporting of the results. However, the results of the present study seem to be valid as the characteristics of the study population are similar to those of contemporaneous STEMI registries.27 Furthermore, although the 24/7 capability of the Codi Infart network hospitals has increased from 5 to 10 hospitals since the beginning of the study period, the main components of the network and its organization remain unchanged. Another limitation of our study is the relatively short follow-up. Our conclusions should be taken as hypothesis-generating and need to be confirmed in future studies with longer follow-up.
CONCLUSIONSFalse-positive STEMI diagnoses within a regional network were frequent. Patients who did not fulfill STEMI criteria and were still treated within a STEMI network had similar short-term mortality to patients with true STEMI. The presence of any modifiable predictors of a false-positive STEMI diagnosis warrants careful assessment to optimize the use of STEMI networks.
FUNDINGAssistance was provided for conducting the statistical analysis of the study, funded by the Codi Infart program of the Pla director de malalties de l’aparell circulatori.
CONFLICTS OF INTERESTNone declared.
- –
Reduction of total ischemia time improves clinical outcomes in patients with STEMI.
- –
Reduction of FMC-to-balloon times in patients with STEMI can be achieved by allowing attending health care professionals to make a diagnosis, select reperfusion strategies, and transfer patients to cardiac catheterization laboratories.
- –
Short-term outcomes are similar between patients with true-positive or false-positive ST-segment elevation diagnoses treated within a STEMI network.
- –
Irrespective of the definition of false-positive STEMI, the factors associated with a higher risk of false-positive STEMI diagnosis were female sex, a previous history of myocardial infarction, and LBBB.
- –
The presence of clinical complications during FMC is associated with a higher rate of false-positive STEMI diagnosis using a clinical definition.
The authors would like to thank all the professionals involved in the Codi Infart program. We recognize Ignacio Ferreira-González and Josep Ramón Marsal for their invaluable assistance in the statistical analysis.