The introduction of the latest generation of bioprosthetic aortic valves has allowed specialist centers experienced in transcatheter aortic valve implantation (TAVI) to use minimally invasive approaches, which reduce hospitalization times. Early hospital discharge after TAVI with balloon-expandable valve prostheses has been shown to be safe,1–3 but there is less evidence for TAVI with self-expanding valves,4,5 raising concerns about the risk of conduction disorders. In this context, immediate assessment of the conduction system through rapid atrial pacing (RAP) is useful to evaluate the integrity of the conduction system and predict the need for pacemaker implantation during follow-up.6
In the present study, we retrospectively analyzed the outcomes of a protocol for early post-TAVI discharge (APRETAVI) introduced in response to the COVID-19 pandemic. This patient-care protocol included all elective TAVI procedures conducted with ultrasound-guided transfemoral access and conscious sedation. We excluded hospitalized patients, those undergoing by more invasive procedures, and severely frail patients lacking adequate family support. The Medical Research Ethics Committee granted an exemption for informed patient consent.
After elective admission, patients received appropriate preparation for the intervention (including assessment of their familial and social situation and frailty status) and gave informed consent. After the TAVI procedure, the conduction system was assessed by RAP.6 Pacing was discontinued in the catheterization laboratory in patients in sinus rhythm who did not develop Wenckebach atrioventricular (AV) block at RAP rates up to 120 bpm, as well as in those in atrial fibrillation with a post-TAVI His-ventricular interval <55ms. Otherwise, pacing was continued for at least 24hours. Patients were monitored for a minimum of 12hours after the TAVI procedure and underwent physical examination, electrocardiography, complete blood count, and transthoracic echocardiography.
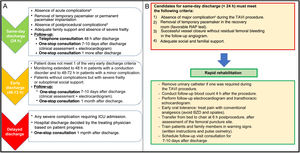
Patients without complications were considered for very early discharge (< 24hours) according to the scheme depicted in figure 1A. Those meeting all the early discharge criteria were given a “rapid rehabilitation” guide (figure 1B) and a pulse heart rate monitor together with written instructions detailing abnormal readings requiring prompt consultation with the medical team after discharge. Each patient's status was also monitored via telephone within 48hours of discharge. As per the protocol, all patients discharged early (< 72hours) attended a clinical follow-up consultation 1 week after TAVI, including assessment of the femoral puncture site and a follow-up electrocardiogram). A further in-depth consultation took place after 1 month.
A: Early hospital discharge algorithm. B: Rapid rehabilitation protocol. AV, atrioventricular; BZD, benzodiazepines.
aSevere respiratory insufficiency, hemodynamic instability, cardiac tamponade, significant aortic regurgitation, severe vascular complication, stroke, severe arrhythmias.
bSignificant anemia, nonoliguric acute renal failure, delirium, pericardial effusion, prosthesis malfunction, advanced atrioventricular conduction disorders.
cMajor complications: hemodynamic or electric instability, severe vascular complication, stroke, coronary occlusion, pericardial effusion, aortic rupture, severe aortic regurgitation.
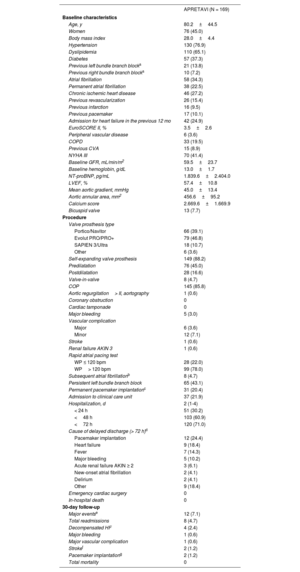
A total of 169 patients underwent transfemoral TAVI at our center between June 2020 and January 2022. The mean age of the patients was 80.2±44.5 years, and 45% of the patients were women. The mean EuroSCORE II was 3.5±2.6%. Baseline patient characteristics are summarized in table 1. Transfemoral access with local anesthesia was achieved in all patients, and secondary radial access was achieved in 164 patients (97%). The incidence of severe complications (VARC-2) was low (table 1). The pacing protocol permitted immediate removal of the temporary pacemaker in 62.9% of the patients. The median length of hospital stay was 2 [interquartile range, 1-4] days, and very early discharge (<24hours) was achieved in 30.2% of the patients. The main causes of delayed discharge are listed in table 1.
Patient characteristics at baseline, procedure details, and 30-day follow-up outcomes
| APRETAVI (N = 169) | |
|---|---|
| Baseline characteristics | |
| Age, y | 80.2±44.5 |
| Women | 76 (45.0) |
| Body mass index | 28.0±4.4 |
| Hypertension | 130 (76.9) |
| Dyslipidemia | 110 (65.1) |
| Diabetes | 57 (37.3) |
| Previous left bundle branch blocka | 21 (13.8) |
| Previous right bundle branch blocka | 10 (7.2) |
| Atrial fibrillation | 58 (34.3) |
| Permanent atrial fibrillation | 38 (22.5) |
| Chronic ischemic heart disease | 46 (27.2) |
| Previous revascularization | 26 (15.4) |
| Previous infarction | 16 (9.5) |
| Previous pacemaker | 17 (10.1) |
| Admission for heart failure in the previous 12 mo | 42 (24.9) |
| EuroSCORE II, % | 3.5±2.6 |
| Peripheral vascular disease | 6 (3.6) |
| COPD | 33 (19.5) |
| Previous CVA | 15 (8.9) |
| NYHA III | 70 (41.4) |
| Baseline GFR, mL/min/m2 | 59.5±23.7 |
| Baseline hemoglobin, g/dL | 13.0±1.7 |
| NT-proBNP, pg/mL | 1.839.6±2.404.0 |
| LVEF, % | 57.4±10.8 |
| Mean aortic gradient, mmHg | 45.0±13.4 |
| Aortic annular area, mm2 | 456.6±95.2 |
| Calcium score | 2.669.6±1.669.9 |
| Bicuspid valve | 13 (7.7) |
| Procedure | |
| Valve prosthesis type | |
| Portico/Navitor | 66 (39.1) |
| Evolut PRO/PRO+ | 79 (46.8) |
| SAPIEN 3/Ultra | 18 (10.7) |
| Other | 6 (3.6) |
| Self-expanding valve prosthesis | 149 (88.2) |
| Predilatation | 76 (45.0) |
| Postdilatation | 28 (16.6) |
| Valve-in-valve | 8 (4.7) |
| COP | 145 (85.8) |
| Aortic regurgitation> II, aortography | 1 (0.6) |
| Coronary obstruction | 0 |
| Cardiac tamponade | 0 |
| Major bleeding | 5 (3.0) |
| Vascular complication | |
| Major | 6 (3.6) |
| Minor | 12 (7.1) |
| Stroke | 1 (0.6) |
| Renal failure AKIN 3 | 1 (0.6) |
| Rapid atrial pacing test | |
| WP ≤ 120 bpm | 28 (22.0) |
| WP> 120 bpm | 99 (78.0) |
| Subsequent atrial fibrillationb | 8 (4.7) |
| Persistent left bundle branch block | 65 (43.1) |
| Permanent pacemaker implantationc | 31 (20.4) |
| Admission to clinical care unit | 37 (21.9) |
| Hospitalization, d | 2 (1-4) |
| < 24 h | 51 (30.2) |
| <48 h | 103 (60.9) |
| <72 h | 120 (71.0) |
| Cause of delayed discharge (> 72 h)d | |
| Pacemaker implantation | 12 (24.4) |
| Heart failure | 9 (18.4) |
| Fever | 7 (14.3) |
| Major bleeding | 5 (10.2) |
| Acute renal failure AKIN ≥ 2 | 3 (6.1) |
| New-onset atrial fibrillation | 2 (4.1) |
| Delirium | 2 (4.1) |
| Other | 9 (18.4) |
| Emergency cardiac surgery | 0 |
| In-hospital death | 0 |
| 30-day follow-up | |
| Major eventse | 12 (7.1) |
| Total readmissions | 8 (4.7) |
| Decompensated HF | 4 (2.4) |
| Major bleeding | 1 (0.6) |
| Major vascular complication | 1 (0.6) |
| Strokef | 2 (1.2) |
| Pacemaker implantationg | 2 (1.2) |
| Total mortality | 0 |
AKIN, Acute Kidney Injury Network; CDO, chronic domiciliary oxygen therapy; COP, cusp overlap projection; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; GFR, glomerular filtration rate; HF, heart failure; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-brain natriuretic peptide; NYHA, New York Heart Association; WP, Wenckebach AV block point.
The incidence of major events in the first 30 days of follow-up was 7.1% (table 1), with a median interval between discharge and event of 14.5 days. An early postprocedure arrhythmic event was experienced by 2 patients, neither of whom had a pre-existing conduction disorder. In both patients, a left bundle branch block developed after implantation of a Portico prosthetic valve (Abbot, United States). The first of these patients (Wenckebach AV block, 110 bpm) experienced a sudden episode of syncope 24hours after discharge, despite 24-hour in-hospital monitoring that did not reveal a high-grade block. Given the high likelihood of paroxysmal AV block, the decision was taken to implant a permanent pacemaker. The second patient (Wenckebach AV block, 110 bpm) attended for new-onset atrial fibrillation with a rapid ventricular response 24hours after discharge; this patient had also been monitored for 48h. After intravenous administration of amiodarone, the patient developed a full AV block, and a pacemaker was implanted.
These findings are similar to those of another study reporting very early discharge of more than 25% of patients.1 Another study showed reductions in hospitalization times to below 48hours in almost 90% of elective patients without complications during the TAVI procedure. As in our sample, all of these patients were closely monitored in the recovery room after implantation, and the postprocedure protocol included rapid rehabilitation, patient and family-member training, and close follow-up after hospital discharge.3
The low event rate during follow-up in our sample reflects the safety of our approach. The overall readmission rate was 4.7%, and the readmission rate for cardiovascular causes was 2.4%. These figures are lower than those reported by other groups, ranging from 6% to 10% and 4% to 6%, respectively; the complication rate during follow-up was also low and was similar to that found in other reports.1–3,5
This study demonstrates that early discharge of patients after minimally invasive TAVI mostly with self-expanding valve prostheses is both feasible and safe, allowing reductions in hospitalization times with a low rate of postprocedure events.
FUNDINGThis study did not receive funding. M. Tamargo holds a Río Hortega grant from the Instituto de Salud Carlos III (2020).
AUTHORS’ CONTRIBUTIONSThe corresponding author guarantees that all the authors made notable contributions to the study design; the acquisition, analysis, and interpretation of results; and manuscript writing or revision. All the authors approved the final version of the manuscript.
CONFLICTS OF INTERESTThere are no conflicts of interest to declare.